- Herbalism
-
Alternative medical systems Acupuncture · Anthroposophic medicine · Ayurveda · Chiropractic · Herbalism · Homeopathy · Naturopathy · Qigong · Siddha medicine · Traditional medicine
(Chinese · Mongolian · Tibetan) · UnaniNCCAM classifications Whole medical systems · Mind-body interventions · Biologically based therapies · Manipulative therapy · Energy therapies See also Alternative medicine · Glossary · People Herbalism is a traditional medicinal or folk medicine practice based on the use of plants and plant extracts. Herbalism is also known as botanical medicine, medical herbalism, herbal medicine, herbology, herblore, and phytotherapy. The scope of herbal medicine is sometimes extended to include fungal and bee products, as well as minerals, shells and certain animal parts.[1] Pharmacognosy is the study of medicines derived from natural sources.
Traditional use of medicines is recognized as a way to learn about potential future medicines. In 2001, researchers identified 122 compounds used in mainstream medicine which were derived from "ethnomedical" plant sources; 80% of these compounds were used in the same or related manner as the traditional ethnomedical use.[2]
Plants have evolved the ability to synthesize chemical compounds that help them defend against attack from a wide variety of predators such as insects, fungi and herbivorous mammals. By chance, some of these compounds, whilst being toxic to plant predators, turn out to have beneficial effects when used to treat human diseases. Such secondary metabolites are highly varied in structure, many are aromatic substances, most of which are phenols or their oxygen-substituted derivatives. At least 12,000 have been isolated so far; a number estimated to be less than 10% of the total. Chemical compounds in plants mediate their effects on the human body by binding to receptor molecules present in the body; such processes are identical to those already well understood for conventional drugs and as such herbal medicines do not differ greatly from conventional drugs in terms of how they work. This enables herbal medicines to be in principle just as effective as conventional medicines but also gives them the same potential to cause harmful side effects. Many of the herbs and spices used by humans to season food yield useful medicinal compounds.[3][4]
Similarly to prescription drugs, a number of herbs are thought to be likely to cause adverse effects.[5] Furthermore, "adulteration, inappropriate formulation, or lack of understanding of plant and drug interactions have led to adverse reactions that are sometimes life threatening or lethal.[6]
Anthropology of herbalism
People on all continents have used hundreds to thousands of indigenous plants for treatment of ailments since prehistoric times. Medicinal herbs were found in the personal effects of Ötzi the Iceman, whose body was frozen in the Ötztal Alps for more than 5,300 years. These herbs appear to have been used to treat the parasites found in his intestines. Anthropologists theorize that animals evolved a tendency to seek out bitter plant parts in response to illness[citation needed].
Indigenous healers often claim to have learned by observing that sick animals change their food preferences to nibble at bitter herbs they would normally reject.[7] Field biologists have provided corroborating evidence based on observation of diverse species, such as chimpanzees, chickens, sheep and butterflies. Lowland gorillas take 90% of their diet from the fruits of Aframomum melegueta, a relative of the ginger plant, that is a potent antimicrobial and apparently keeps shigellosis and similar infections at bay.[8] Current research focuses on the possibility that this plants also protects gorillas from fibrosing cardiomyopathy which has a devastating effect on captive animals.[9]
Researchers from Ohio Wesleyan University found that some birds select nesting material rich in antimicrobial agents which protect their young from harmful bacteria.[10]
Sick animals tend to forage plants rich in secondary metabolites, such as tannins and alkaloids.[11] Since these phytochemicals often have antiviral, antibacterial, antifungal and antihelminthic properties, a plausible case can be made for self-medication by animals in the wild.[8]
Some animals have digestive systems especially adapted to cope with certain plant toxins. For example, the koala can live on the leaves and shoots of the eucalyptus, a plant that is dangerous to most animals.[12] A plant that is harmless to a particular animal may not be safe for humans to ingest.[13] A reasonable conjecture is that these discoveries were traditionally collected by the medicine men of indigenous tribes, who then passed on safety information and cautions.
The use of herbs and spices in cuisine developed in part as a response to the threat of food-borne pathogens. Studies show that in tropical climates where pathogens are the most abundant, recipes are the most highly spiced. Further, the spices with the most potent antimicrobial activity tend to be selected.[14] In all cultures vegetables are spiced less than meat, presumably because they are more resistant to spoilage.[15]
History
 Borage from Project Gutenberg EBook of Culinary Herbs: Their Cultivation Harvesting Curing and Uses, by M. G. Kains
Borage from Project Gutenberg EBook of Culinary Herbs: Their Cultivation Harvesting Curing and Uses, by M. G. Kains
The use of plants as medicines predates written human history. A 60 000-year-old Neanderthal burial site, "Shanidar IV", in northern Iraq has yielded large amounts of pollen from 8 plant species, 7 of which are used now as herbal remedies.[16]
In the written record, the study of herbs dates back over 5,000 years to the Sumerians, who described well-established medicinal uses for such plants as laurel, caraway, and thyme. Ancient Egyptian medicine of 1000 BC are known to have used garlic, opium, castor oil, coriander, mint, indigo, and other herbs for medicine and the Old Testament also mentions herb use and cultivation, including mandrake, vetch, caraway, wheat, barley, and rye.
In India, Ayurveda medicine has used many herbs such as turmeric possibly as early as 1900 BC.[17] Many other herbs and minerals used in Ayurveda were later described by ancient Indian herbalists such as Charaka and Sushruta during the 1st millennium BC. The Sushruta Samhita attributed to Sushruta in the 6th century BC describes 700 medicinal plants, 64 preparations from mineral sources, and 57 preparations based on animal sources.[18]
The first Chinese herbal book, the Shennong Bencao Jing, compiled during the Han Dynasty but dating back to a much earlier date, possibly 2700 BC,[citation needed] lists 365 medicinal plants and their uses - including ma-Huang, the shrub that introduced the drug ephedrine to modern medicine. Succeeding generations augmented on the Shennong Bencao Jing, as in the Yaoxing Lun (Treatise on the Nature of Medicinal Herbs), a 7th century Tang Dynasty treatise on herbal medicine.
The ancient Greeks and Romans made medicinal use of plants. Greek and Roman medicinal practices, as preserved in the writings of Hippocrates and - especially - Galen, provided the pattern for later western medicine. Hippocrates advocated the use of a few simple herbal drugs - along with fresh air, rest, and proper diet. Galen, on the other hand, recommended large doses of drug mixtures - including plant, animal, and mineral ingredients. The Greek physician compiled the first European treatise on the properties and uses of medicinal plants, De Materia Medica. In the first century AD, Dioscorides wrote a compendium of more than 500 plants that remained an authoritative reference into the 17th century. Similarly important for herbalists and botanists of later centuries was the Greek book that founded the science of botany, Theophrastus' Historia Plantarum, written in the fourth century BC.
Middle Ages
The uses of plants for medicine and other purposes changed little in early medieval Europe. Many Greek and Roman writings on medicine, as on other subjects, were preserved by hand copying of manuscripts in monasteries. The monasteries thus tended to become local centers of medical knowledge, and their herb gardens provided the raw materials for simple treatment of common disorders. At the same time, folk medicine in the home and village continued uninterrupted, supporting numerous wandering and settled herbalists. Among these were the "wise-women", who prescribed herbal remedies often along with spells and enchantments. It was not until the late Middle Ages that women who were knowledgeable in herb lore became the targets of the witch hysteria. One of the most famous women in the herbal tradition was Hildegard of Bingen. A twelfth century Benedictine nun, she wrote a medical text called Causes and Cures.
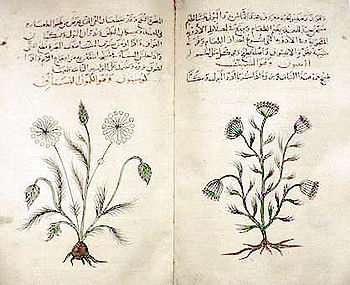
Medical schools known as Bimaristan began to appear from the 9th century in the medieval Islamic world among Persians and Arabs, which was generally more advanced than medieval Europe at the time. The Arabs venerated Greco-Roman culture and learning, and translated tens of thousands of texts into Arabic for further study.[19] As a trading culture, the Arab travellers had access to plant material from distant places such as China and India. Herbals, medical texts and translations of the classics of antiquity filtered in from east and west.[20] Muslim botanists and Muslim physicians significantly expanded on the earlier knowledge of materia medica. For example, al-Dinawari described more than 637 plant drugs in the 9th century,[21] and Ibn al-Baitar described more than 1,400 different plants, foods and drugs, over 300 of which were his own original discoveries, in the 13th century.[22] The experimental scientific method was introduced into the field of materia medica in the 13th century by the Andalusian-Arab botanist Abu al-Abbas al-Nabati, the teacher of Ibn al-Baitar. Al-Nabati introduced empirical techniques in the testing, description and identification of numerous materia medica, and he separated unverified reports from those supported by actual tests and observations. This allowed the study of materia medica to evolve into the science of pharmacology.[23]
Avicenna's The Canon of Medicine (1025) lists 800 tested drugs, plants and minerals.[24] Book Two is devoted to a discussion of the healing properties of herbs, including nutmeg, senna, sandalwood, rhubarb, myrrh, cinammon, and rosewater.[19] Baghdad was an important center for Arab herbalism, as was Al-Andalus between 800 and 1400. Abulcasis (936-1013) of Cordoba authored The Book of Simples, an important source for later European herbals, while Ibn al-Baitar (1197–1248) of Malaga authored the Corpus of Simples, the most complete Arab herbal which introduced 200 new healing herbs, including tamarind, aconite, and nux vomica.[19][25] Other pharmacopoeia books include that written by Abu-Rayhan Biruni in the 11th century[citation needed] and Ibn Zuhr (Avenzoar) in the 12th century (and printed in 1491),[26] The origins of clinical pharmacology also date back to the Middle Ages in Avicenna's The Canon of Medicine, Peter of Spain's Commentary on Isaac, and John of St Amand's Commentary on the Antedotary of Nicholas.[27] In particular, the Canon introduced clinical trials,[28] randomized controlled trials,[29][30] and efficacy tests.[31][32]
Alongside the university system, folk medicine continued to thrive. The continuing importance of herbs for the centuries following the Middle Ages is indicated by the hundreds of herbals published after the invention of printing in the fifteenth century. Theophrastus’ Historia Plantarum was one of the first books to be printed, but Dioscorides’ De Materia Medica, Avicenna's Canon of Medicine and Avenzoar's pharmacopoeia were not far behind.
 Marjoram from Project Gutenberg EBook of Culinary Herbs: Their Cultivation Harvesting Curing and Uses, by M. G. Kains
Marjoram from Project Gutenberg EBook of Culinary Herbs: Their Cultivation Harvesting Curing and Uses, by M. G. Kains
Modern era
The fifteenth, sixteenth, and seventeenth centuries were the great age of herbals, many of them available for the first time in English and other languages rather than Latin or Greek. The first herbal to be published in English was the anonymous Grete Herball of 1526. The two best-known herbals in English were The Herball or General History of Plants (1597) by John Gerard and The English Physician Enlarged (1653) by Nicholas Culpeper. Gerard’s text was basically a pirated translation of a book by the Belgian herbalist Dodoens and his illustrations came from a German botanical work. The original edition contained many errors due to faulty matching of the two parts. Culpeper’s blend of traditional medicine with astrology, magic, and folklore was ridiculed by the physicians of his day yet his book - like Gerard’s and other herbals - enjoyed phenomenal popularity. The Age of Exploration and the Columbian Exchange introduced new medicinal plants to Europe. The Badianus Manuscript was an illustrated Aztec herbal translated into Latin in the 16th century.
The second millennium, however, also saw the beginning of a slow erosion of the pre-eminent position held by plants as sources of therapeutic effects. This began with the Black Death, which the then dominant Four Element medical system proved powerless to stop. A century later, Paracelsus introduced the use of active chemical drugs (like arsenic, copper sulfate, iron, mercury, and sulfur). These were accepted even though they had toxic effects because of the urgent need to treat Syphilis. The rapid development of chemistry and the other physical sciences, led increasingly to the dominance of chemotherapy - chemical medicine - as the orthodox system of the twentieth century.
Role in modern human society
 Botánicas, such as this one in Jamaica Plain, Massachusetts, cater to the Latino community and sell herbal cures and folk medicine alongside statues of saints, candles decorated with prayers, lucky bamboo, and other items.
Botánicas, such as this one in Jamaica Plain, Massachusetts, cater to the Latino community and sell herbal cures and folk medicine alongside statues of saints, candles decorated with prayers, lucky bamboo, and other items.
The use of herbs to treat disease is almost universal among non-industrialized societies.[33] A number of traditions came to dominate the practice of herbal medicine at the end of the twentieth century:
- The "classical" herbal medicine system, based on Greek and Roman sources
- The Siddha and Ayurvedic medicine systems from various South Asian Countries
- Chinese herbal medicine (Chinese herbology) 中药 (zhōngyào)
- Traditional African medicine
- Unani-Tibb medicine
- Shamanic herbalism: a catch-all phrase for information mostly supplied from South America and the Himalayas
- Native American medicine.
Many of the pharmaceuticals currently available to physicians have a long history of use as herbal remedies, including opium, aspirin, digitalis, and quinine. The World Health Organization (WHO) estimates that 80 percent of the world's population presently uses herbal medicine for some aspect of primary health care.[34] Pharmaceuticals are prohibitively expensive for most of the world's population, half of which lives on less than $2 U.S. per day.[33] In comparison, herbal medicines can be grown from seed or gathered from nature for little or no cost.
In addition to the use in the developing world, herbal medicine is used in industrialized nations by alternative medicine practitioners such as naturopaths. A 1998 survey of herbalists in the UK found that many of the herbs recommended by them were used traditionally but had not been evaluated in clinical trials.[35] In Australia, a 2007 survey found that these Western herbalists tend to prescribe liquid herbal combinations of herbs rather than tablets of single herbs.[36]
The use of, and search for, drugs and dietary supplements derived from plants have accelerated in recent years. Pharmacologists, microbiologists, botanists, and natural-products chemists are combing the Earth for phytochemicals and leads that could be developed for treatment of various diseases. In fact, according to the World Health Organisation, approximately 25% of modern drugs used in the United States have been derived from plants.[37]
- Among the 120 active compounds currently isolated from the higher plants and widely used in modern medicine today, 80 percent show a positive correlation between their modern therapeutic use and the traditional use of the plants from which they are derived.[2]
- More than two thirds of the world's plant species - at least 35,000 of which are estimated to have medicinal value - come from the developing countries.[verification needed]
- At least 7,000 medical compounds in the modern pharmacopoeia are derived from plants[38]
Biological background
 The anthocyanins in sweet violets produce deep red, violet and blue shades.
The anthocyanins in sweet violets produce deep red, violet and blue shades.
 The carotenoids in primrose produce bright red, yellow and orange shades.
The carotenoids in primrose produce bright red, yellow and orange shades.
All plants produce chemical compounds as part of their normal metabolic activities. These are divided into primary metabolites, such as sugars and fats, found in all plants, and secondary metabolites, compounds not essential for basic function found in a smaller range of plants, some useful ones found only in a particular genus or species. Pigments harvest light, protect the organism from radiation and display colors to attract pollinators. Many common weeds, such as nettle, dandelion and chickweed, have medicinal properties.[39][40]
The functions of secondary metabolites are varied. For example, some secondary metabolites are toxins used to deter predation, and others are pheromones used to attract insects for pollination. Phytoalexins protect against bacterial and fungal attacks. Allelochemicals inhibit rival plants that are competing for soil and light.
Plants upregulate and downregulate their biochemical paths in response to the local mix of herbivores, pollinators and microorganisms.[41] The chemical profile of a single plant may vary over time as it reacts to changing conditions. It is the secondary metabolites and pigments that can have therapeutic actions in humans and which can be refined to produce drugs.
Plants synthesize a bewildering variety of phytochemicals but most are derivatives of a few biochemical motifs.
- Alkaloids contain a ring with nitrogen. Many alkaloids have dramatic effects on the central nervous system. Caffeine is an alkaloid that provides a mild lift but the alkaloids in datura cause severe intoxication and even death.
- polyphenol, also known as phenolics, contain phenol rings. The anthocyanins that give grapes their purple color, the isoflavones, the phytoestrogens from soy and the tannins that give tea its astringency are phenolics.
- Terpenoids are built up from terpene building blocks. Each terpene consists of two paired isoprenes. The names monoterpenes, sesquiterpenes, diterpenes and triterpenes are based on the number of isoprene units. The fragrance of rose and lavender is due to monoterpenes. The carotenoids produce the reds, yellows and oranges of pumpkin, corn and tomatoes.
- Glycosides consist of a glucose moiety attached to an aglycone. The aglycone is a molecule that is bioactive in its free form but inert until the glycoside bond is broken by water or enzymes. This mechanism allows the plant to defer the availability of the molecule to an appropriate time, similar to a safety lock on a gun. An example is the cyanoglycosides in cherry pits that release toxins only when bitten by a herbivore.
The word drug itself comes from the Dutch word "droog" (via the French word Drogue), which means 'dried plant'. Some examples are inulin from the roots of dahlias, quinine from the cinchona, morphine and codeine from the poppy, and digoxin from the foxglove.
The active ingredient in willow bark, once prescribed by Hippocrates, is salicin, which is converted in the body into salicylic acid. The discovery of salicylic acid would eventually lead to the development of the acetylated form acetylsalicylic acid, also known as "aspirin", when it was isolated from a plant known as meadowsweet. The word aspirin comes from an abbreviation of meadowsweet's Latin genus Spiraea, with an additional "A" at the beginning to acknowledge acetylation, and "in" was added at the end for easier pronunciation.[42] "Aspirin" was originally a brand name, and is still a protected trademark in some countries. This medication was patented by Bayer AG.
Herbal philosophy
Four approaches to the use of plants as medicine include:
1. The magical/shamanic
Almost all non-modern societies recognise this kind of use. The practitioner is regarded as endowed with gifts or powers that allow him/her to use herbs in a way that is hidden from the average person, and the herbs are said to affect the spirit or soul of the person.
2. The energetic
This approach includes the major systems of TCM, Ayurveda, and Unani. Herbs are regarded as having actions in terms of their energies and affecting the energies of the body. The practitioner may have extensive training, and ideally be sensitive to energy, but need not have supernatural powers.
3. The functional dynamic
This approach was used by early physiomedical practitioners, whose doctrine forms the basis of contemporary practice in the UK. Herbs have a functional action, which is not necessarily linked to a physical compound, although often to a physiological function, but there is no explicit recourse to concepts involving energy.
4. The chemical
Modern practitioners - called Phytotherapists - attempt to explain herb actions in terms of their chemical constituents. It is generally assumed that the specific combination of secondary metabolites in the plant are responsible for the activity claimed or demonstrated, a concept called synergy.
Most[weasel words] modern herbalists concede that pharmaceuticals are more effective in emergency situations where time is of the essence. An example would be where a patient had an acute heart attack that posed imminent danger. However they claim that over the long term herbs can help the patient resist disease, and that in addition, they provide nutritional and immunological support that pharmaceuticals lack. They view their goal as prevention as well as cure.
Herbalists tend to use extracts from parts of plants, such as the roots or leaves but not isolate particular phytochemicals.[43] Pharmaceutical medicine prefers single ingredients on the grounds that dosage can be more easily quantified. It is also possible to patent single compounds, and therefore generate income. Herbalists often reject the notion of a single active ingredient, arguing that the different phytochemicals present in many herbs will interact to enhance the therapeutic effects of the herb and dilute toxicity.[44] Furthermore, they argue that a single ingredient may contribute to multiple effects. Herbalists deny that herbal synergism can be duplicated with synthetic chemicals. They argue that phytochemical interactions and trace components may alter the drug response in ways that cannot currently be replicated with a combination of a few putative active ingredients.[45][46] Pharmaceutical researchers recognize the concept of drug synergism but note that clinical trials may be used to investigate the efficacy of a particular herbal preparation, provided the formulation of that herb is consistent.[47]
In specific cases the claims of synergy[48] and multifunctionality[49] have been supported by science. The open question is how widely both can be generalized. Herbalists would argue that cases of synergy can be widely generalized, on the basis of their interpretation of evolutionary history, not necessarily shared by the pharmaceutical community. Plants are subject to similar selection pressures as humans and therefore they must develop resistance to threats such as radiation, reactive oxygen species and microbial attack in order to survive.[50] Optimal chemical defenses have been selected for and have thus developed over millions of years.[51] Human diseases are multifactorial and may be treated by consuming the chemical defences that they believe to be present in herbs. Bacteria, inflammation, nutrition and ROS (reactive oxygen species) may all play a role in arterial disease.[52] Herbalists claim a single herb may simultaneously address several of these factors. Likewise a factor such as ROS may underlie more than one condition.[53] In short herbalists view their field as the study of a web of relationships rather than a quest for single cause and a single cure for a single condition.
In selecting herbal treatments herbalists may use forms of information that are not applicable to pharmacists. Because herbs can moonlight as vegetables, teas or spices they have a huge consumer base and large-scale epidemiological studies become feasible. Ethnobotanical studies are another source of information.[54] For example, when indigenous peoples from geographically dispersed areas use closely related herbs for the same purpose that is taken as supporting evidence for its efficacy.[citation needed] Herbalists contend that historical medical records and herbals are underutilized resources.[55] They favor the use of convergent information in assessing the medical value of plants. An example would be when in-vitro activity is consistent with traditional use.
Popularity
A survey released in May 2004 by the National Center for Complementary and Alternative Medicine focused on who used complementary and alternative medicines (CAM), what was used, and why it was used. The survey was limited to adults, aged 18 years and over during 2002, living in the United States.
According to this survey, herbal therapy, or use of natural products other than vitamins and minerals, was the most commonly used CAM therapy (18.9%) when all use of prayer was excluded.[56][57]
Herbal remedies are very common in Europe. In Germany, herbal medications are dispensed by apothecaries (e.g., Apotheke). Prescription drugs are sold alongside essential oils, herbal extracts, or herbal teas. Herbal remedies are seen by some as a treatment to be preferred to pure medical compounds which have been industrially produced.[58]
In the United Kingdom, the training of medical herbalists is done by state funded Universities. For example, Bachelor of Science degrees in herbal medicine are offered at Universities such as University of East London, Middlesex University, University of Central Lancashire, University of Westminster, University of Lincoln and Napier University in Edinburgh at the present. Avid public interest in herbalism in the UK has been recently confirmed by the popularity of the topic in mainstream media, such as the prime-time hit TV series BBC's Grow Your Own Drugs,which demonstrated how to grow and prepare herbal remedies at home.
In the United States, a Bachelor of Science degree in herbal sciences is offered at Bastyr University, and a Master of Science in herbal medicine is offered at Tai Sophia Institute. There are also many smaller organizations and teachers offering certifications.
A 2004 Cochrane Collaboration review found that herbal therapies are supported by strong evidence but are not widely used in all clinical settings.[59]
Types of herbal medicine systems
Use of medicinal plants can be as informal as, for example, culinary use or consumption of an herbal tea or supplement, although the sale of some herbs considered dangerous is often restricted to the public. Sometimes such herbs are provided to professional herbalists by specialist companies. Many herbalists, both professional and amateur, often grow or "wildcraft" their own herbs.
Some researchers trained in both western and traditional Chinese medicine have attempted to deconstruct ancient medical texts in the light of modern science. One idea is that the yin-yang balance, at least with regard to herbs, corresponds to the pro-oxidant and anti-oxidant balance. This interpretation is supported by several investigations of the ORAC ratings of various yin and yang herbs.[60][61]
In America, early settlers relied on plants imported from Europe, and also from local Indian knowledge. One particularly successful practitioner, Samuel Thomson developed a hugely popular system of medicine. This approach was subsequently broadened to include concepts introduced from modern physiology, a discipline called Physiomedicalism. Another group, the Eclectics, were a later offshoot from the orthodox medical profession, who were looking to avoid the then current medical treatments of mercury and bleeding, and introduced herbal medicine into their practices. Both groups were eventually overcome by the actions of the American Medical Association, which was formed for this purpose. Cherokee medicine tends to divide herbs into foods, medicines and toxins and to use seven plants in the treatment of disease, which is defined with both spiritual and physiological aspects, according to Cherokee herbalist David Winston.[62]
In India, Ayurvedic medicine has quite complex formulas with 30 or more ingredients, including a sizable number of ingredients that have undergone "alchemical processing", chosen to balance "Vata", "Pitta" or "Kapha."[63]
In Tamil Nadu, Tamils have their own medicinal system now popularly called the Siddha medicinal system. The Siddha system is entirely in the Tamil language. It contains roughly 300,000 verses covering diverse aspects of medicine such as anatomy, sex ("kokokam" is the sexual treatise of par excellence), herbal, mineral and metallic compositions to cure many diseases that are relevant even to-day. Ayurveda is in Sanskrit, but Sanskrit was not generally used as a mother tongue and hence its medines are mostly taken from Siddha and other local traditions.[64]
In addition there are more modern theories of herbal combination like William LeSassier's triune formula which combined Pythagorean imagery with Chinese medicine ideas and resulted in 9 herb formulas which supplemented, drained or neutrally nourished the main organ systems affected and three associated systems[citation needed]. His system has been taught to thousands of influential American herbalists through his own apprenticeship programs during his lifetime, the William LeSassier Archive[65] and the David Winston Center for Herbal Studies.[66] Different chemicals in herbs are more abundant than in a single drug. Some chemicals in herbs may work as growth hormones or antibiotics, nutrients, and toxin neutralizers.
Many traditional African remedies have performed well in initial laboratory tests to ensure they are not toxic and in tests on animals. Gawo, a herb used in traditional treatments, has been tested in rats by researchers from Nigeria's University of Jos and the National Institute for Pharmaceutical Research and Development. According to research in the African Journal of Biotechnology, Gawo passed tests for toxicity and reduced induced fevers, diarrhoea and inflammation [67]
Routes of administration
The exact composition of a herbal product is influenced by the method of extraction. A tisane will be rich in polar components because water is a polar solvent. Oil on the other hand is a non-polar solvent and it will absorb non-polar compounds. Alcohol lies somewhere in between. There are many forms in which herbs can be administered, these include:
- Tinctures - Alcoholic extracts of herbs such as Echinacea extract. Usually obtained by combining 100% pure ethanol (or a mixture of 100% ethanol with water) with the herb. A completed tincture has a ethanol percentage of at least 25% (sometimes up to 90%).[68] The term tincture is sometimes applied to preparations using other solvents than ethanol.
- Herbal wine and elixirs - These are alcoholic extract of herbs; usually with an ethanol percentage of 12-38% [68] Herbal wine is a maceration of herbs in wine, while an elixir is a maceration of herbs in spirits (e.g., vodka, grappa, etc.)
- Tisanes - Hot water extracts of herb, such as chamomile.
- Decoctions - Long-term boiled extract of usually roots or bark.
- Macerates - Cold infusion of plants with high mucilage-content as sage, thyme, etc. Plants are chopped and added to cold water. They are then left to stand for 7 to 12 hours (depending on herb used). For most macerates 10 hours is used.[68]
- Vinegars - Prepared at the same way as tinctures, except using a solution of acetic acid as the solvent.
- Topicals:
- Essential oils - Application of essential oil extracts, usually diluted in a carrier oil (many essential oils can burn the skin or are simply too high dose used straight – diluting in olive oil or another food grade oil such as almond oil can allow these to be used safely as a topical).[69]
- Salves, oils, balms, creams and lotions - Most topical applications are oil extractions of herbs. Taking a food grade oil and soaking herbs in it for anywhere from weeks to months allows certain phytochemicals to be extracted into the oil. This oil can then be made into salves, creams, lotions, or simply used as an oil for topical application. Any massage oils, antibacterial salves and wound healing compounds are made this way.
- Poultices and compresses - One can also make a poultice or compress using whole herb (or the appropriate part of the plant) usually crushed or dried and re-hydrated with a small amount of water and then applied directly in a bandage, cloth or just as is.
- Whole herb consumption - This can occur in either dried form (herbal powder), or fresh juice, (fresh leaves and other plant parts).
- Syrups - Extracts of herbs made with syrup or honey. Sixty five parts of sugar are mixed with 35 parts of water and herb. The whole is then boiled and macerated for three weeks.[68]
- Extracts - Include liquid extracts, dry extracts and nebulisates. Liquid extracts are liquids with a lower ethanol percentage than tinctures. They can (and are usually) made by vacuum distilling tinctures. Dry extracts are extracts of plant material which are evaporated into a dry mass. They can then be further refined to a capsule or tablet.[68] A nebulisate is a dry extract created by freeze-drying.
- Inhalation as in aromatherapy can be used as a mood changing treatment[70][71] to fight a sinus infection or cough [72][citation needed], or to cleanse the skin on a deeper level (steam rather than direct inhalation here)[citation needed]
Safety
For partial list of herbs with known adverse effects, see List of herbs with known adverse effects.A number of herbs are thought to be likely to cause adverse effects.[5] Furthermore, "adulteration, inappropriate formulation, or lack of understanding of plant and drug interactions have led to adverse reactions that are sometimes life threatening or lethal.[6]" Proper double-blind clinical trials are needed to determine the safety and efficacy of each plant before they can be recommended for medical use.[73] Although many consumers believe that herbal medicines are safe because they are "natural", herbal medicines and synthetic drugs may interact, causing toxicity to the patient. Herbal remedies can also be dangerously contaminated, and herbal medicines without established efficacy, may unknowingly be used to replace medicines that do have corroborated efficacy.[74]
Standardization of purity and dosage is not mandated in the United States, but even products made to the same specification may differ as a result of biochemical variations within a species of plant.[75] Plants have chemical defense mechanisms against predators that can have adverse or lethal effects on humans. Examples of highly toxic herbs include poison hemlock and nightshade.[76] They are not marketed to the public as herbs, because the risks are well known, partly due to a long and colorful history in Europe, associated with "sorcery", "magic" and intrigue.[77] Although not frequent, adverse reactions have been reported for herbs in widespread use.[78] On occasion serious untoward outcomes have been linked to herb consumption. A case of major potassium depletion has been attributed to chronic licorice ingestion.,[79] and consequently professional herbalists avoid the use of licorice where they recognise that this may be a risk. Black cohosh has been implicated in a case of liver failure.[80] Few studies are available on the safety of herbs for pregnant women,[81][82] and one study found that use of complementary and alternative medicines are associated with a 30% lower ongoing pregnancy and live birth rate during fertility treatment.[83] Examples of herbal treatments with likely cause-effect relationships with adverse events include aconite, which is often a legally restricted herb, ayurvedic remedies, broom, chaparral, Chinese herb mixtures, comfrey, herbs containing certain flavonoids, germander, guar gum, liquorice root, and pennyroyal.[84] Examples of herbs where a high degree of confidence of a risk long term adverse effects can be asserted include ginseng, which is unpopular among herbalists for this reason, the endangered herb goldenseal, milk thistle, senna, against which herbalists generally advise and rarely use, aloe vera juice, buckthorn bark and berry, cascara sagrada bark, saw palmetto, valerian, kava, which is banned in the European Union, St. John's wort, Khat, Betel nut, the restricted herb Ephedra, and Guarana.[6]
There is also concern with respect to the numerous well-established interactions of herbs and drugs.[6] In consultation with a physician, usage of herbal remedies should be clarified, as some herbal remedies have the potential to cause adverse drug interactions when used in combination with various prescription and over-the-counter pharmaceuticals, just as a patient should inform a herbalist of their consumption of orthodox prescription and other medication.
For example, dangerously low blood pressure may result from the combination of an herbal remedy that lowers blood pressure together with prescription medicine that has the same effect. Some herbs may amplify the effects of anticoagulants.[85] Certain herbs as well as common fruit interfere with cytochrome P450, an enzyme critical to much drug metabolism.[86]
Name confusion
The common names of herbs (folk taxonomy) may not reflect differences in scientific taxonomy, and the same (or a very similar) common name might group together different plant species with different effects.
For example, in 1993 in Belgium, medical doctors created a formula including some Traditional Chinese medicine (TCM) herbs for weight loss. One herb (Stephania tetrandra) was swapped for another (Aristolochia fangchi) whose name in Chinese was extremely similar but which contained higher levels of a renal toxin, aristolochic acid; this mistake resulted in 105 cases of kidney damage.[87][88]
Note that neither herb used in a TCM context would be used for weight loss or given for long periods of time. In Chinese medicine these herbs are used for certain forms of acute arthritis and edema.[89][90][91]
For this reason, Western herbalists use binomial nomenclature in their terminology within the profession.
Effectiveness
 Running total of the number of research papers listed on PubMed from 1990-2007 containing the word "phytotherapy."[original research?]
Running total of the number of research papers listed on PubMed from 1990-2007 containing the word "phytotherapy."[original research?]
The highest standard for pharmaceutical testing is repeated, small-scale, randomized, double-blind tests.[citation needed] In 2002 the U.S. National Center for Complementary and Alternative Medicine of the National Institutes of Health began funding clinical trials into the effectiveness of herbal medicine.[92] In a 2010 survey of 1000 plants, 356 had clinical trials published evaluating their "pharmacological activities and therapeutic applications" while 12% of the plants, although available in the Western market, had "no substantial studies" of their properties.[93]
Many herbs have shown positive results in-vitro, animal model or small-scale clinical tests[94] but many studies on herbal treatments have also found negative results.[95] The quality of the trials on herbal remedies is highly variable and many trials of herbal treatments have been found to be of poor quality, with many trials lacking an intention to treat analysis or a comment on whether blinding was successful.[96] The few randomized, double-blind tests that receive attention in medical publications are often questioned on methodological grounds or interpretation. Likewise, studies published in peer-reviewed medical journals such as Journal of the American Medical Association receive more consideration than those published in specialized herbal journals.
One study found that non-impact factor alternative medicine journals published more studies with positive results than negative results and that trials finding positive results were of lower quality than trials finding negative results. High impact factor mainstream medical journals, on the other hand, published equal numbers of trials with positive and negative results. In high impact journals, trials finding positive results were also found to have lower quality scores than trials finding negative results.[95] Another study reported that some clinical studies of herbal medicines were not inferior to similar medical studies.[97] However, this study used a matched pair design and excluded all herbal trials that were not controlled, did not use a placebo or did not use random or quasi random assignment.
Herbalists criticize mainstream studies on the grounds that they make insufficient use of historical usage, which has been shown useful in drug discovery and development in the past and present[2] They maintain that tradition can guide the selection of factors such as optimal dose, species, time of harvesting and target population.[98]
Dosage is in general an outstanding issue for herbal treatments: while most medicines are heavily tested to determine the most effective and safest dosages (especially in relation to things like body weight, drug interactions, etc.), there are fewer varieties of dosages for various herbal treatments on the market.[citation needed] Furthermore, from a conventional pharmacological perspective, herbal medicines taken in whole form cannot generally guarantee a consistent dosage or drug quality, since certain samples may contain more or less of a given active ingredient.
Several methods of standardization may be applied to herbs. One is the ratio of raw materials to solvent. However different specimens of even the same plant species may vary in chemical content. For this reason, thin layer chromatography is sometimes used by growers to assess the content of their products before use. Another method is standardization on a signal chemical.[99]
Standards and quality control
The issue of regulation is an area of continuing controversy in the EU and USA. At one end of the spectrum, some herbalists maintain that traditional remedies have a long history of use, and do not require the level of safety testing as xenobiotics or single ingredients in an artificially concentrated form.[citation needed] On the other hand, others are in favor of legally enforced quality standards, safety testing and prescription by a qualified practitioner.[citation needed] Some professional herbalist organizations have made statements calling for a category of regulation for herbal products.[100] Yet others agree with the need for more quality testing but believe it can be managed through reputation without government intervention.[101] The legal status of herbal ingredients varies by country.
In the EU, herbal medicines are now regulated under the European Directive on Traditional Herbal Medicinal Products.
In the United States, most herbal remedies are regulated as dietary supplements by the Food and Drug Administration.[citation needed] Manufacturers of products falling into this category are not required to prove the safety or efficacy of their product, though the FDA may withdraw a product from sale should it prove harmful.[102][103]
The National Nutritional Foods Association, the industry's largest trade association, has run a program since 2002, examining the products and factory conditions of member companies, giving them the right to display the GMP (Good Manufacturing Practices) seal of approval on their products.[62]
In the UK, herbal remedies that are bought over the counter are regulated as supplements, as in the US[citation needed]. However, herbal remedies prescribed and dispensed by a qualified "Medical Herbalist", after a personal consultation, are regulated as medicines.
A Medical Herbalist can prescribe some herbs which are not available over the counter, covered by Schedule III of the Medicines Act[citation needed]. Forthcoming changes to laws regulating herbal products in the UK, are intended to ensure the quality of herbal products used[citation needed].
Some herbs, such as cannabis and coca, are outright banned in most countries. Since 2004, the sales of ephedra as a dietary supplement is prohibited in the United States by the Food and Drug Administration.,[104] and subject to Schedule III restrictions in the United Kingdom.
Danger of extinction
Because "over 50% of prescription drugs are derived from chemicals first identified in plants,"[105] a 2008 report from the Botanic Gardens Conservation International (representing botanic gardens in 120 countries) warned that "cures for things such as cancer and HIV may become 'extinct before they are ever found'." They identified 400 medicinal plants at risk of extinction from over-collection and deforestation, threatening the discovery of future cures for disease. These included Yew trees (the bark is used for the cancer drug paclitaxel); Hoodia (from Namibia, a potential source of weight loss drugs); half of Magnolias (used as Chinese medicine for 5,000 years to fight cancer, dementia and heart disease); and Autumn crocus (for gout). Their report said that "five billion people still rely on traditional plant-based medicine as their primary form of health care."[105]
See also
- List of plants used in herbalism
- Medicinal mushrooms
- List of herbs with known adverse effects
- Herb garden
- Doctrine of signatures
References
- ^ Acharya, Deepak and Shrivastava Anshu (2008): Indigenous Herbal Medicines: Tribal Formulations and Traditional Herbal Practices, Aavishkar Publishers Distributor, Jaipur- India. ISBN 978-81-7910-252-7. pp 440.
- ^ a b c Fabricant DS, Farnsworth NR (March 2001). "The value of plants used in traditional medicine for drug discovery". Environ. Health Perspect. 109 Suppl 1: 69–75. PMC 1240543. PMID 11250806. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1240543.
- ^ Lai PK, Roy J (June 2004). "Antimicrobial and chemopreventive properties of herbs and spices". Curr. Med. Chem. 11 (11): 1451–60. PMID 15180577.
- ^ Tapsell LC, Hemphill I, Cobiac L, et al. (August 2006). "Health benefits of herbs and spices: the past, the present, the future". Med. J. Aust. 185 (4 Suppl): S4–24. PMID 17022438.
- ^ a b Talalay, P; Talalay, P (2001). "The importance of using scientific principles in the development of medicinal agents from plants.". Academic Medicine 76 (3): 238–47. PMID 11242573.
- ^ a b c d Elvin-Lewis M. (2001). "Should we be concerned about herbal remedies". Journal of Ethnopharmacology 75 (2–3): 141–164. doi:10.1016/S0378-8741(00)00394-9. PMID 11297844.
- ^ Huffman MA (May 2003). "Animal self-medication and ethno-medicine: exploration and exploitation of the medicinal properties of plants" (in hindi). Proc Nutr Soc 62 (2): 371–81. doi:10.1079/PNS2003257. PMID 14506884.
- ^ a b Engel, Cindy (2002). Wild Health: How Animals Keep Themselves Well and What We Can Learn From Them. Houghton Mifflin. ISBN 0618071784.
- ^ Out of Africa: A Tale of Gorillas, Heart Disease... and a Swamp Plant; Dybas, Raskin; BioScience 2007 57:5, 392-397 fulltext
- ^ Jann Ichida, Proceedings of the 104th General Meeting of the American Society for Microbiology. reported in Birds use herbs to protect their nests, BJS, Science Blog, Wed, 2004-05-26
- ^ Hutchings MR, Athanasiadou S, Kyriazakis I, Gordon IJ (May 2003). "Can animals use foraging behavior to combat parasites?". Proc Nutr Soc. 62 (2): 361–70. doi:10.1079/PNS2003243. PMID 14506883.
- ^ "Phascolarctos cinereus". http://animaldiversity.ummz.umich.edu/site/accounts/information/Phascolarctos_cinereus.html.
- ^ "Take Time to Identify Toxic Plants to Keep Your Family and Pets Safe". http://cetulare.ucdavis.edu/mg/articles/n052203.htm.
- ^ "Antimicrobial functions of spices: why some like it hot". Q Rev Biol. 73 (1): 3–49. March 1998. doi:10.1086/420058. PMID 9586227.
- ^ "Why vegetable recipes are not very spicy". Evol Hum Behav. 22 (3): 147–163. May 2001. doi:10.1016/S1090-5138(00)00068-4. PMID 11384883.
- ^ . Bibcode 1975Sci...190..880S. doi:10.1126/science.190.4217.880.
- ^ Aggarwal BB, Sundaram C, Malani N, Ichikawa H (2007). "Curcumin: the Indian solid gold". Adv. Exp. Med. Biol. 595: 1–75. doi:10.1007/978-0-387-46401-5_1. PMID 17569205.
- ^ Girish Dwivedi, Shridhar Dwivedi (2007) (PDF). History of Medicine: Sushruta – the Clinician – Teacher par Excellence. National Informatics Centre. http://medind.nic.in/iae/t07/i4/iaet07i4p243.pdf. Retrieved 2008-10-08.
- ^ a b c Castleman, Michael (2001). The New Healing Herbs: The Classic Guide to Nature's Best Medicines Featuring the Top 100 Time-Tested Herbs. Rodale. p. 15. ISBN 1579543049, 97815795430.
- ^ "Pharmaceutics and Alchemy". http://www.nlm.nih.gov/exhibition/islamic_medical/islamic_11.html.
- ^ Fahd, Toufic. "Botany and agriculture". pp. 815., in (Morelon & Rashed 1996, pp. 813–52)
- ^ Diane Boulanger (2002), "The Islamic Contribution to Science, Mathematics and Technology", OISE Papers, in STSE Education, Vol. 3.
- ^ Huff, Toby (2003). The Rise of Early Modern Science: Islam, China, and the West. Cambridge University Press. p. 218. ISBN 0521529948.
- ^ Jacquart, Danielle (2008). "Islamic Pharmacology in the Middle Ages: Theories and Substances". European Review 16 (2): 219–227 [223]. doi:10.1017/S1062798708000215.
- ^ Dr. Kasem Ajram (1992), Miracle of Islamic Science, Appendix B, Knowledge House Publishers. ISBN 0-911119-43-4.
- ^ Krek M. (1979). "The Enigma of the First Arabic Book Printed from Movable Type". Journal of Near Eastern Studies 38 (3): 203–212. doi:10.1086/372742.
- ^ Brater, D. Craig; Daly, Walter J. (2000). "Clinical pharmacology in the Middle Ages: Principles that presage the 21st century". Clinical Pharmacology & Therapeutics 67 (5): 447–450 [448–449]. doi:10.1067/mcp.2000.106465. PMID 10824622.
- ^ Tschanz, David W.; MSPH (2003). "Arab Roots of European Medicine" (PDF). Heart Views 4: 2. http://www.bxscience.edu/ourpages/auto/2007/11/9/1194631995278/Arab%20Roots%20of%20European%20Medicine.pdf.
- ^ Eldredge Jonathan D. (2003). "The Randomised Controlled Trial design: unrecognized opportunities for health sciences librarianship". Health Information and Libraries Journal 20: 34–44 [36]. doi:10.1046/j.1365-2532.20.s1.7.x.
- ^ Bloom Bernard S., Retbi Aurelia, Dahan Sandrine, Jonsson Egon (2000). "Evaluation Of Randomized Controlled Trials On Complementary And Alternative Medicine". International Journal of Technology Assessment in Health Care 16 (1): 13–21. doi:10.1017/S0266462300016123. PMID 10815350.
- ^ Brater, D. Craig; Daly, Walter J. (2000). "Clinical pharmacology in the Middle Ages: Principles that presage the 21st century". Clinical Pharmacology & Therapeutics 67 (5): 447–450 [449]. doi:10.1067/mcp.2000.106465. PMID 10824622.
- ^ Daly, Walter J.; Brater, D. Craig (2000). "Medieval contributions to the search for truth in clinical medicine". Perspectives in Biology and Medicine 43 (4): 530–540. PMID 11058989.
- ^ a b Edgar J. DaSilva, Elias Baydoun, Adnan Badran (2002). "Biotechnology and the developing world". Electronic Journal of Biotechnology 5 (1). doi:10.2225/vol5-issue1-fulltext-1. ISSN 0717-3458. http://www.scielo.cl/scielo.php?pid=S0717-34582002000100013&script=sci_arttext&tlng=en.
- ^ "Traditional medicine". http://www.who.int/mediacentre/factsheets/fs134/en/.
- ^ Barnes, Joanne; Ernst, Edzard (1998). "Traditional herbalists’ prescriptions for common clinical conditions: A survey of members of the UK National Institute of Medical Herbalists". Phytotherapy research 12 (5): 369. doi:10.1002/(SICI)1099-1573(199808)12:5<369::AID-PTR304>3.0.CO;2-8.
- ^ Casey MG, Adams J, Sibbritt D (March 2007). "An examination of the prescription and dispensing of medicines by Western herbal therapists: a national survey in Australia". Complement Ther Med 15 (1): 13–20. doi:10.1016/j.ctim.2005.10.008. PMID 17352967.
- ^ "Traditional medicine.". http://www.who.int/mediacentre/factsheets/fs134/en/.
- ^ Interactive European Network for Industrial Crops and their Applications (2000-2005). "Summary Report for the European Union". QLK5-CT-2000-00111. http://ec.europa.eu/research/quality-of-life/ka5/en/00111.html. [www.ienica.net/reports/ienicafinalsummaryreport2000-2005.pdf Free full-text].
- ^ "The role of weeds as sources of pharmaceuticals". Journal of Ethnopharmacology 92 (2–3): 163–166. June 2004. doi:10.1016/j.jep.2004.03.002. PMID 15137997.
- ^ "The importance of weeds in ethnopharmacology". Journal of Ethnopharmacology 75 (1): 19–23. April 2001. doi:10.1016/S0378-8741(00)00385-8. PMID 11282438.
- ^ "Unraveling the Function of Secondary Metabolites". http://4e.plantphys.net/article.php?ch=13&id=313.
- ^ Lichterman, B. L (2004). "The Story of a Wonder Drug". BMJ 329 (7479): 1408. doi:10.1136/bmj.329.7479.1408.
- ^ Vickers, A; Zollman, C (October 16, 1999). "ABC of complementary medicine: Herbal medicine". British Medical Journal 319 (7216): 1050–3. PMC 1116847. PMID 10521203. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1116847.
- ^ "What is Herb Standardization?". http://content.herbalgram.org/abc/herbalgram/articleview.asp?a=2230.
- ^ Challem, Jack (January 1999). "The Problem With Herbs". Natural Health. http://findarticles.com/p/articles/mi_m0NAH/is_1_29/ai_54062642/. Retrieved 2010-12-23.
- ^ "Synergy and other interactions in phytomedicines". Phytomedicine 8 (5): 401–409. 2001. doi:10.1078/0944-7113-00060. PMID 11695885.
- ^ Goldman, Peter (2001). "Herbal Medicines Today and the Roots of Modern Pharmacology" (PDF). Annals of internal medicine 135 (8 Pt 1): 594–600. PMID 11601931. http://annals.highwire.org/cgi/reprint/135/8_Part_1/594.pdf.
- ^ "Synergy and other interactions in phytomedicines". Phytomedicine 8 (5): 401–409. 2001. doi:10.1078/0944-7113-00060. PMID 11695885.
- ^ "Emodin – a secondary metabolite with multiple ecological functions in higher plants". New Phytologist 155 (2): 205–217. 2002. doi:10.1046/j.1469-8137.2002.00459.x.
- ^ "Plant’s defence and its benefits for animals and medicine: role of phenolics and terpenoids in avoiding oxygen stress". Plant Physiology and Biochemistry 40 (6–8): 471–478. June–August 2002. doi:10.1016/S0981-9428(02)01395-5.
- ^ "Medicinal Plants and Phytomedicines. Linking Plant Biochemistry and Physiology to Human Health". Plant Physiol, 124 (2): 507–514. October 2000. doi:10.1104/pp.124.2.507. PMC 1539282. PMID 11027701. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1539282.
- ^ "Atherosclerosis pathophysiology and the role of novel risk factors: a clinicobiochemical perspective". Angiology 58 (5): 513–22. 2007 October–November. doi:10.1177/0003319707303443. PMID 18024933.
- ^ "Antioxidant approach to disease management and the role of 'Rasayana' herbs of Ayurveda". J Ethnopharmacol. 99 (2): 165–78. 2005. doi:10.1016/j.jep.2005.02.035. PMID 15894123.
- ^ Slikkerveer, L.J. (2006). The Challenge Of Non-experimental Validation Of Mac Plants. Springer. http://library.wur.nl/ojs/index.php/frontis/article/viewFile/1220/792.
- ^ "History as a tool in identifying "new" old drugs". Adv Exp Med Biol. 505: 89–94. 2002. PMID 12083469.
- ^ Barnes, P M; Powell-Griner E, McFann K, Nahin R L (2004-05-27). "Complementary and Alternative Medicine Use Among Adults: United States, 2002" (PDF). Advance data from vital and health statistics; no 343. National Center for Health Statistics. 2004. pp. 20. http://nccam.nih.gov/news/report.pdf. Retrieved September 16, 2006. (See table 1 on page 8).
- ^ More Than One-Third of U.S. Adults Use Complementary and Alternative Medicine Press release, May 27, 2004. National Center for Complementary and Alternative Medicine
- ^ James A. Duke (Dec/January 2000). "Returning to our Medicinal Roots". Mother Earth News: 26–33. http://www.highbeam.com/doc/1G1-73088521.html.
- ^ Cochrane reviews of complementary and alternative therapies: evaluating the strength of the evidence Cochrane Collaboration. Published 2004. Accessed 9 January 2010.
- ^ Liao, Hui; Banbury, Linda K.; Leach, David N. (2008). "Antioxidant activity of 45 Chinese herbs and the relationship with their TCM characteristics". Evidence-Based Complementary and Alternative Medicine 5 (4): 429–34. doi:10.1093/ecam/nem054. PMC 2586310. PMID 18955214. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2586310.
- ^ Boxin Ou, Dejian Huang1, Maureen Hampsch-Woodill and Judith A. Flanagan (2003). "When east meets west: the relationship between yin-yang and antioxidation-oxidation". The FASEB Journal 17 (2): 127–129. doi:10.1096/fj.02-0527hyp. PMID 12554690.
- ^ a b Safety & Regulation--Who's Watching the Herbal Store?, Tillotson Institute of Natural Health
- ^ Tillotson Institute of Natural Health - The Language of Herbs
- ^ Theivaththin Kural, Chandrasekarendra saraswathi sankaracharya,Vol.3,pp737
- ^ William LeSassier Archive website
- ^ David Winston Center for Herbal Studies website
- ^ [1] website
- ^ a b c d e Groot Handboek Geneeskrachtige Planten by Geert Verhelst
- ^ "Essential Oil Safety Information". http://aromaweb.com/articles/safety.asp.
- ^ "Aromatherapy". http://www.umm.edu/altmed/articles/aromatherapy-000347.htm.
- ^ Herz RS. (2009). "Aroma therapy facts and fiction: a scientific analysis". Int J Neurosci 119 (2): 263–290. doi:10.1080/00207450802333953. PMID 19125379.
- ^ Gilani AH, Shah AJ, Zubair A., Khalid S, Kiani J, Ahmed A, Rasheed M, Ahmad V (2009). "Chemical composition and mechanisms underlying the spasmolytic and bronchodilatory properties of the essential oil of Nepeta cataria L". J of Ethnopharmacol 121 (3): 405–411. doi:10.1016/j.jep.2008.11.004.
- ^ Vickers AJ (2007). "Which botanicals or other unconventional anticancer agents should we take to clinical trial?". J Soc Integr Oncol 5 (3): 125–9. doi:10.2310/7200.2007.011. PMC 2590766. PMID 17761132. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2590766.
- ^ Ernst E (2007). "Herbal medicines: balancing benefits and risks". Novartis Found. Symp. 282: 154–67; discussion 167–72, 212–8. doi:10.1002/9780470319444.ch11. PMID 17913230.
- ^ "Botanical Products". http://www.medscape.com/viewarticle/425061.
- ^ Müller, JL (1998). "Love potions and the ointment of witches: historical aspects of the nightshade alkaloids". J Toxicol Clin Toxicol. 36 (6): 617–27. PMID 9776969.
- ^ Lee, MR (December 2006). "Solanaceae III: henbane, hags and Hawley Harvey Crippen". J R Coll Physicians Edinb. 36 (4): 366–73. PMID 17526134.
- ^ Pinn, G (November 2001). "Adverse effects associated with herbal medicine". Aust Fam Physician. 30 (11): 1070–5. PMID 11759460.
- ^ Lin, Shih-Hua; Yang, SS; Chau, T; Halperin, ML (March 2003). "An unusual cause of hypokalemic paralysis: chronic licorice ingestion". Am J Med Sci. 325 (3): 153–6. doi:10.1097/00000441-200303000-00008. PMID 12640291.
- ^ Lynch, Christopher R.; Folkers, ME; Hutson, WR (June 2006). "Fulminant hepatic failure associated with the use of black cohosh: a case report". Liver Transpl. 12 (6): 989–92. doi:10.1002/lt.20778. PMID 16721764.
- ^ Born, D; Barron, ML (May 2005-June). "Herb use in pregnancy: what nurses should know". MCN Am J Matern Child Nurs. 30 (3): 201–6. PMID 15867682.
- ^ Herbs to avoid during pregnancy, Gaia Garden website
- ^ Boivin J., Schmidt L. (2009). "Use of complementary and alternative medicines associated with a 30% lower onging pregnancy/live birth rate during 12 months of fertility treatment". Human Reproduction 21 (7): 1626–1631. doi:10.1093/humrep/dep077.
- ^ Ernst E (1998). "Harmless Herbs? A Review of the Recent Literature" (PDF). The American Journal of Medicine 141 (2): 170–8. doi:10.1016/S0002-9343(97)00397-5. PMID 9528737. http://toxicology.usu.edu/endnote/Harmless-Herbs.pdf. Retrieved 27 December 2010.
- ^ Spolarich AE, Andrews L (2007 Summer). "An examination of the bleeding complications associated with herbal supplements, antiplatelet and anticoagulant medications". J Dent Hyg. 81 (3): 67. PMID 17908423. http://findarticles.com/p/articles/mi_hb6368/is_3_81/ai_n31843689/.
- ^ Nekvindová J, Anzenbacher P (July 2007). "Interactions of food and dietary supplements with drug metabolising cytochrome P450 enzymes". Ceska Slov Farm. 56 (4): 165–73. PMID 17969314.
- ^ "Complexities of the herbal nomenclature system in traditional Chinese medicine (TCM): lessons learned from the misuse of Aristolochia-related species and the importance of the pharmaceutical name during botanical drug product development". Phytomedicine.;():. Epub 2006 Jul 24 14 (4): 273–9. April 2007. doi:10.1016/j.phymed.2006.05.009. PMID 16863692.
- ^ "Misuse of herbal remedies: the case of an outbreak of terminal renal failure in Belgium (Chinese herbs nephropathy)". J Altern Complement Med. 4 (1): 9–13. 1998 Spring. doi:10.1089/acm.1998.4.1-9. PMID 9553830.
- ^ Dan Bensky, Steven Clavey, Erich Stoger, and Andrew Gamble. Chinese Herbal Medicine: Materia Medica, Third Edition. 2004: 1054-1055
- ^ Vanherweghem JL, Depierreux M, Tielemans C, Depierreux M., Vanhaelen-Fastre R., Vanhaelen M., Dratwa M., Richard C. et al. (Feb 1993). "Rapidly progressive interstitial renal fibrosis in young women: association with slimming regimen including Chinese herbs". Lancet 341 (8842): 387–91. doi:10.1016/0140-6736(93)92984-2. PMID 8094166.
- ^ Vanhaelen M, Vanhaelen-Fastre R, But P, Vanherweghem JL. (Jan 1994). "Identification of aristolochic acid in Chinese herbs". Lancet 343 (8890): 174. doi:10.1016/S0140-6736(94)90964-4. PMID 7904018.
- ^ Herbal Medicine, NIH Institute and Center Resources, National Center for Complementary and Alternative Medicine, National Institutes of Health.
- ^ Cravotto G, Boffa L, Genzini L, Garella D (February 2010). "Phytotherapeutics: an evaluation of the potential of 1000 plants". J Clin Pharm Ther 35 (1): 11–48. doi:10.1111/j.1365-2710.2009.01096.x. PMID 20175810.
- ^ Srinivasan K (2005). "Spices as influencers of body metabolism: an overview of three decades of research". Food Research International 38 (1): 77–86. doi:10.1016/j.foodres.2004.09.001.
- ^ a b "Location bias in controlled clinical trials of complementary/alternative therapies". International Journal of Epidemiology 53 (5): 485–489. 2000. doi:10.1016/S0895-4356(99)00220-6. PMID 10812320.
- ^ "The methodological quality of randomized controlled trials of homeopathy, herbal medicines and acupuncture". International Journal of Epidemiology 30 (3): 526–531. 2005. doi:10.1093/ije/30.3.526. PMID 11416076. http://ije.oxfordjournals.org/cgi/content/full/30/3/526.
- ^ Nartey L, Huwiler-Müntener K, Shang A, Liewald K, Jüni P, Egger M (August 2007). "Matched-pair study showed higher quality of placebo-controlled trials in Western phytotherapy than conventional medicine". J Clin Epidemiol 60 (8): 787–94. doi:10.1016/j.jclinepi.2006.11.018. PMID 17606174.
- ^ Eric Yarnell, N.D., R.H., and Kathy Abascal, J.D (2002). "Dilemmas of Traditional Botanical Research". HerbalGram. 55: 46–54.
- ^ "What is Herb Standardization?". HerbalGram. (52): 25. 2001. http://content.herbalgram.org/iherb/herbalgram/articleview.asp?a=2230.
- ^ "Wrangling an Herbal Legen" (PDF). http://content.herbalgram.org/abc/HEG/files/MBHerbsforHealth.pdf.
- ^ "Some Arguments against the Standardization of Herbalists". http://www.gaianstudies.org/articles10.htm.
- ^ US Dietary Supplement Health and Education Act of 1994
- ^ Goldman P (2001). "Herbal medicines today and the roots of modern pharmacology". Ann. Intern. Med. 135 (8 Pt 1): 594–600. PMID 11601931.
- ^ FDA Issues Regulation Prohibiting Sale of Dietary Supplements Containing Ephedrine Alkaloids and Reiterates Its Advice That Consumers Stop Using These Products
- ^ a b BBC NEWS, Medical plants 'face extinction'
Further reading
- Lindequist, U.; Niedermeyer, T.H.J. ; Jülich, W.D. (2005). "The pharmacological potential of mushrooms". Evid Based Complement Alternat Med. 2 (3): 285–99. doi:10.1093/ecam/neh107. PMC 1193547. PMID 16136207. http://ecam.oxfordjournals.org/cgi/content/full/2/3/285.
- Lesley Braun and Marc Cohen. (2007). Herbs and Natural Supplements: An Evidence-Based Guide. Elsevier Australia. ISBN 0-7295-3796-X 9780729537964.
Traditional medicine East Asian 
South & Southeast
AsianMediterranean &
Near EasternAfrican Americas Australasia & Oceania General Medicinal herbs and fungi Herbs Regional practices Related subjects Categories:- Herbalism
- Alternative medical systems
- Biologically based therapies
- Dietary supplements
Wikimedia Foundation. 2010.