- Eosinophilic esophagitis
-
Eosinophilic esophagitis Classification and external resources 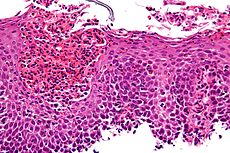
Micrograph showing eosinophilic esophagitis. H&E stain.ICD-9 530.13  Endoscopic image of esophagus in a case of eosinophilic esophagitis. Concentric rings are termed trachealization of the esophagus.
Endoscopic image of esophagus in a case of eosinophilic esophagitis. Concentric rings are termed trachealization of the esophagus.
 The barium swallow of the esophagus on the left side shows multiple rings associated with eosinophilic esophagitis.
The barium swallow of the esophagus on the left side shows multiple rings associated with eosinophilic esophagitis.
Eosinophilic esophagitis is an allergic inflammatory condition of the esophagus. Symptoms are swallowing difficulty, food impaction, and heartburn. The disease was first described in children but occurs in adults as well. The condition is not well understood, but food allergy may play a significant role.[1]
Contents
Diagnosis
The diagnosis of eosinophilic esophagitis is a clinicopathologic one, requiring mucosal biopsies of the esophagus obtained during esophagogastroduodenoscopy. Normal esophageal mucosa does not have any infiltrating eosinophils. In eosinophilic esophagitis, eosinophils inflitrate the epithelium. A minimum of 15 eosinophils per high power field are required to make the diagnosis. Typically, eosinophils can be found in superficial clusters near the surface of the epithelium. Degranulated forms of eosinophils are also often visualized. In addition to esophageal infiltration, an expansion of the basal layer is seen in response to the inflammatory damage to the epithelium.[2]
At the time of endoscopy, ridges or furrows may be seen in the esophagus wall. Presence of white exudates in esophagus is also suggestive of the diagnosis. Sometimes, multiple rings may occur in the esophagus, leading to the term "corrugated esophagus" or "feline esophagus" due to the similarity in the rings of the cat esophagus. In the radiology literature, the term "ringed esophagus" has been used for the appearance of eosinophilic esophagitis on barium esophagrams to contrast with the appearance of transient transverse folds sometimes seen with esophageal reflux (termed "feline esophagus").[3][4]
A characteristic set of genes elucidated by Dr. Marc Rothenberg's laboratory and termed the "EE transcriptome" is expressed and distinguishes patients with EE from unaffected individuals or from patients with other forms of esophagitis.[5]
Treatment
Treatment strategies include dietary modification to exclude food allergens, medical therapy, and mechanical dilatation of the esophagus. The initial approach to the disorder is often allergy evaluation in an attempt to identify the allergens in the diet or environment that may be triggering the disease. If the offending agent is found, the diet is modified so that these allergens are eliminated. There are cases, especially in children, where there are multiple food allergies involved. Some patients require an elemental diet through the use of a specialty formula. Sticking to this diet and drinking the required amount of formula can be difficult. The use of feeding tubes in these situations is often required.[6]
A minority of EE patients appear to be non-atopic (non-allergic), yet still present with this disease. Eosinophilic Esophagitis can cause severe pain in many patients.
First line therapy is with swallowed liquid corticosteroids. Proton Pump inhibition historically had no role in the treatment of eosinophilic esophagitis, although some recent evidence suggests that a significant proportion of patients with suspected EE achieve clinicopathological remission on PPI therapy[7] . EE patients by definition have persistent symptoms even with acid-inhibition therapy. For this reason, alternative medical therapies are often employed. Treatment that targets the inflammation includes swallowed corticosteroids such as fluticasone,a topical viscous budesonide oral suspension, leukotriene antagonists like montelukast, and anti-interleukins such as the anti-IL-5 monoclonal antibody mepolizumab. Other drugs attempt to halt the allergic response; these include antihistamines such as loratadine. Patients with severe symptoms despite these interventions may require oral corticosteroids such as methylprednisolone.
Mechanical dilatation may be considered in severe cases of EE that have progressed to esophageal stricture or severe stenosis. Dilatation is accomplished by passing dilators through the mouth and down the esophagus to gently expand its diameter. As the esophagus of patients with EE is rather thin and delicate, care is taken not to perforate the esophagus by overzealous dilatation.
History
Eosinophilic esophagitis (often referred to as EE in the United States, or EO in countries which use British spelling) was only discovered in recent years, and little is known about its pathogenesis. EE is a chronic disease associated with an elevated count of eosinophils in the esophagus. Normally, very few or no eosinophils are present in this upper digestive organ. In the past, patients with EE were incorrectly diagnosed as GERD suffererers. These patients were typically prescribed proton pump inhibitors, under the assumption that their problem was caused by excess stomach acid. However, researches have since discovered that EE patients often have a normal pH in their GI tract. The symptoms of GERD and EE are often similar, and this makes the diagnosis more difficult. But when a patient suffering from esophageal discomfort tests normal from an esophageal pH monitoring, GERD is eliminated as a possible cause and EE becomes the main suspect. In fact, GERD patients may also show an elevated count of eosinophils, but this elevation is much lower than in EE patients.
At this time, the only reliable method used to diagnose EE is the upper endoscopy with multiple biopsies. The barium swallow test may show irregularities in the shape of the esophagus caused by EE, but not all patients have such physical characteristics. The endoscopy is performed by a gastroenterologist, a specialist in pathology associated with the GI tract. The upper endoscopy is normally done as an outpatient procedure, with local anaesthetic spray or the administration of mild sedation. Biopsy samples must be taken from multiple sites on the surface of the esophagus, to ensure that the condition is not overlooked.
More recently, researches have begun looking for links between EE and autoimmune diseases. Some EE patients suffer from skin conditions such as psoriasis or seborrheic dermatitis or respiratory conditions such as asthma or allergic rhinitis. At this time, there appears to be no proven link between EE and esophageal cancer.
See also
References
- ^ Blanchard C, Rothenberg ME (January 2008). "Basic pathogenesis of eosinophilic esophagitis". Gastrointest. Endosc. Clin. N. Am. 18 (1): 133–43; x. doi:10.1016/j.giec.2007.09.016. PMC 2194642. PMID 18061107. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2194642.
- ^ Furuta GT, Liacouras CA, Collins MH, Gupta SK, Justinich C, Putnam PE, Bonis P, Hassall E, Straumann A, Rothenberg ME; First International Gastrointestinal Eosinophil Research Symposium (FIGERS) Subcommittees. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007 Oct;133(4):1342-63.
- ^ Zimmerman SL, Levine MS, Rubesin SE, et al. (July 2005). "Idiopathic eosinophilic esophagitis in adults: the ringed esophagus". Radiology 236 (1): 159–65. doi:10.1148/radiol.2361041100. PMID 15983073.
- ^ Samadi F, Levine MS, Rubesin SE, Katzka DA, Laufer I (April 2010). "Feline esophagus and gastroesophageal reflux". AJR Am J Roentgenol 194 (4): 972–6. doi:10.2214/AJR.09.3352. PMID 20308499.
- ^ Blanchard C, Wang N, Stringer KF, Mishra A, Fulkerson PC, Abonia JP, Jameson SC, Kirby C, Konikoff MR, Collins MH, Cohen MB, Akers R, Hogan SP, Assa'ad AH, Putnam PE, Aronow BJ, Rothenberg ME (February 2006). "Eotaxin-3 and a uniquely conserved gene-expression profile in eosinophilic esophagitis". J. Clin. Invest. 116 (2): 536–47. doi:10.1172/JCI26679. PMC 1359059. PMID 16453027. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1359059.
- ^ http://www.apfed.org/
- ^ Molina-Infante, Javiar (2011). J Gastroenterology 46: 712–3. doi:10.1007/s00535-011-0388-8.
External links
- American Partnership for Eosinophilic Disorders
- Families Affected By Eosinophilic Disorders
- Canadian Council of Eosinophilic Disorders
- Cincinnati Center for Eosinophilic Disorders
- Hoover boy's rare disease leaves him allergic to almost everything he eats
- Research For Eosinophilic Disorders
- Australian Support for Eosinophilic Disorders
Health science - Medicine - Allergic conditions Respiratory system Allergic rhinitis · Asthma · Hypersensitivity pneumonitis · Eosinophilic pneumonia · Churg-Strauss syndrome · Allergic bronchopulmonary aspergillosis · Farmer's lung · Laboratory animal allergySkin Blood and immune system Circulatory system Digestive system Coeliac disease · Eosinophilic gastroenteritis · Eosinophilic esophagitis · Food allergy · Milk intoleranceNervous system Eosinophilic meningitisGenitourinary system Other conditions Categories:- Esophagus disorders
Wikimedia Foundation. 2010.
