- Lymphoid system
-
Lymphoid System 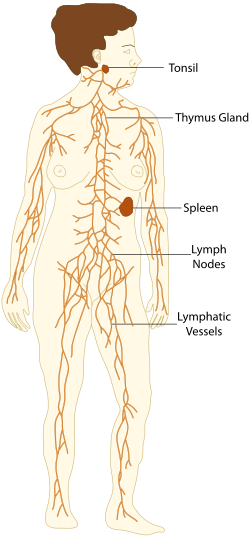
An image displaying the lymphoid system. Latin systema lymphoideum The lymphoid system is the part of the immune system comprising a network of conduits called lymphatic vessels that carry a clear fluid called lymph (from Latin lympha "water"[1]) unidirectionally toward the heart. Lymphoid tissue is found in many organs, particularly the lymph nodes, and in the lymphoid follicles associated with the digestive system such as the tonsils. The system also includes all the structures dedicated to the circulation and production of lymphocytes, which includes the spleen, thymus, bone marrow and the lymphoid tissue associated with the digestive system.[2] The lymphatic system as we know it today was first described independently by Olaus Rudbeck and Thomas Bartholin.
The blood does not directly come in contact with the parenchymal cells and tissues in the body, but constituents of the blood first exit the microvascular exchange blood vessels to become interstitial fluid, which comes into contact with the parenchymal cells of the body. Lymph is the fluid that is formed when interstitial fluid enters the initial lymphatic vessels of the lymphatic system. The lymph is then moved along the lymphatic vessel network by either intrinsic contractions of the lymphatic passages or by extrinsic compression of the lymphatic vessels via external tissue forces (e.g. the contractions of skeletal muscles). Eventually, the lymph vessels empty into the lymphatic ducts, which drain into one of the two subclavian veins (near the junctions of the subclavian veins with the internal jugular veins).
Contents
Functions
The lymphoid system has multiple interrelated functions:[3]
- it is responsible for the removal of interstitial fluid from tissues
- it absorbs and transports fatty acids and fats as chyle from the digestive system
- it transports white blood cells to and from the lymph nodes into the bones
- The lymph transports antigen-presenting cells (APCs), such as dendritic cells, to the lymph nodes where an immune response is stimulated.
Lymphatic tissue is a specialized connective tissue - reticular connective, that contains large quantities of lymphocytes.
Clinical significance
The study of lymphatic drainage of various organs is important in diagnosis, prognosis, and treatment of cancer. The lymphatic system, because of its physical proximity to many tissues of the body, is responsible for carrying cancerous cells between the various parts of the body in a process called metastasis. The intervening lymph nodes can trap the cancer cells. If they are not successful in destroying the cancer cells the nodes may become sites of secondary tumors.
Organization
The lymphoid system can be broadly divided into the conducting system and the lymphoid tissue.
- The conducting system carries the lymph and consists of tubular vessels that include the lymph capillaries, the lymph vessels, and the right and left thoracic ducts.
- The lymphoid tissue is primarily involved in immune responses and consists of lymphocytes[4] and other white blood cells enmeshed in connective tissue through which the lymph passes. Regions of the lymphoid tissue that are densely packed with lymphocytes are known as lymphoid follicles. Lymphoid tissue can either be structurally well organized as lymph nodes or may consist of loosely organized lymphoid follicles known as the mucosa-associated lymphoid tissue (MALT)
Lymphoid tissue
Lymphoid tissue associated with the lymphatic system is concerned with immune functions in defending the body against the infections and spread of tumors. It consists of connective tissue with various types of white blood cells enmeshed in it, most numerous being the lymphocytes.
The lymphoid tissue may be primary, secondary, or tertiary depending upon the stage of lymphocyte development and maturation it is involved in. (The tertiary lymphoid tissue typically contains far fewer lymphocytes, and assumes an immune role only when challenged with antigens that result in inflammation. It achieves this by importing the lymphocytes from blood and lymph.[5])
Primary lymphoid organs
The central or primary lymphoid organs generate lymphocytes from immature progenitor cells.
The thymus and the bone marrow constitute the primary lymphoid tissues involved in the production and early selection of lymphocytes.
Secondary lymphoid organs
Secondary or peripheral lymphoid organs maintain mature naive lymphocytes and initiate an adaptive immune response. The peripheral lymphoid organs are the sites of lymphocyte activation by antigen. Activation leads to clonal expansion and affinity maturation. Mature lymphocytes recirculate between the blood and the peripheral lymphoid organs until they encounter their specific antigen.
Secondary lymphoid tissue provides the environment for the foreign or altered native molecules (antigens) to interact with the lymphocytes. It is exemplified by the lymph nodes, and the lymphoid follicles in tonsils, Peyer's patches, spleen, adenoids, skin, etc. that are associated with the mucosa-associated lymphoid tissue (MALT).
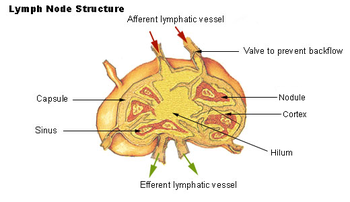
Lymph nodes
A lymph node is an organized collection of lymphoid tissue, through which the lymph passes on its way to returning to the blood. Lymph nodes are located at intervals along the lymphatic system. Several afferent lymph vessels bring in lymph, which percolates through the substance of the lymph node, and is drained out by an efferent lymph vessel.
The substance of a lymph node consists of lymphoid follicles in the outer portion called the "cortex", which contains the lymphoid follicles, and an inner portion called "medulla", which is surrounded by the cortex on all sides except for a portion known as the "hilum". The hilum presents as a depression on the surface of the lymph node, which makes the otherwise spherical or ovoid lymph node bean-shaped. The efferent lymph vessel directly emerges from the lymph node here. The arteries and veins supplying the lymph node with blood enter and exit through the hilum.
Lymph follicles are a dense collection of lymphocytes, the number, size and configuration of which change in accordance with the functional state of the lymph node. For example, the follicles expand significantly upon encountering a foreign antigen. The selection of B cells occurs in the germinal center of the lymph nodes.
Lymph nodes are particularly numerous in the mediastinum in the chest, neck, pelvis, axilla (armpit), inguinal (groin) region, and in association with the blood vessels of the intestines.[2]
Lymphatics
Tubular vessels transport back lymph to the blood ultimately replacing the volume lost from the blood during the formation of the interstitial fluid. These channels are the lymphatic channels or simply called lymphatics.[6]
Function of the fatty acid transport system
Lymph vessels called lacteals are present in the lining of the gastrointestinal tract, predominantly in the small intestine. While most other nutrients absorbed by the small intestine are passed on to the portal venous system to drain via the portal vein into the liver for processing, fats (lipids) are passed on to the lymphatic system to be transported to the blood circulation via the thoracic duct. (There are exceptions, for example medium-chain triglycerides (MCTs) are fatty acid esters of glycerol that passively diffuse from the GI tract to the portal system.) The enriched lymph originating in the lymphatics of the small intestine is called chyle. As the blood circulates, fluid leaks out into the body tissues. This fluid is important because it carries food to the cells and waste back to the bloodstream. The nutrients that are released to the circulatory system are processed by the liver, having passed through the systemic circulation. The lymph system is a one-way system, transporting interstitial fluid back to blood.
Diseases of the lymphatic system
Lymphedema is the swelling caused by the accumulation of lymph fluid,[7] which may occur if the lymphatic system is damaged or has malformations. It usually affects the limbs, though face, neck and abdomen may also be affected.
Some common causes of swollen lymph nodes include infections, infectious mononucleosis, and cancer, e.g. Hodgkin's and non-Hodgkin lymphoma, and metastasis of cancerous cells via the lymphatic system.
Lymphangiomatosis is a disease involving multiple cysts or lesions formed from lymphatic vessels.
In elephantiasis, infection of the lymphatic vessels cause a thickening of the skin and enlargement of underlying tissues, especially in the legs and genitals. It is most commonly caused by a parasitic disease known as lymphatic filariasis. Lymphangiosarcoma is a malignant soft tissue tumor, whereas lymphangioma is a benign tumor occurring frequently in association with Turner syndrome. Lymphangioleiomyomatosis is a benign tumor of the smooth muscles of the lymphatics that occurs in the lungs.
Development of lymphatic tissue
Lymphatic tissues begin to develop by the end of the fifth week of embryonic development. Lymphatic vessels develop from lymph sacs that arise from developing veins, which are derived from mesoderm.
The first lymph sacs to appear are the paired jugular lymph sacs at the junction of the internal jugular and subclavian veins. From the jugular lymph sacs, lymphatic capillary plexuses spread to the thorax, upper limbs, neck and head. Some of the plexuses enlarge and form lymphatic vessels in their respective regions. Each jugular lymph sac retains at least one connection with its jugular vein, the left one developing into the superior portion of the thoracic duct.
The next lymph sac to appear is the unpaired retroperitoneal lymph sac at the root of the mesentery of the intestine. It develops from the primitive vena cava and mesonephric veins. Capillary plexuses and lymphatic vessels spread from the retroperitoneal lymph sac to the abdominal viscera and diaphragm. The sac establishes connections with the cisterna chyli but loses its connections with neighboring veins.
The last of the lymph sacs, the paired posterior lymph sacs, develop from the iliac veins. The posterior lymph sacs produce capillary plexuses and lymphatic vessels of the abdominal wall, pelvic region, and lower limbs. The posterior lymph sacs join the cisterna chyli and lose their connections with adjacent veins.
With the exception of the anterior part of the sac from which the cisterna chyli develops, all lymph sacs become invaded by mesenchymal cells and are converted into groups of lymph nodes.
The spleen develops from mesenchymal cells between layers of the dorsal mesentery of the stomach. The thymus arises as an outgrowth of the third pharyngeal pouch.
Lymphatico-Venous Communications
Present research has found cues about a lymphatico-venous communication. In mammals, lymphatico-venous communications other than those at the base of the neck are not easy to demonstrate, but described in some experiments.[8]
The specialists observed that the pulmonary complications following lymphangiography (a test which utilizes X ray technology, along with the injection of a contrast agent, to view lymphatic circulation and lymph nodes for diagnostic purposes)are more often severe in patients with lymphatic obstruction. In these cases, the contrast medium is thought to reach the vascular system via lymphovenous communications with shunt the material directly into the venous stream, bypassing those lymph nodes distal to the communications,[9] Because less contrast agent is absorbed in lymph nodes, a greater portion of the injected volume passes into the vascular system. Since pulmonary complications are related to the amount of medium reaching the lungs area, the early recognition of lymphovenous communications is a great significance to the lymphangiographer.[9] Another "hint" in proving a lymph-vein communication is offered by a Robert F Dunn experiment. The passage of radioactively tagged tracers, injected at elevated pressure, through the lymph node-venous communications coincides with the increased pressures of injection and subsequent nodal palpation in dogs. The passage of iodinated I 125 serum albumen (ISA) indicates that direct lymph node-venous communications are present, whereas passage of nucleated erythrocytes requires a communication structure the size of a capillary or larger.[10] Moreover, the evidence suggest that in mammals under normal conditions, mostly of the lymph is returned to the blood stream through the lymphatico-venous communications at the base of the neck. When the thoracic duct-venous communication is blocked, however, the resultant raised intralymphatic pressure will usually cause other normal non-functioning communications to open and thereby allow the return of lymph to the blood stream.[8]
History
Hippocrates was one of the first persons to mention the lymphatic system in 5th century BC. In his work "On Joints," he briefly mentioned the lymph nodes in one sentence. Rufus of Ephesus, a Roman physician, identified the axillary, inguinal and mesenteric lymph nodes as well as the thymus during the 1st to 2nd century AD.[11] The first mention of lymphatic vessels was in 3rd century BC by Herophilos, a Greek anatomist living in Alexandria, who incorrectly concluded that the "absorptive veins of the lymphatics", by which he meant the lacteals (lymph vessels of the intestines), drained into the hepatic portal veins, and thus into the liver.[11] Findings of Ruphus and Herophilos findings were further propagated by the Greek physician Galen, who described the lacteals and mesenteric lymph nodes which he observed in his dissection of apes and pigs in the 2nd century AD.[11][12]
Until the 17th century, ideas of Galen were most prevalent. Accordingly, it was believed that the blood was produced by the liver from chyle contaminated with ailments by the intestine and stomach, to which various spirits were added by other organs, and that this blood was consumed by all the organs of the body. This theory required that the blood be consumed and produced many times over. His ideas had remained unchallenged until the 17th century, and even then were defended by some physicians.[12]
In the mid 16th century Gabriele Falloppio (discoverer of the fallopian tubes) described what are now known as the lacteals as "coursing over the intestines full of yellow matter."[11] In about 1563 Bartolomeo Eustachi, a professor of anatomy, described the thoracic duct in horses as vena alba thoracis.[11] The next breakthrough came when in 1622 a physician, Gaspare Aselli, identified lymphatic vessels of the intestines in dogs and termed them venae alba et lacteae, which is now known as simply the lacteals. The lacteals were termed the fourth kind of vessels (the other three being the artery, vein and nerve, which was then believed to be a type of vessel), and disproved Galen's assertion that chyle was carried by the veins. But, he still believed that the lacteals carried the chyle to the liver (as taught by Galen).[13] He also identified the thoracic duct but failed to notice its connection with the lacteals.[11] This connection was established by Jean Pecquet in 1651, who found a white fluid mixing with blood in a dog's heart. He suspected that fluid to be chyle as its flow increased when abdominal pressure was applied. He traced this fluid to the thoracic duct, which he then followed to a chyle-filled sac he called the chyli receptaculum, which is now known as the cisternae chyli; further investigations led him to find that lacteals' contents enter the venous system via the thoracic duct.[11][13] Thus, it was proven convincingly that the lacteals did not terminate in the liver, thus disproving Galen's second idea: that the chyle flowed to the liver.[13] Johann Veslingius drew the earliest sketches of the lacteals in humans in 1647.[12]
The idea that blood recirculates through the body rather than being produced anew by the liver and the heart was first accepted as a result of works of William Harvey—a work he published in 1628. In 1652, Olaus Rudbeck (1630–1702), a Swede, discovered certain transparent vessels in the liver that contained clear fluid (and not white), and thus named them hepatico-aqueous vessels. He also learned that they emptied into the thoracic duct, and that they had valves.[13] He announced his findings in the court of Queen Christina of Sweden, but did not publish his findings for a year,[14] and in the interim similar findings were published by Thomas Bartholin, who additionally published that such vessels are present everywhere in the body, and not just the liver. He is also the one to have named them "lymphatic vessels".[13] This had resulted in a bitter dispute between one of Bartholin's pupils, Martin Bogdan,[15] and Rudbeck, whom he accused of plagiarism.[14]
See also
- American Society of Lymphology
- Lymphangiogenesis
- Manual lymphatic drainage
- Reticuloendothelial system
References
- ^ "Lymph - Definition and More from the Free Merriam-Webster Dictionary". www.merriam-webster.com. http://www.merriam-webster.com/dictionary/lymph. Retrieved 2010-05-29.
- ^ a b Warwick, Roger; Peter L. Williams. "Angiology (Chapter 6)". Gray's anatomy. illustrated by Richard E. M. Moore (Thirty-fifth ed.). London: Longman. pp. 588–785.
- ^ "The functions of the Lymphatic System.". http://www.lymphnotes.com/article.php/id/151/. Retrieved Feb. 25, 2011.
- ^ "lymphoid tissue" at Dorland's Medical Dictionary
- ^ Goldsby, Richard; Kindt, TJ; Osborne, BA; Janis Kuby (2003) [1992]. "Cells and Organs of the Immune System (Chapter 2)". Immunology (Fifth ed.). New York: W. H. Freeman and Company. pp. 24–56. ISBN 07167-4947-5.
- ^ "Definition of lymphatics". Webster's New World Medical Dictionary. medicineNet.com. http://www.medterms.com/script/main/art.asp?articlekey=4217. Retrieved 2008-07-06.
- ^ "Lymphedema". http://www.merck.com/mmhe/sec03/ch037/ch037b.html.
- ^ a b Schwartz, Colin; Werthessen, N, Wolf, S (1981) [1931]. "The Lymphatic Circulation". Structure and Function of Circulation, vol 2 (Fifth ed.). New York: Plenum Press. pp. 502–503.
- ^ a b Farrel, Walter (October 1966). Lymphangiographic Demonstration of Lymphovenous Communication After Radiotherapy in Hodgkin's Disease,. Journal of radiological Society of North America. http://www.radiology.rsna.org/content/87/4/630.extract/. Retrieved 23 April 2011.
- ^ Robert F Dunn; Ronald W Strahan, Paul H Ward (1973). "Lymph Node-Venous Communications". Lymph Node-Venous Communication. Arch Otolaringology. http://www.archotol.ama-assn.org/cgi/content/abstract/97/6/461. Retrieved 23 April 2011.
- ^ a b c d e f g Ambrose, C. (2006). "Immunology’s first priority dispute—An account of the 17th-century Rudbeck–Bartholin feud". Cellular Immunology 242 (1): 1. doi:10.1016/j.cellimm.2006.09.004. PMID 17083923.
- ^ a b c Fanous, Medhat YZ; Anthony J Phillips, John A Windsor (2007). "Mesenteric Lymph: The Bridge to Future Management of Critical Illness". Journal of the Pancreas (Department of Internal Medicine and Gastroenterology ALMA MATER STUDIORUM - UNIVERSITY OF BOLOGNA) 8 (4): 374–399. PMID 17625290. http://www.joplink.net/prev/200707/06.html. Retrieved 2008-07-11.
- ^ a b c d e Flourens, P. (1859). "ASELLI, PECQUET, RUDBECK, BARTHOLIN (Chapter 3)". A History of the Discovery of the Circulation of the Blood. Rickey, Mallory & company. pp. 67–99. http://books.google.com/?id=4QqS6LrYWf4C&printsec=frontcover&dq=william+harvey. Retrieved 2008-07-11.
- ^ a b Eriksson, G. (2004). "Olaus Rudbeck as scientist and professor of medicine (Original article in Swedish)" (in Swedish). Svensk Medicinhistorisk Tidskrift 8 (1): 39–44. PMID 16025602.
- ^ "Disputatio anatomica, de circulatione sanguinis". Account of Rudbeck's work on lymphatic system and dispute with Bartholin. The International League of Antiquarian Booksellers. http://www.ilab.org/db/detail.php?booknr=349906004. Retrieved 2008-07-11.[dead link]
External links
- Lymphatic System
- Lymphatic System Overview (innerbody.com)
Human systems and organs TA 2–4:
MSBone (Carpus · Collar bone (clavicle) · Thigh bone (femur) · Fibula · Humerus · Mandible · Metacarpus · Metatarsus · Ossicles · Patella · Phalanges · Radius · Skull (cranium) · Tarsus · Tibia · Ulna · Rib · Vertebra · Pelvis · Sternum) · CartilageTA 5–11:
splanchnic/
viscusMouth (Salivary gland, Tongue) · upper GI (Oropharynx, Laryngopharynx, Esophagus, Stomach) · lower GI (Small intestine, Appendix, Colon, Rectum, Anus) · accessory (Liver, Biliary tract, Pancreas)TA 12–16 Blood
(Non-TA)General anatomy: systems and organs, regional anatomy, planes and lines, superficial axial anatomy, superficial anatomy of limbsLymphatic system - Lymphatic trunks and ducts (TA A12.4.01, GA 8.690) Path details ... Blood → Interstitial fluid → Lymph →
Lymph capillary → Afferent lymph vessel (Lymphatic vessel) → Lymph node → Efferent lymph vessel (Lymphatic vessel) →
Lymph trunk (Subclavian lymph trunk • Jugular lymph trunk • Bronchomediastinal lymph trunk • Intestinal lymph trunk → Cisterna chyli • Lumbar lymph trunk → Cisterna chyli) → Lymph duct {Right lymphatic duct and Thoracic duct (left side)} →
Subclavian vein (right and left) → Blood ...Other concepts M: LMO
anat(h, u, t, a, l)/phys/depv
noco/cong/tumr
proc
Lymphoid system (TA A13.1–2, TH H3.10, GA 8 and 9) Primary lymphoid organs Secondary lymphoid organs structural: Hilum · Trabeculae · Diaphragmatic surface of spleen · Visceral surface of spleen
Red pulp (Cords of Billroth, Marginal zone)
White pulp (Periarteriolar lymphoid sheaths, Germinal center)
blood flow: Trabecular arteries · Trabecular veinslymph flow: Afferent lymph vessels · Cortical sinuses · Medullary sinuses · Efferent lymph vessels
T cells: High endothelial venules
B cells: Primary follicle/Germinal center · Mantle zone · Marginal zone
layers: Capsule/Trabeculae · Subcapsular sinus · Cortex · Paracortex · Medulla (Medullary cord) · HilumM: LMO
anat(h, u, t, a, l)/phys/depv
noco/cong/tumr
proc
Lymphatics of head and neck (TA A13.3.00, GA 8.692) Head PosteriorAnteriorNeck/Cervical Superficial cervical: Superficial anterior cervical · Superficial lateral cervical
Deep cervical: Deep anterior cervical (Pretracheal, Paratracheal, Prelaryngeal, Thyroid) · Deep lateral cervical (Superior deep cervical, Inferior deep cervical, Retropharyngeal, Jugulodigastric, Jugulo-omohyoid)
Anterior cervical · Lateral cervical
Supraclavicular (Virchow's)
Jugular trunkM: LMO
anat(h, u, t, a, l)/phys/depv
noco/cong/tumr
proc
Lymphatics of upper limbs (TA A13.3.01, GA 8.699) Axillary Other M: LMO
anat(h, u, t, a, l)/phys/depv
noco/cong/tumr
proc
Chest parietal: Parasternal · Intercostal · Superior diaphragmatic
visceral: Tracheobronchial (Superior tracheobronchial nodes · Inferior tracheobronchial nodes · Bronchopulmonary nodes · Paratracheal lymph nodes, Intrapulmonary nodes)
Right lymphatic duct · Thoracic duct · Bronchomediastinal lymph trunkM: LMO
anat(h, u, t, a, l)/phys/depv
noco/cong/tumr
proc
Lymphatics of abdomen (TA A13.3.03–04, GA 8.703) Abdomen Parietal/
Lumbar trunkOtherPelvic M: LMO
anat(h, u, t, a, l)/phys/depv
noco/cong/tumr
proc
Lymphatics of lower limbs (TA A13.3.05, GA 8.701) Inguinal Other M: LMO
anat(h, u, t, a, l)/phys/depv
noco/cong/tumr
proc
Categories:
Wikimedia Foundation. 2010.