- Plasmodium
-
This article is about the malaria parasite. For plasmodial slime molds, see Slime mold.
Plasmodium 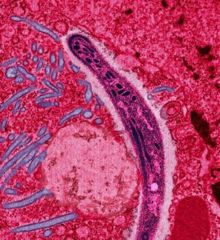
Scientific classification Domain: Eukaryota Kingdom: Chromalveolata Superphylum: Alveolata Phylum: Apicomplexa Class: Aconoidasida Order: Haemosporida Family: Plasmodiidae Genus: Plasmodium
Marchiafava & Celli, 1885subgenera Asiamoeba (5 species)
Bennetinia (1 species)
Carinamoeba (7 species)
Giovannolaia (14 species)
Haemamoeba (12 species)
Huffia (2 species)
Lacertamoeba (2 species)
Laverania (5 species)
Ophidiella (3 species)
Novyella (19 species)
Nyssorhynchus (1 species)
Paraplasmodium (3 species)
Plasmodium (30 species)
Sauramoeba (15 species)
Vinckeia (32 species)
Incertae sedis (124 species)Plasmodium is a genus of parasitic protists. Infection by these organisms is known as malaria. The genus Plasmodium was described in 1885 by Ettore Marchiafava and Angelo Celli. Currently over 200 species of this genus are recognized and new species continue to be described.[1][2]
Of the over 200 known species of Plasmodium, at least 11 species infect humans. Other species infect other animals, including monkeys, rodents, birds, and reptiles. The parasite always has two hosts in its life cycle: a mosquito vector and a vertebrate host.
Contents
History
Main article: History of malariaThe organism itself was first seen by Laveran on November 6, 1880 at a military hospital in Constantine, Algeria, when he discovered a microgametocyte exflagellating. In 1885, similar organisms were discovered within the blood of birds in Russia. There was brief speculation that birds might be involved in the transmission of malaria; in 1894 Patrick Manson hypothesized that mosquitoes could transmit malaria. This hypothesis was independently confirmed by the Italian physician Giovanni Battista Grassi working in Italy and the British physician Ronald Ross working in India, both in 1898. Ross demonstrated the existence of Plasmodium in the wall of the midgut and salivary glands of a Culex mosquito using bird species as the vertebrate host. For this discovery he won the Nobel Prize in 1902. Grassi showed that human malaria could only be transmitted by Anopheles mosquitoes. It is worth noting, however, that for some species the vector may not be a mosquito.[citation needed]
Biology
The genome of four Plasmodium species - Plasmodium falciparum, Plasmodium knowlesi, Plasmodium vivax and Plasmodium yoelii - have been sequenced. All these species have genomes of about 25 megabases organised into 14 chromosomes consistent with earlier estimates. The chromosomes vary in length from 500 kilobases to 3.5 megabases and it is presumed that this is the pattern throughout the genus.
The biology of these organisms is more fully described on the Plasmodium falciparum biology page.
Diagnostic characteristics of the genus Plasmodium
- Merogony occurs both in erythrocytes and other tissues
- Merozoites, schizonts or gametocytes can be seen within erythrocytes and may displace the host nucleus
- Merozoites have a “signet-ring” appearance due to a large vacuole that forces the parasite’s nucleus to one pole
- Schizonts are round to oval inclusions that contain the deeply staining merozoites
- Forms gamonts in erythrocytes
- Gametocytes are 'halter-shaped' similar to Haemoproteus but the pigment granules are more confined
- Hemozoin is present
- Vectors are either mosquitos or sandflies
- Vertebrate hosts include mammals, birds and reptiles
Life cycle
The life cycle of Plasmodium while complex is similar to several other species in the Haemosporidia.
All the Plasmodium species causing malaria in humans are transmitted by mosquito species of the genus Anopheles. Species of the mosquito genera Aedes, Culex, Culiseta, Mansonia and Theobaldia can also transmit malaria but not to humans. Bird malaria is commonly carried by species belonging to the genus Culex. The life cycle of Plasmodium was discovered by Ross who worked with species from the genus Culex.
Both sexes of mosquitos live on nectar. Because nectar's protein content alone is insufficient for oogenesis (egg production) one or more blood meals is needed by the female. Only female mosquitoes bite.
Sporozoites from the saliva of a biting female mosquito are transmitted to either the blood or the lymphatic system of the recipient.[3] It has been known for some time now that the parasites block the salivary ducts of the mosquito and as a consequence the insect normally requires multiple attempts to obtain blood. The reason for this has not been clear. It is now known that the multiple attempts by the mosquito may contribute to immunological tolerance of the parasite.[4] The majority of sporozoites appear to be injected into the subcutaneous tissue from which they migrate into the capillaries. A proportion are ingested by macrophages and still others are taken up by the lymphatic system where they are presumably destroyed. ~10% of the parasites inoculated by the mosquitoes may remain in the skin where they may develop into infective merozoites.[5]
Hepatic stages
The majority of sporozoites migrate to the liver and invade hepatocytes. For reasons that are currently unclear each sporozoite typically penetrates several hepatocytes before choosing one to reside within. Once the sporozoite has ceased migration it undergoes an initial remodelling of the pellicle, with disassembly of the inner membrane complex and the appearance of a bulb that progressively enlarges until the initially elongated sporozoite has transformed into a rounded form.[6][7] This rounded form then matures within the hepatocyte to a schizont containing many merozoites. In some Plasmodium species, such as Plasmodium vivax and Plasmodium ovale, the parasite in the hepatocyte may not achieve maturation to a schizont immediately but remain as a latent or dormant form and called a hypnozoite. Although Plasmodium falciparum is not considered to have a hypnozoite form,[8] this may not be entirely correct (vide infra). This stage may be as short as 48 hours in the rodent parasites and as long as 15 days in P. malariae in humans.
There is considerable variation in the appearance of the blood forms between individuals experimentally inoculated at the same time. Even within a single experimentally individual there may be considerable variation in the maturity of the hepatic forms seen on liver biopsy.
A proportion of the hepatic stages may remain within the liver for considerable time - a form known as hypnozoites. Reactivation of the hypnozoites has been reported for up to 30 years after the initial infection in humans. The factors precipating this reactivation are not known. In the species Plasmodium ovale[9] and Plasmodium vivax,[10] but not in Plasmodium malariae,[11][12] hypnozoites have been shown to occur. It is not yet known if hypnozoite reactivaction occurs with any of the remaining species that infect humans but this is presumed to be the case.
The development from the hepatic stages to the erythrocytic stages has, until very recently, been obscure. In 2006 it was shown that the parasite buds off the hepatocytes in merosomes containing hundreds or thousands of merozoites.[13] These merosomes lodge in the pulmonary capillaries and slowly disintegrate there over 48–72 hours releasing merozoites.[14] The membrane of the merosome is derived from the host hepatocyte.[15] The membrane of the merozoites is formed by repeated invagination of the parasite's membrane. The parastitophorus vacuole breaks down within the hepatocyte. This is associated with degeneration of the host cell's mitochondria and cessation of protein synthesis which is probably due to the lack of mitochondially produced ATP. The membrane of the merosome is then formed from that of the hepatocyte membrane but the hepatocyte proteins within the membrane are lost. This host derived membrane presumably provides protection from the immune system while the merozoites are transported to the lung. Erythrocyte invasion is enhanced when blood flow is slow and the cells are tightly packed: both of these conditions are found in the alveolar capillaries.
Infection of the liver may be influenced by the iron regulatory hormone hepcidin[16] and this may play a role in preventing superinfection despite repeated inoculation.
Erythrocyte stages
After entering the erythrocyte, the merozoite lose one of their membranes, the apical rings, conoid and the rhopteries. Phagotropy commences and both smooth and granular endoplasmic reticulum becomes prominent. The nucleus may become lobulated.
Within the erythrocytes the merozoite grow first to a ring-shaped form and then to a larger trophozoite form. In the schizont stage, the parasite divides several times to produce new merozoites, which leave the red blood cells and travel within the bloodstream to invade new red blood cells. The parasite feeds by ingesting haemoglobin and other materials from red blood cells and serum. The feeding process damages the erythrocytes. Details of this process have not been studied in species other than Plasmodium falciparum so generalizations may be premature at this time.
Erythrocytes infected by Plasmodium falciparum tend to form clumps - rosettes - and these have been linked to pathology caused by vascular occlusion. This rosette formation may be inhibted by heparin. This agent has been used in the past as part of the treatment of malaria but was abandoned because of an increased risk of haemorrhage. Low molecular weight heparin also disrupts rosette formation and may have a lower risk of bleeding in malaria.[17]
Merozoites
The budding of the merozoites from interconnected cytoplasmic masses (pseudocytomeres) is a complex process. At the tip of each bud a thickened region of pellicle gives rise to the apical rings and conoid. As development proceeds an aggregation of smooth membranes and the nucleus enter the base of the bud. The cytoplasm contains numerous large ribosomes. Synchronous multiple cytoplasmic cleavage of the mature schizont results in the formation of numerous uninucleate merozoites.
Escape of the merozoites from the erythrocyte has also been studied.[18] The erythrocyte swells under osmotic pressure. A pore opens in the erythrocte membrane and 1-2 meorozites escape. This is followed by an eversion the entire erythrocyte membrane, an action that propels the merozoites into the blood stream.
Invasion of erythrocyte precursors has only recently been studied.[19] The earliest stage susceptible to infection were the orthoblasts - the stage immediately preceding the reticulocyte stage which in turn is the immediate precursor to the mature erythrocyte. Invasion of the erythrocyte is inhibited by angiotensin 2[20] Angiotensin 2 is normally metabolized by erythrocytes to angiotensin (Ang) IV and Ang-(1-7). Parasite infection decreased the Ang-(1-7) levels and completely abolished Ang IV formation. Ang-(1-7), like its parent molecule, is capable of decreasing the level of infection. The mechanism of inhibition seems likely to be an inhibition of protein kinase A activity within the erythrocyte.
Placental malaria
More than a hundred late-stage trophozoites or early schizont infected erythrocytes of P. falciparum in a case of placental malaria of a Tanzanian woman were found to form a nidus in an intervillous space of placenta.[21] While such a concentration of parasites in placental malaria is rare, placental malaria cannot give rise to persistent infection as pregnancy in humans normally lasts only 9 months.
Gametocytes
Most merozoites continue this replicative cycle but some merozoites differentiate into male or female sexual forms (gametocytes) (also in the blood), which are taken up by the female mosquito. This process of differentiation into gametocytes appears to occur in the bone marrow. Five distinct morphological stages have recognised (stages I - V). Female gametocytes are produced about four times as commonly as male. In chonic infections in humans the gametocytes are often the only forms found in the blood. Incidentally the characteristic form of the female gametocytes in Plasmodium falciparum gave rise to this species's name.
Gameteocytes appear in the blood after a number of days post infection. In P. falciparum infections they appear after 7 to 15 days while in others they appear after 1 to 3 days.[22] The ratio of asexual to sexual forms is between 10:1 and 156:1[23][24] The half life of the gametocytes has been estimated to be between 2 and 3 days but some are known to persist for up to four weeks.[25]
Gametocyte carriage is associated with anaemia.[26] Although female gametocytes normally outnumber males this may be reversed in the presence of anaemia.
Gametocyte morphology
The five recognised morphological stages were first described by Field and Shute in 1956.[27]
One constant feature of the gametocytes in all stages that distinguishes them from the asexual forms is the presence of a pellicular complex. This originates in small membranous vesicle observed beneath the gametocyte plasmalemma in late stage I. Its function is not known. The structure itself consists of a subpellicular membrane vacuole. Deep to this is an array of longitudinally oriented microtubules. This structure is likely to be relatively inflexible and may help to explain the lack of amoeboid forms observed in asexual parasites.
Early stage one gametoctyes are very difficult to distinguish from small round trophozoites. Later stages can be distinguished by the distribution of pigment granulues. Under the electrom microscope the formation of the subpellicular membrane and a smooth plasma membrane are recognisable. The nuclei are recognisably dimorphic into male and female. These forms may be found between day 0 and day 2 in P falciparum infections.
In stage two the gametocyte enlarges and becomes D shaped. The nucleus may occupy a terminal end of the cell or lie along its length. Early spindle formation may be visible. These forms are found between day 1 to day 4 in P falciparum infections.
In stage three the erythrocyte becomes distorted. A staining difference between the male and female gametoctyes is apparent (male stain pink while female stain faint blue with the usual stains). The male nucleus is noticeably larger than the female and more lobulated. The female cytoplasm has more ribosomes, endoplasmic reticulum and mitochondria.
In stage four the erythrocyte is clearly deformed and the gametocyte is elongated. The male gametocytes stain red while the female stain violet blue. In the male pigment granules are scattered while in the female they are more dense. In the male the kinetochores of each chromosome are located over a nuclear pore. Osmophilic bodies are found in both but are more numerous in the female. These forms are found between day 6 and day 10 in P falciparum infections.
In stage five the gametocytes are clearly recognisable on light microscopy with the typical banana shaped female gametocytes. The subpellicular microtubules depolymerise but the membrane itself remains. In the male gametocyte exhibit the is a dramatic reduction in ribosomal density. Very few mitochondria are retained and the nucleus enlarges with a kinetochore complex attached to the nuclear envelope. In the female gametocytes there are numerous mitochondria, ribosomes and osmophillic bodies. The nucleus is small with a transcription factory.
Stages other than stage five are not normally found in the periferal blood. For reasons not yet understood stages I to IV are sequestered preferentially in the bone marrow and spleen. Stage V gametocytes only become infectious to mosquitoes after a further two or three days of circulation.
Infection of mosquito
In the mosquito's midgut, the gametocytes develop into gametes and fertilize each other, forming motile zygotes called ookinetes. It has been shown that up to 50% of the ookinetes may undergo apoptosis within the midgut.[28][29] The reason for this behavior is unknown. While in the mosquito gut the parasites form thin cytoplasmic extensions to communicate with each other.[30] These structures persist from the time of gametocyte activation until the zygote transforms into an ookinete. The function of these tubular structres remains to be discovered.
The ookinetes penetrate and escape the midgut, then embed themselves onto the exterior of the gut membrane. As in the liver the parasite tends to invade a number of cells before choosing one to reside in. The reason for the behavior is not known. Here they divide many times to produce large numbers of tiny elongated sporozoites. These sporozoites migrate to the salivary glands of the mosquito where they are injected into the blood and subcutaneous tissue of the next host the mosquito bites.
The escape of the gametocytes from the erythrocytes has been until recently obscure.[31] The parasitophorous vacuole membrane ruptures at multiple sites within less than a minute following ingestion. This process may be inhibited by cysteine protease inhibitors. After this rupture of the vacoule the subpellicular membrane begins to disintegrate. This process also can be inhibited by aspartic and the cysteine/serine protease inhibitors. Approximately 15 minutes post-activation, the erythrocyte membrane ruptures at a single breaking point a third process that can be interrupted by protease inhibitors.
Infection of the mosquito has noticeable effects on the host. The presence of the parasite induces apotosis of the egg follicles.[32]
Discussion
The pattern of alternation of sexual and asexual reproduction which may seem confusing at first is a very common pattern in parasitic species. The evolutionary advantages of this type of life cycle were recognised by Gregor Mendel.
Under favourable conditions asexual reproduction is superior to sexual as the parent is well adapted to its environment and its descendents share these genes. Transferring to a new host or in times of stress, sexual reproduction is generally superior as this produces a shuffling of genes which on average at a population level will produce individuals better adapted to the new environment.
The advantages to asexual reproduction within a host can be seen from this simple model taken from Cook.[33] The proportion of hosts that are parasitised is assumed to be small. This being the case the Poisson distribution is a reasonable model. If the parasite is self fertilizing then the chance of successful reproduction is 1 - e-m where m is the proportion of the population parasitised. If the parasite is a faculative bisexual one - one that requires the presence of another parasite on the same host the likelyhood of success is 1 - (1 + m)e-m. If the parasite has two distinct sexes and requires both for reproduction, then the chance of success is ∑ (1 - 21-n)(mn/n!e-m) where the sum is taken between n = 2 and infinity. If m = 0.1 then the chance of success of the self fertilizing parasite is 40 times that of one with distinct sexes. The chance of success of the bisexual parasite is twice that of the parasite with distinct sexes. For smaller values of m, the advantages of self fertilization are even greater.
Given that this parasite spends part of its life cycle in two different hosts it must use a proportion of its available resources within each host. The proportion utilized is currently unknown. Empiracal estimates of this parameter are desirable for modeling of its life cycle.
Dormant forms
Plasmodium falciparum malaria
A report of P. falciparum malaria in a patient with sickle cell anemia four years after exposure to the parasite has been published.[34] A second report that P. falciparum malaria had become symptomatic eight years after leaving an endemic area has also been published.[35]
A third case of an apparent recurrence nine years after leaving an endemic area of P. falciparum malaria has now been reported.[36] A fourth case of recurrence in a patient with lung cancer has been reported.[37] Two cases in pregnant women both from Africa but who had not lived there for over a year have been reported.[38]
A case of congenital malaria due to both P. falciparum and P. malariae has been reported in a child born to a woman from Ghana, a malaria endemic area, despite the mother having emigrated to Austria eighteen months before and never having returned.[39] A second case of congenital malaria in twins due to P. falciparum has been reported.[40] The mother had left Togo 14 months before the diagnosis, had not returned in the interim and was never diagnosed with malaria during her pregnancy.
One case of malaria has been reported in a man of African origin with sickle cell trait who was treated for B cell lymphoma with chemotherapy and an autologous bone marrow transplant.[41] He developed symptomatic malaria only after a subsequent splenectomy performed for worsening disease. Pre treatment blood films and antigen testing were negative.
It seems that at least occasionally P. falciparum has a dormant stage. If this is in fact the case, eradication or control of this organism may be more difficult than previously believed.
Drug induced
Developmental arrest was induced by in vitro culture of P. falciparum in the presence of sub lethal concentrations of artemisinin.[42] The drug induces a subpopulation of ring stages into developmental arrest. At the molecular level this is associated with overexpression of heat shock and erythrocyte binding surface proteins with the reduced expression of a cell-cycle regulator and a DNA biosynthesis protein.
The schizont stage-infected erythrocyte in an experimental culture of P. falciparum, F32 was suppressed to a low level with the use of atovaquone.[43] The parasites resumed growth several days after the drug was removed from the culture.
Biological refuges
Macrophages containing merozoites dispersed in their cytoplasm, called 'merophores', were observed in P. vinckei petteri - an organism that causes murine malaria.[44] Similar merophores were found in the polymorph leukocytes and macrophages of other murine malaria parasite, P. yoelii nigeriensis[44] and P. chabaudi chabaudi. All these species unlike P. falciparum are known to produce hyponozoites that may cause a relapse. The finding of Landau et al.[44] on the presence of malaria parasites inside lymphatics suggest a mechanism for the recrudescence and chronicity of malaria infection.[45]
Evolution
As of 2007[update], DNA sequences are available from less than sixty species of Plasmodium and most of these are from species infecting either rodent or primate hosts. The evolutionary outline given here should be regarded as speculative, and subject to revision as more data becomes available.
Apicomplexa
The Apicomplexa (the phylum to which Plasmodium belongs) are thought to have originated within the Dinoflagellates — a large group of photosynthetic protists. It is thought that the ancestors of the Apicomplexa were originally prey organisms that evolved the ability to invade the intestinal cells and subsequently lost their photosynthetic ability.[46] Many of the species within the Apicomplexia still possess plastids (the organelle in which photosynthesis occurs in photosynthetic eukaryotes), and some that lack plastids nonetheless have evidence of plastid genes within their genomes. In the majority of such species, the plastids are not capable of photosynthesis. Their function is not known, but there is suggestive evidence that they may be involved in reproduction.
Some extant dinoflagellates, however, can invade the bodies of jellyfish and continue to photosynthesize, which is possible because jellyfish bodies are almost transparent. In host organisms with opaque bodies, such an ability would most likely rapidly be lost. The 2008 description of a photosynthetic protist related to the Apicomplexia with a functional plastid supports this hypothesis.[47]
A recently identified apicomplexan found in Australian corals - Chromera velia - has retained a photosynthetic plastid.[48]
An alternative to the ingestion hypothesis is that the ancestor of this group was a predator like Colpodella that uses myzocytosis as its feeding mechanism instead invaded the prey cells instead of ingesting them.
Plasmodium genus
Current (2007) theory suggests that the genera Plasmodium, Hepatocystis and Haemoproteus evolved from one or more Leucocytozoon species. Parasites of the genus Leucocytozoan infect white blood cells (leukocytes) and liver and spleen cells, and are transmitted by 'black flies' (Simulium species) — a large genus of flies related to the mosquitoes.
It is thought that Leucocytozoon evolved from a parasite that spread by the orofaecal route and which infected the intestinal wall. At some point this parasite evolved the ability to infect the liver. This pattern is seen in the genus Cryptosporidium, to which Plasmodium is distantly related. At some later point this ancestor developed the ability to infect blood cells and to survive and infect mosquitoes. Once vector transmission was firmly established, the previous orofecal route of transmission was lost.
The pattern of orofaecal transmission with coincidental infection of the erythrocytes is seen in the genus Schellackia. Species in this genus infect lizards. The usual route of transmission is orofaecal but the parasites can also infect erythrocytes if they traverse the intestinal wall. The infected erythrocytes may be ingested by mites. These infected mites may subsequently be eaten by other uninfected lizards whereupon the parasites emerge and infect these new hosts. Unlike Plasmodium no development occurs in the mite.
Molecular evidence suggests that a reptile - specifically a squamate - was the first vertebrate host of Plasmodium. Birds were the second vertebrate hosts with mammals being the most recent group of vertebrates infected.[49]
Leukocytes, hepatocytes and most spleen cells actively phagocytose particulate matter, which makes the parasite's entry into the cell easier. The mechanism of entry of Plasmodium species into erythrocytes is still very unclear, as it takes place in less than 30 seconds. It is not yet known if this mechanism evolved before mosquitoes became the main vectors for transmission of Plasmodium.
The genus Plasmodium evolved (presumably from its Leucocytozoon ancestor) about 130 million years ago, a period that is coincidental with the rapid spread of the angiosperms (flowering plants). This expansion in the angiosperms is thought to be due to at least one gene duplication event. It seems probable that the increase in the number of flowers led to an increase in the number of mosquitoes and their contact with vertebrates.
Vectors
Mosquitoes evolved in what is now South America about 230 million years ago. There are over 3500 species recognized, but to date their evolution has not been well worked out, so a number of gaps in our knowledge of the evolution of Plasmodium remain. There is evidence of a recent expansion of Anopheles gambiae and Anopheles arabiensis populations in the late Pleistocene in Nigeria.[50]
The reason why a relatively limited number of mosquitoes should be such successful vectors of multiple diseases is not yet known. It has been shown that, among the most common disease-spreading mosquitoes, the symbiont bacterium Wolbachia are not normally present.[51] It has been shown that infection with Wolbachia can reduce the ability of some viruses and Plasmodium to infect the mosquito, and that this effect is Wolbachia-strain specific.
Classification
Taxonomy
Plasmodium belongs to the family Plasmodiidae (Levine, 1988), order Haemosporidia and phylum Apicomplexa. There are currently 450 recognised species in this order. Many species of this order are undergoing reexamination of their taxonomy with DNA analysis.[citation needed] It seems likely that many of these species will be re-assigned after these studies have been completed.[52][53] For this reason the entire order is outlined here.
Order Haemosporida
Family Haemoproteidae
- Genus Haemocystidium Castellani and Willey 1904, emend. Telford 1996
- Genus Haemoproteus
- Subgenus Parahaemoproteus
- Subgenus Haemoproteus
Family Garniidae
- Genus Fallisia Lainson, Landau & Shaw 1974
- Subgenus Fallisia
- Subgenus Plasmodioides
- Genus Garnia
- Genus Progarnia
Family Leucocytozoidae
- Genus Leucocytozoon
- Subgenus Leucocytozoon
- Subgenus Akiba
Family Plasmodiidae
- Genus Plasmodium
- Subgenus Asiamoeba Telford 1988
- Subgenus Bennettinia Valkiūnas 1997
- Subgenus Carinamoeba Garnham 1966
- Subgenus Giovannolaia Corradetti, Garnham & Laird 1963
- Subgenus Haemamoeba Grassi & Feletti 1890
- Subgenus Huffia Garnham & Laird 1963
- Subgenus Lacertaemoba Telford 1988
- Subgenus Laverania Bray 1963
- Subgenus Novyella Corradetti, Garnham & Laird 1963
- Subgenus Ophidiella Garnham 1966
- Subgenus Plasmodium Bray 1963 emend. Garnham 1964
- Subgenus Paraplasmodium Telford 1988
- Subgenus Sauramoeba Garnham 1966
- Subgenus Vinckeia Garnham 1964
- Genus Polychromophilus
- Genus Rayella
- Genus Saurocytozoon
Phylogenetic trees
The relationship between a number of these species can be seen on the Tree of Life website. Perhaps the most useful inferences that can be drawn from this phylogenetic tree are:
- P. falciparum and P. reichenowi (subgenus Laverania) branched off early in the evolution of this genus
- The genus Hepatocystis is nested within (paraphytic with) the genus Plasmodium
- The primate (subgenus Plasmodium) and rodent species (subgenus Vinckeia) form distinct groups
- The rodent and primate groups are relatively closely related
- The lizard and bird species are intermingled
- Although Plasmodium gallinaceum (subgenus Haemamoeba) and Plasmodium elongatum (subgenus Huffia) appear be related here there are so few bird species (three) included, this tree may not accurately reflect their real relationship.
- While no snake parasites have been included these are likely to group with the lizard-bird division
While this tree contains a considerable number of species, DNA sequences from many species in this genus have not been included - probably because they are not available yet. Because of this problem, this tree and any conclusions that can be drawn from it should be regarded as provisional.
Three additional trees are available from the American Museum of Natural History.
These trees agree with the Tree of Life. Because of their greater number of species in these trees, some additional inferences can be made:
- The genus Hepatocystis appears to lie within the primate-rodent clade[54]
- The genus Haemoproteus appears lie within the bird-lizard clade
- The trees are consistent with the proposed origin of Plasmodium from Leucocytozoon
It is also known that the species infecting humans do not form a single clade.[55] In contrast, the species infecting Old World monkeys seem to form a clade. Plasmodium vivax may have originated in Asia and the related species Plasmodium simium appears to be derived through a transfer from the human P. vivax to New World monkey species in South America. This occurred during an indepth study of Howler Monkeys near São Paulo, Brasil.[56]
Another tree concetrating on the species infecting the primates is available here: PLOS site
This tree shows that the 'African' (P. malaria and P. ovale) and 'Asian' (P.cynomogli, P. gonderi, P. semiovale and P. simium) species tend to cluster together into separate clades. P. vivax clusters with the 'Asian' species. The rodent species (P. bergei, P. chabaudi and P. yoelli) form a separate clade. As usual P. falciparum does not cluster with any other species. The bird species (P. juxtanucleare, P. gallinaceum and P. relictum) form a clade that is related to the included Leucocytozoon and Haemoproteus species.
A second tree can be found on the PLoS website: PLOS site This tree concentrates largely on the species infecting primates.
The three bird species included in this tree (P. gallinacium, P. juxtanucleare and P. relictum) form a clade.
Four species (P. billbrayi, P. billcollinsi, P. falciparum and P. reichenowi) form a clade within the subgenus Lavernia. This subgenus is more closely related to the other primate species than to the bird species or the included Leuocytozoan species. Both P. billbrayi and P. billcollinsi infect both the chimpanzee subspecies included in this study (Pan troglodytes troglodytes and Pan troglodytes schweinfurthii). P. falciparum infects the bonbo (Pan paniscus) and P. reichenowi infects only one subspecies (Pan troglodytes troglodytes).
The eleven 'Asian' species included here form a clade with P. simium and P. vivax being clearly closely related as are P. knowseli and P. coatneyi; similarly P. brazillium and P. malariae are related. P. hylobati and P. inui are closely related. P. fragile and P. gonderi appear to be more closely related to P. vivax than to P. malariae.
P. coatneyi and P. inui appear to be closely related to P. vivax.[54]
P. ovale is more closely related to P. malariae than to P. vivax.
Within the 'Asian' clade are three unnamed potential species. One infects each of the two chimpanzee subspecies included in the study (Pan troglodytes troglodytes and Pan troglodytes schweinfurthii). These appear to be related to the P. vivax/P. simium clade.
Two unnamed potential species infect the bonbo (Pan paniscus) and these are related to the P. malariae/P. brazillium clade.
Notes
An analysis of ten 'Asian' species (P. coatneyi, P. cynomolgi, P. fieldi, P. fragile, P. gonderi, P. hylobati, P. inui, P. knowlesi, P. simiovale and P. vivax) suggests that P. coatneyi and P. knowlesi are closely related and that P. fragile is the species most closely related to these two.[57] P. vivax and P. cynomolgi appear to be related.
Unlike other eukaryotes studied to date Plasmodium species have two or three distinct SSU rRNA (18S rRNA) molecules encoded within the genome.[58] These have been divided into types A, S and O. Type A is expressed in the asexual stages; type S in the sexual and type O only in the oocyte. Type O is only known to occur in Plasmodium vivax at present. The reason for this gene duplication is not known but presumably reflects an adaption to the different environments the parasite lives within.
The Asian simian Plasmodium species - Plasmodium coatneyi, Plasmodium cynomolgi, Plasmodium fragile, Plasmodium inui, Plasmodium fieldi, Plasmodium hylobati and Plasmodium simiovale - have a single S-type-like gene and several A-type-like genes. It seems likely that these species form a clade within the subgenus Plasmodium.
Analysis of the merozoite surface protein in ten species of the Asian clade suggest that this group diversified between 3 and 6.3 million years ago - a period that coincided with the radiation of the macques within South East Asia.[59] The inferred branching order differs from that found from the analysis of other genes suggesting that this phylogenetic tree may be difficult to resolve. Positive selection on this gene was also found.
P. vivax appears to have evolved between 45,000 and 82,000 years ago from a species that infects south east Asian macques.[60] This is consistent with the other evidence of a south eastern origin of this species.
It has been reported that the C terminal domain of the RNA polymerase 2 in the primate infecting species (other than P. falciparum and probably P. reichenowei) appears to be unusual[61] suggesting that the classification of species into the subgenus Plasmodium may have an evolutionary and biological basis.
A report of a new species that clusters with P. falciparum and P. reichenowi in chimpanzees has been published, although to date the species has been identified only from the sequence of its mitochondrion.[62] Further work will be needed to describe this new species, however, it appears to have diverged from the P. falciparum- P. reichenowi clade about 21 million years ago. A second report has confirmed the existence of this species in chimpanzees.[63] This report has also shown that P. falciparum is not a uniquely human parasite as had been previously believed. A third report of P. falciparum has been published.[64] This study investigated two mitochondrial genes (cytB and cox1), one plastid gene (tufA), and one nuclear gene (ldh) in 12 chimpanzees and two gorillas from Cameroon and one lemur from Madagascar. Plasmodium falciparum was found in one gorilla and two chimpanzee samples. Two chimpanzee samples tested positive for Plasmodium ovale and one for Plasmodium malariae. Additionally one chimpanzee sample showed the presence of P. reichenowi and another P. gaboni. A new species - Plasmodium malagasi - was provisionally identified in the lemur. This species seems likely to belong to the Vinckeia subgenus but further work is required.
A study of ~3000 wild ape specimens collected from Central Africa has shown that Plasmodium infection is common and is usually with multiple species.[65] The ape species included in the study were western gorillas (Gorilla gorilla), eastern gorillas (Gorilla beringei), bonobos (Pan paniscus) and chimpanzees (Pan troglodytes). 99% of the strains fell into six species within the subgenus Laverina. P. falciparum formed a monophyletic lineage within the gorilla parasite radiation suggesting an origin in gorrilas rather than chimpanzees.
It has been shown that P. falciparum forms a clade with the species P reichenowi.[66] This clade may have originated between 3 million and 10000 years ago. It is proposed that the origin of P. falciparum may have occurred when its precursors developed the ability to bind to sialic acid Neu5Ac possibly via erythrocyte binding protein 175. Humans lost the ability to make the sialic acid Neu5Gc from its precursor Neu5Ac several million years ago and this may have protected them against infection with P. reichenowi.
The dates of the evolution of the species within the subgenus Laverania have been estimated as follows:[67] Laverania: 12.0 million years ago (Mya) (95% estimated range: 6.0 - 19.0 Mya)
P. falciparum in humans: 0.2 Mya (range: 0.078 - 0.33 Mya)
P. falciparum in Pan paniscus: 0.77 Mya (range: 0.43 - 1.6 Mya)
P. falciparum in humans and Pan paniscus: 0.85 Mya (0.46 - 1.3 Mya)
P. reichenowi - P. falciparum in Pan paniscus: 2.2 Mya (range: 1.0 - 3.1 Mya) nd that P. reichenowi - 1.8 Mya (range: 0.6 - 3.2 Mya)
P. billbrayi - 1.1 Mya (range: 0.52 - 1.7 Mya) lciparum P. billcollinsi - 0.97 Mya (range: 0.38 - 1.7 Mya)
Another estimation of the date of evolution of this genus based upon the mutation rate in the cytochrome b gene places the evolution of P. falciparum at 2.5 Mya.[68] The authors also estimated that the mammalian species of this genus evolved 12.8 Mya and that the order Haemosporida evolved 16.2 Mya. While the date of evolution of P. falciparum is consistent with alternative methods, the other two dates are considerably more recent than other published estimates and probably should be treated with caution.
Plasmodium ovale has recently been shown to consist of two cocirculating species - Plasmodium ovale curtisi and Plasmodium ovale wallikeri.[69] These two species can only be distinguished by genetic means and they separated between 1.0 and 3.5 million years ago.
A recently (2009) described species (Plasmodium hydrochaeri) that infects capybaras (Hydrochaeris hydrochaeris) may complicate the phylogentics of this genus.[70] This species appears to be most similar to Plasmodium mexicanum a lizard parasite. Further work in this area seems indicated.
Subgenera
The full taxonomic name of a species includes the subgenus but this is often omitted. The full name indicates some features of the morphology and type of host species. Sixteen subgenera are currently recognised.
The avian species were discovered soon after the description of P. falciparum and a variety of generic names were created. These were subsequently placed into the genus Plasmodium although some workers continued to use the genera Laverinia and Proteosoma for P. falciparum and the avian species respectively. The 5th and 6th Congresses of Malaria held at Istanbul (1953) and Lisbon (1958) recommended the creation and use of subgenera in this genus. Laverinia was applied to the species infecting humans and Haemamoeba to those infecting lizards and birds. This proposal was not universally accepted. Bray in 1955 proposed a definition for the subgenus Plasmodium and a second for the subgenus Laverinia in 1958. Garnham described a third subgenus - Vinckeia - in 1964.
Mammal infecting species
Two species in the subgenus Laverania are currently recognised: P. falciparum and P. reichenowi. Three additional species - Plasmodium billbrayi, Plasmodium billcollinsi and Plasmodium gaboni - may also exist (based on molecular data) but a full description of these species have not yet been published.[67][71] The presence of elongated gametocytes in several of the avian subgenera and in Laverania in addition to a number of clinical features suggested that these might be closely related. This is no longer thought to be the case.
The type species is Plasmodium falciparum.
Species infecting monkeys and apes (the higher primates) other than those in the subgenus Laverania are placed in the subgenus Plasmodium. The position of the recently described Plasmodium GorA and Plasmodium GorB has not yet been settled.[63] The distinction between P. falciparum and P. reichenowi and the other species infecting higher primates was based on the morphological findings but have since been confirmed by DNA analysis.
The type species is Plasmodium malariae.
Parasites infecting other mammals including lower primates (lemurs and others) are classified in the subgenus Vinckeia. Vinckeia while previously considered to be something of a taxonomic 'rag bag' has been recently shown - perhaps rather surprisingly - to form a coherent grouping.
The type species is Plasmodium bubalis.
Bird infecting species
The remaining groupings are based on the morphology of the parasites. Revisions to this system are likely to occur in the future as more species are subject to analysis of their DNA.
The four subgenera Giovannolaia, Haemamoeba, Huffia and Novyella were created by Corradetti et al. for the known avian malarial species.[72] A fifth—Bennettinia—was created in 1997 by Valkiunas.[73] The relationships between the subgenera are the matter of current investigation. Martinsen et al. 's recent (2006) paper outlines what is currently (2007) known.[74] The subgenera Haemamoeba, Huffia, and Bennettinia appear to be monphylitic. Novyella appears to be well defined with occasional exceptions. The subgenus Giovannolaia needs revision.[75]
P. juxtanucleare is currently (2007) the only known member of the subgenus Bennettinia.
Nyssorhynchus is an extinct subgenus of Plasmodium. It has one known member - Plasmodium dominicum
Reptile infecting species
Unlike the mammalian and bird malarias those species (more than 90 currently known) that infect reptiles have been more difficult to classify.
In 1966 Garnham classified those with large schizonts as Sauramoeba, those with small schizonts as Carinamoeba and the single then known species infecting snakes (Plasmodium wenyoni) as Ophidiella.[76] He was aware of the arbitrariness of this system and that it might not prove to be biologically valid. Telford in 1988 used this scheme as the basis for the currently accepted (2007) system.[77]
These species have since been divided in to 8 genera - Asiamoeba, Carinamoeba, Fallisia, Garnia, Lacertamoeba, Ophidiella, Paraplasmodium and Sauramoeba. Three of these genera (Asiamoeba, Lacertamoeba and Paraplasmodium) were created by Telford in 1988. Another species (Billbraya australis) described in 1990 by Paperna and Landau and is the only known species in this genus. This species may turn out to be another subgenus of lizard infecting Plasmodium.
Classification criteria for subgenera
Bird infecting species
There are ~40 recognised bird species. Although over 50 species have been described, several have been rejected as being invalid.
With the exception of P. elongatum the exoerythrocytic stages occur in the endothelial cells and those of the macrophage-lymphoid system. The exoerythrocytic stages of P. elongatum parasitise the blood forming cells.
The various subgenera are first distinguished on the basis of the morphology of the mature gametocytes. Those of subgenus Haemamoeba are round or oval while those of the subgenera Giovannolaia, Huffia and Novyella are elongated. These latter genera are distinguished on the basis of the size of the schizonts: Giovannolaia and Huffia have large schizonts while those of Novyella are small.
Species in the subgenus Bennettinia have the following characteristics:
The type species is Plasmodium juxtanucleare.
Species in the subgenus Giovannolaia have the following characteristics:
- Schizonts contain plentiful cytoplasm, are larger than the host cell nucleus and frequently displace it. They are found only in mature erythrocytes.
- Gametocytes are elongated.
- Exoerythrocytic schizogony occurs in the mononuclear phagocyte system.
The type species is Plasmodium circumflexum.
Species in the subgenus Haemamoeba have the following characteristics:
- Mature schizonts are larger than the host cell nucleus and commonly displace it.
- Gametocytes are large, round, oval or irregular in shape and are substantially larger than the host nucleus.
The type species is Plasmodium relictum.
Species in the subgenus Huffia have the following characteristics:
- Mature schizonts, while varying in shape and size, contain plentiful cytoplasm and are commonly found in immature erthryocytes.
- Gametocytes are elongated.
The type species is Plasmodium elongatum.
Species in the subgenus Novyella have the following characteristics:
- Mature schizonts are either smaller than or only slightly larger than the host nucleus. They contain scanty cytoplasm.
- Gametocytes are elongated. Sexual stages in this subgenus resemble those of Haemoproteus.
- Exoerythrocytic schizogony occurs in the mononuclear phagocyte system
The type species is Plasmodium vaughani.
Reptile infecting species
All species in these subgenera infect lizards.
Species in the subgenus Asiamoeba have the following characteristics:
Species in the subgenus Carinamoeba have the following characteristics:
- Schizonts normally give rise to less than 8 merozoites
- Schizonts are normally smaller than the host nucleus
The type species is Plasmodium minasense.
Species in the subgenus Fallisia have the following characteristics:
- Non-pigmented asexual and gametocyte forms are found in leukocytes and thrombocytes
Species in the subgenus Garnia have the following characteristics:
- Pigment is absent
Species in the subgenus Lacertaemoba have the following characteristics:
Species in the subgenus Paraplasmodium have the following characteristics:
Species in the subgenus Sauramoeba have the following characteristics:
- Schizonts normally give rise to more than 8 merozoites
- Schizonts are normally larger than the host nucleus
- Non-pigmented gametocytes are typically the only forms found
- Pigmented forms may be found in the leukocytes occasionally
The type species is Plasmodium agamae.
All species in Ophidiella infect snakes
The type species is Plasmodium weyoni.
Notes
- The erythrocytes of both reptiles and birds retain their nucleus, unlike those of mammals. The reason for the loss of the nucleus in mammalian erythocytes remains unknown.
Species listed by subgenera
The listing given here by subgenus is incomplete. A full listing of the species is avilable at Plasmodium species.
- Asiamoeba
- Plasmodium clelandi
- Plasmodium draconis
- Plasmodium lionatum
- Plasmodium saurocordatum
- Plasmodium vastator
- Bennetinia
- Plasmodium juxtanucleare
- Carinamoeba
- Plasmodium basilisci
- Plasmodium clelandi
- Plasmodium lygosomae
- Plasmodium mabuiae
- Plasmodium minasense
- Plasmodium rhadinurum
- Plasmodium volans
- Giovannolaia
- Plasmodium anasum
- Plasmodium circumflexum
- Plasmodium dissanaikei
- Plasmodium durae
- Plasmodium fallax
- Plasmodium formosanum
- Plasmodium gabaldoni
- Plasmodium garnhami
- Plasmodium gundersi
- Plasmodium hegneri
- Plasmodium lophurae
- Plasmodium pedioecetii
- Plasmodium pinnotti
- Plasmodium polare
- Haemamoeba
- Plasmodium cathemerium
- Plasmodium coggeshalli
- Plasmodium coturnixi
- Plasmodium elongatum
- Plasmodium gallinaceum
- Plasmodium giovannolai
- Plasmodium lutzi
- Plasmodium matutinum
- Plasmodium paddae
- Plasmodium parvulum
- Plasmodium relictum
- Plasmodium tejera
- Huffia
- Plasmodium elongatum
- Plasmodium hermani
- Lacertamoeba
- Laverania
- Plasmodium billbrayi
- Plasmodium billcollinsi
- Plasmodium falciparum
- Plasmodium gaboni
- Plasmodium reichenowi
- Ophidiella
- Novyella
- Plasmodium ashfordi
- Plasmodium bertii
- Plasmodium bambusicolai
- Plasmodium columbae
- Plasmodium corradettii
- Plasmodium dissanaikei
- Plasmodium globularis
- Plasmodium hexamerium
- Plasmodium jiangi
- Plasmodium kempi
- Plasmodium lucens
- Plasmodium megaglobularis
- Plasmodium multivacuolaris
- Plasmodium nucleophilum
- Plasmodium papernai
- Plasmodium parahexamerium
- Plasmodium paranucleophilum
- Plasmodium rouxi
- Plasmodium vaughani
- Nyssorhynchus
- Plasmodium dominicum
- Paraplasmodium
- Plasmodium
- Plasmodium bouillize
- Plasmodium brasilianum
- Plasmodium cercopitheci
- Plasmodium coatneyi
- Plasmodium cynomolgi
- Plasmodium eylesi
- Plasmodium fieldi
- Plasmodium fragile
- Plasmodium georgesi
- Plasmodium girardi
- Plasmodium gonderi
- Plasmodium gora
- Plasmodium gorb
- Plasmodium inui
- Plasmodium jefferyi
- Plasmodium joyeuxi
- Plasmodium knowlesi
- Plasmodium hyobati
- Plasmodium malariae
- Plasmodium ovale
- Plasmodium petersi
- Plasmodium pitheci
- Plasmodium rhodiani
- Plasmodium schweitzi
- Plasmodium semiovale
- Plasmodium semnopitheci
- Plasmodium silvaticum
- Plasmodium simium
- Plasmodium vivax
- Plasmodium youngi
- Sauramoeba
- Plasmodium achiotense
- Plasmodium adunyinkai
- Plasmodium aeuminatum
- Plasmodium agamae
- Plasmodium balli
- Plasmodium beltrani
- Plasmodium brumpti
- Plasmodium cnemidophori
- Plasmodium diploglossi
- Plasmodium giganteum
- Plasmodium heischi
- Plasmodium josephinae
- Plasmodium pelaezi
- Plasmodium zonuriae
- Vinckeia
- Plasmodium achromaticum
- Plasmodium aegyptensis
- Plasmodium anomaluri
- Plasmodium atheruri
- Plasmodium berghei
- Plasmodium booliati
- Plasmodium brodeni
- Plasmodium bubalis
- Plasmodium bucki
- Plasmodium caprae
- Plasmodium cephalophi
- Plasmodium chabaudi
- Plasmodium coulangesi
- Plasmodium cyclopsi
- Plasmodium foleyi
- Plasmodium girardi
- Plasmodium incertae
- Plasmodium inopinatum
- Plasmodium landauae
- Plasmodium lemuris
- Plasmodium melanipherum
- Plasmodium narayani
- Plasmodium odocoilei
- Plasmodium percygarnhami
- Plasmodium pulmophilium
- Plasmodium sandoshami
- Plasmodium traguli
- Plasmodium tyrio
- Plasmodium uilenbergi
- Plasmodium vinckei
- Plasmodium watteni
- Plasmodium yoelli
Host range
Host range among the mammalian orders is non uniform. At least 29 species infect non human primates; rodents outside the tropical parts of Africa are rarely affected; a few species are known to infect bats, porcupines and squirrels; carnivores, insectivores and marsupials are not known to act as hosts.
The listing of host species among the reptiles has rarely been attempted. Ayala in 1978 listed 156 published accounts on 54 valid species and subspecies between 1909 and 1975.[78] The regional breakdown was Africa: 30 reports on 9 species; Australia, Asia & Oceania: 12 reports on 6 species and 2 subspecies; Americas: 116 reports on 37 species.
Because of the number of species parasited by Plasmodium further discussion has been broken down into following pages:
Species reclassified into other genera
The following species have been assigned to the genus Plasmodium in the past:
- Hepatocystis epomophori
- Hepatocystis kochi
- Hepatocystis limnotragi Van Denberghe 1937
- Hepatocystis pteropi Breinl 1911
- Hepatocystis ratufae Donavan 1920
- Hepatocystis vassali Laveran 1905
- Haemoemba praecox
- Haemoemba rousseleti
- Garnia gonatodi
- Fallisia siamense
Species of dubious validity
The following species are currently regarded as questionable validity (nomen dubium).
- Plasmodium bitis
- Plasmodium bowiei
- Plasmodium brucei
- Plasmodium bufoni
- Plasmodium caprea
- Plasmodium carinii
- Plasmodium causi
- Plasmodium chalcidi
- Plasmodium chloropsidis
- Plasmodium centropi
- Plasmodium danilweskyi
- Plasmodium divergens
- Plasmodium effusum
- Plasmodium fabesia
- Plasmodium gambeli
- Plasmodium galinulae
- Plasmodium herodiadis
- Plasmodium limnotragi
- Plasmodium malariae raupachi
- Plasmodium metastaticum
- Plasmodium moruony
- Plasmodium periprocoti
- Plasmodium ploceii
- Plasmodium struthionis
References
- ^ Chavatte J.M., Chiron F., Chabaud A., Landau I. (March 2007). "Probable speciations by "host-vector 'fidelity'": 14 species of Plasmodium from magpies" (in French). Parasite 14 (1): 21–37. PMID 17432055.
- ^ Perkins S.L., Austin C. (September 2008). "Four New Species of Plasmodium from New Guinea Lizards: Integrating Morphology and Molecules". J. Parasitol. 95 (2): 1. doi:10.1645/GE-1750.1. PMID 18823150.
- ^ HHMI Staff (22 January 2006). "Malaria Parasites Develop in Lymph Nodes". HHMI News. Howard Hughes Medical Institute. http://www.hhmi.org/news/menard20060122.html.
- ^ Guilbride DL, Gawlinski P, Guilbride PD (2010). Rodrigues, Mauricio Martins. ed. "Why functional pre-erythrocytic and bloodstage malaria vaccines fail: a meta-analysis of fully protective immunizations and novel immunological model". PloS One 5 (5): e10685. doi:10.1371/journal.pone.0010685. PMC 2873430. PMID 20502667. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2873430.
- ^ Gueirard P, Tavares J, Thiberge S, et al. (October 2010). "Development of the malaria parasite in the skin of the mammalian host". Proc. Natl. Acad. Sci. U.S.A. 107 (43): 18640–5. doi:10.1073/pnas.1009346107. PMC 2972976. PMID 20921402. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2972976.
- ^ Kaiser K, Camargo N, Kappe SH (2003). "Transformation of sporozoites into early exoerythrocytic malaria parasites does not require host cells". J Exp Med 197: 1045–1050.
- ^ Gantt SM, Myung JM, Briones MR, Li WD, Corey EJ et al. (1998). "Proteasome inhibitors block development of Plasmodium spp". Antimicrob Agents Chemother 42: 2731–2738.
- ^ Manson-Bahr PEC, Bell DR, eds. (1987). Manson's Tropical Diseases London: Bailliere Tindall, ISBN 0-7020-1187-8
- ^ Cogswell FB (January 1992). "The hypnozoite and relapse in primate malaria.". Clinical microbiology reviews 5 (1): 26–35. PMC 358221. PMID 1735093. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=358221.
- ^ Krotoski WA, Collins WE, Bray RS, et al. (November 1982). "Demonstration of hypnozoites in sporozoite-transmitted Plasmodium vivax infection.". The American journal of tropical medicine and hygiene 31 (6): 1291–3. PMID 6816080.
- ^ Greenwood BM, Fidock DA, Kyle DE, et al. (April 2008). "Malaria: progress, perils, and prospects for eradication". J. Clin. Invest. 118 (4): 1266–76. doi:10.1172/JCI33996. PMC 2276780. PMID 18382739. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2276780.
- ^ Tanomsing N, Imwong M, Pukrittayakamee S, et al. (October 2007). "Genetic analysis of the dihydrofolate reductase-thymidylate synthase gene from geographically diverse isolates of Plasmodium malariae". Antimicrob. Agents Chemother. 51 (10): 3523–30. doi:10.1128/AAC.00234-07. PMC 2043249. PMID 17682097. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2043249.
- ^ Sturm, A; Amino, R; Van De Sand, C; Regen, T; Retzlaff, S; Rennenberg, A; Krueger, A; Pollok, JM et al.; et al. (2006). "Manipulation of host hepatocytes by the malaria parasite for delivery into liver sinusoids". Science 313 (5791): 1287–1290. doi:10.1126/science.1129720. PMID 16888102.
- ^ Baer, K; Klotz, C; Kappe, SH; Schnieder, T; Frevert, U; et al. (2007). "Release of hepatic Plasmodium yoelii merozoites into the pulmonary microvasculature". PLoS Pathogens 3 (11): e171. doi:10.1371/journal.ppat.0030171. PMC 2065874. PMID 17997605. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2065874.
- ^ Graewe S, Rankin KE, Lehmann C, Deschermeier C, Hecht L, Froehlke U, Stanway RR, Heussler V (2011). "Hostile takeover by Plasmodium: Reorganization of parasite and host cell membranes during liver stage egress". PLoS Pathog 7 (9): e1002224.
- ^ Portugal S, Carret C, Recker M, Armitage AE, Gonçalves LA, Epiphanio S, Sullivan D, Roy C, Newbold CI, Drakesmith H, Mota MM (2011) Host-mediated regulation of superinfection in malaria. Nat Med
- ^ Leitgeb AM, Blomqvist K, Cho-Ngwa F, Samje M, Nde P, Titanji V, Wahlgren M (2011). "Low Anticoagulant heparin disrupts Plasmodium falciparum rosettes in fresh clinical isolates". Am J Trop Med Hyg 84 (3): 390–396. doi:10.4269/ajtmh.2011.10-0256. PMC 3042813. PMID 21363975. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3042813.
- ^ A novel mechanism for malaria parasite egress from the red blood cell. Abkarian M, Massiera G, Berry L, Roques M, Braun-Breton C. Blood.
- ^ Tamez PA, Liu H, Fernandez-Pol S, Haldar K, Wickrema A (October 2009). "Stage-specific susceptibility of human erythroblasts to Plasmodium falciparum malaria infection". Blood 114 (17): 3652–5. doi:10.1182/blood-2009-07-231894. PMC 2766680. PMID 19706885. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2766680.
- ^ Saraiva VB, de Souza Silva L, Ferreira-Dasilva CT, Silva-Filho JL, Teixeira-Ferreira A, Perales J, Souza MC, Henriques MG, Caruso-Neves C et al. (2011). Snounou, Georges. ed. "Impairment of the Plasmodium falciparum erythrocytic cycle induced by angiotensin peptides". PLoS One 6 (2): e17174. doi:10.1371/journal.pone.0017174. PMC 3041794. PMID 21364758. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3041794.
- ^ Muehlenbachs A., Mutabingwa T.K., Fried M., Duffy P.E. (2007) An unusual presentation of placental malaria: A single persisting nidus of sequestered parasites. Hum. Pathol. 38(3): 520-523, PMID 17239927 doi:10.1016/j.humpath.2006.09.016
- ^ Robert V, Boudin C (2003). "Biology of man-mosquito Plasmodium transmission". Bull Soc Pathol Exot. 96 (1): 6–20. PMID 12784587.
- ^ Kitchen SF, Putnam P (1942). "Observations on the mechanism of the parasite cycle in falciparum malaria". Am J Trop Med. 22: 381–386.
- ^ Eichner M, Diebner HH, Molineaux L, Collins WE, Jeffery GM, Dietz K (2001). "Genesis, sequestration and survival of Plasmodium falciparum gametocytes: parameter estimates from fitting a model to malaria therapy data". Trans R Soc Trop Med Hyg 95 (5): 497–501. doi:10.1016/S0035-9203(01)90016-1. PMID 11706658.
- ^ Smalley ME, Sinden RE (1977). "Plasmodium falciparum gametocytes: their longevity and infectivity". Parasitology 74 (1): 1–8. doi:10.1017/S0031182000047478. PMID 320542.
- ^ Gbotosho GO, Sowunmi A, Okuboyejo TM, Happi CT, Michael OS, Folarin OA, Adewoye EO (2011) Plasmodium falciparum gametocyte carriage, emergence, clearance and population sex ratios in anaemic and non-anaemic malarious children. Mem Inst Oswaldo Cruz. 106(5):562-569
- ^ Field JW, Shute PG (1956) A morphological study of the erythrocytic parasites. Kuala Lumpur: Government Press. The microscopic diagnostic of human malaria; p. 142
- ^ Al-Olayana EM, Williamsb GT, Hurd H (2002). "Apoptosis in the malaria protozoan, Plasmodium berghei: a possible mechanism for limiting intensity of infection in the mosquito". Inter. J. Parasitol 32 (9): 1133–1143. doi:10.1016/S0020-7519(02)00087-5.
- ^ Hurd H, Grant KM, Arambage SC (2006). "Apoptosis-like death as a feature of malaria infection in mosquitoes". Parasitology 132 Suppl: S33–47. doi:10.1017/S0031182006000849. PMID 17018164.
- ^ Rupp I, Sologub L, Williamson KC, et al. (December 2010). "Malaria parasites form filamentous cell-to-cell connections during reproduction in the mosquito midgut". Cell Res 21 (4): 683–696. doi:10.1038/cr.2010.176. PMID 21173797.
- ^ Sologub L, Kuehn A, Kern S, Przyborski J, Schillig R, Pradel G (2011) Malaria proteases mediate inside-out egress of gametocytes from red blood cells following parasite transmission to the mosquito. Cell Microbiol. doi: 10.1111/j.1462-5822.2011.01588.x.
- ^ Hopwood JA, Ahmed AM, Polwart A, Williams GT, Hurd H (2001). "Malaria-induced apoptosis in mosquito ovaries: a mechanism to control vector egg production". J. Exp. Biol. 204 (Pt 16): 2773–2780. PMID 11683433.
- ^ Cook LM (1971) Coefficients of natural selection. Hutchinson University Library.
- ^ Greenwood, T.; et al. (2008). "Febrile Plasmodium falciparum malaria four years after exposure in a man with sickle cell disease". Clin. Infect. Dis. 47 (4): e39–e41. doi:10.1086/590250. PMID 18616395.
- ^ Szmitko, P. E.; Kohn, M. L.; Simor, A. E. (2008). "Plasmodium falciparum malaria occurring eight years after leaving an endemic area". Diagn. Microbiol. Infect. Dis. 61 (1): 105–107. doi:10.1016/j.diagmicrobio.2008.08.017. PMID 18945569.
- ^ Theunissen, C.; Mutabingwa, TK; Fried, M; Duffy, PE; Van-Esbroeck, M; Van-Gompel, A; Van-Denende, J (2009). "Falciparum malaria in patient 9 years after leaving malaria-endemic area". Emerg Infect Dis. 15 (1): 115–116. doi:10.3201/eid1501.080909. PMC 2660708. PMID 17239927. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2660708.
- ^ Foca E, Zulli R, Buelli F, De Vecchi M, Regazzoli A, Castelli F (March 2009). "P. falciparum malaria recrudescence in a cancer patient". Le infezioni in medicina: rivista periodica di eziologia, epidemiologia, diagnostica, clinica e terapia delle patologie infettive 17 (1): 33–4. PMID 19359823.
- ^ Poilane I, Jeantils V, Carbillon L (October 2009). "[Pregnancy associated Plasmodium falciparum malaria discovered fortuitously: report of two cases]" (in French). Gynecol Obstet Fertil 37 (10): 824–6. doi:10.1016/j.gyobfe.2009.07.011. PMID 19766039.
- ^ Zenz W, Trop M, Kollaritsch H, Reinthaler (2000). "Congenital malaria due to Plasmodium falciparum and Plasmodium malariae". Wien Klin Wochenschr 112 (10): 459–461. PMID 10890139.
- ^ Romand S, Bourée P, Gelez J, Bader-Meunier B, Bisaro F, Dommergues JP (1994). "Congenital malaria. A case observed in twins born to an asymptomatic mother". Presse Med 23 (17): 797–800. PMID 8078837.
- ^ Linares M, Albizua E, Méndez D, Rubio JM, Martínez-Serna A, Martínez MA, Salto E, Puyet A, Diez A, Martinez-López J, Bautista JM (2011) Malaria hidden in a patient with diffuse large B-cell lymphoma and sickle cell trait. J Clin Microbiol
- ^ Witkowski B, Lelièvre J, Barragán MJ, et al. (May 2010). "Increased tolerance to artemisinin in Plasmodium falciparum is mediated by a quiescence mechanism". Antimicrob. Agents Chemother. 54 (5): 1872–7. doi:10.1128/AAC.01636-09. PMC 2863624. PMID 20160056. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2863624.
- ^ Thapar MM, Gil JP, Björkman A (January 2005). "In vitro recrudescence of Plasmodium falciparum parasites suppressed to dormant state by atovaquone alone and in combination with proguanil". Trans. R. Soc. Trop. Med. Hyg. 99 (1): 62–70. doi:10.1016/j.trstmh.2004.01.016. PMID 15550263.
- ^ a b c Landau I, Chabaud AG, Mora-Silvera E, et al. (December 1999). "Survival of rodent malaria merozoites in the lymphatic network: potential role in chronicity of the infection". Parasite (Paris, France) 6 (4): 311–22. PMID 10633501.
- ^ Gautret P (2000). "The Landau and Chabaud's phenomenon". Parasite 7 (1): 57–58. PMID 10743652.
- ^ Moore RB, Oborník M, Janouskovec J, et al. (February 2008). "A photosynthetic alveolate closely related to apicomplexan parasites". Nature 451 (7181): 959–963. doi:10.1038/nature06635. PMID 18288187. http://www.nature.com/nature/journal/v451/n7181/full/nature06635.html.
- ^ Moore RB, Oborník M, Janouskovec J, et al. (February 2008). "A photosynthetic alveolate closely related to apicomplexan parasites". Nature 451 (7181): 959–63. doi:10.1038/nature06635. PMID 18288187.
- ^ Botte CY, Yamaryo-Botte Y, Janouskovec J, Rupasinghe T, Keeling PJ, Crellin P, Coppel R, Marechal E, McConville MJ, McFadden GI (2011) Identification of plant-like galactolipids in Chromera velia, a photosynthetic relative of malaria parasites. J Biol Chem
- ^ Yotoko, KSC; C Elisei (2006-11). "Malaria parasites (Apicomplexa, Haematozoea) and their relationships with their hosts: is there an evolutionary cost for the specialization?". Journal of Zoological Systematics and Evolutionary Research 44 (4): 265–73. doi:10.1111/j.1439-0469.2006.00377.x.
- ^ Matthews SD, Meehan LJ, Onyabe DY, et al. (December 2007). "Evidence for late Pleistocene population expansion of the malarial mosquitoes, Anopheles arabiensis and Anopheles gambiae in Nigeria". Med. Vet. Entomol. 21 (4): 358–69. doi:10.1111/j.1365-2915.2007.00703.x. PMID 18092974. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0269-283X&date=2007&volume=21&issue=4&spage=358.
- ^ Moreira LA, Iturbe-Ormaetxe I, Jeffery JA, Lu G, Pyke AT, Hedges LM, Rocha BC, Hall-Mendelin S, Day A et al. (2009). "A Wolbachia symbiont in Aedes aegypti limits infection with dengue, chikungunya, and Plasmodium". Cell 139 (7): 1268–1278. doi:10.1016/j.cell.2009.11.042. PMID 20064373.
- ^ Perkins SL, Schall JJ (October 2002). "A molecular phylogeny of malarial parasites recovered from cytochrome b gene sequences". J. Parasitol. 88 (5): 972–8. doi:10.1645/0022-3395(2002)088[0972:AMPOMP]2.0.CO;2. ISSN 0022-3395. PMID 12435139.
- ^ Yotoko, K. S. C.; Elisei, C. (2006). "Malaria parasites (Apicomplexa, Haematozoea) and their relationships with their hosts: is there an evolutionary cost for the specialization?". J. Zoo. Syst. Evol. Res. 44 (4): 265. doi:10.1111/j.1439-0469.2006.00377.x.
- ^ a b Seethamchai S, Putaporntip C, Malaivijitnond S, Cui L, Jongwutiwes S (2008). "Malaria and Hepatocystis species in wild macaques, southern Thailand". Am. J. Trop. Med. Hyg. 78 (4): 646–653. PMID 18385364.
- ^ Leclerc M.C., Hugot J.P., Durand P., Renaud F. (2004). "Evolutionary relationships between 15 Plasmodium species from new and old world primates (including humans): an 18S rDNA cladistic analysis". Parasitology 129 (6): 677–684. doi:10.1017/S0031182004006146.
- ^ Plasmodium Simium, Fonseca 1951 1.13 (1951): 153-61.DPDx. Web. 27 Feb. 2010
- ^ Mitsui H, Arisue N, Sakihama N, et al. (January 2010). "Phylogeny of Asian primate malaria parasites inferred from apicoplast genome-encoded genes with special emphasis on the positions of Plasmodium vivax and P. fragile". Gene 450 (1–2): 32–8. doi:10.1016/j.gene.2009.10.001. PMID 19818838.
- ^ Nishimoto Y, Arisue N, Kawai S, Escalante AA, Horii T, Tanabe K, Hashimoto T (2008). "Evolution and phylogeny of the heterogeneous cytosolic SSU rRNA genes in the genus Plasmodium". Mol Phylogenet Evol. 47 (1): 45–53. doi:10.1016/j.ympev.2008.01.031. PMID 18334303.
- ^ Sawai H, Otani H, Arisue N, Palacpac N, de Oliveira Martins L, Pathirana S, Handunnetti S, Kawai S, Kishino H et al. (2010). "Lineage-specific positive selection at the merozoite surface protein 1 (msp1) locus of Plasmodium vivax and related simian malaria parasites". Evol Biol. 10 (1): 52. doi:10.1186/1471-2148-10-52. PMC 2832629. PMID 20167126. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2832629.
- ^ Escalante AA, Cornejo OE, Freeland DE, Poe AC, Durrego E, Collins WE, Lal AA (2005). "A monkey's tale: the origin of Plasmodium vivax as a human malaria parasite". Proc Natl Acad Sci USA 102 (6): 1980–5. doi:10.1073/pnas.0409652102. PMC 548581. PMID 15684081. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=548581.
- ^ Kishore SP, Perkins SL, Templeton TJ, Deitsch KW (June 2009). "An unusual recent expansion of the C-terminal domain of RNA polymerase II in primate malaria parasites features a motif otherwise found only in mammalian polymerases". J. Mol. Evol. 68 (6): 706–14. doi:10.1007/s00239-009-9245-2. PMID 19449052.
- ^ Ollomo B, Durand P, Prugnolle F, et al. (May 2009). Holmes, Edward C.. ed. "A new malaria agent in African hominids". PLoS Pathog. 5 (5): e1000446. doi:10.1371/journal.ppat.1000446. PMC 2680981. PMID 19478877. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2680981.
- ^ a b Prugnolle F, Durand P, Neel C, Ollomo B, Ayala FJ, Arnathau C, Etienne L, Mpoudi-Ngole E, Nkoghe D et al. (2010). "African great apes are natural hosts of multiple related malaria species, including Plasmodium falciparum". Proc. Natl. Acad. Sci. USA 107 (4): 1458–1463. doi:10.1073/pnas.0914440107. PMC 2824423. PMID 20133889. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2824423.
- ^ Duval L, Fourment M, Nerrienet E, et al. (June 2010). "African apes as reservoirs of Plasmodium falciparum and the origin and diversification of the Laverania subgenus". Proc. Natl. Acad. Sci. U.S.A. 107 (23): 10561–6. doi:10.1073/pnas.1005435107. PMC 2890828. PMID 20498054. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2890828.
- ^ Liu W, Li Y, Learn GH, Rudicell RS, Robertson JD, Keele BF, Ndjango JB, Sanz CM, Morgan DB et al. (2010). "Origin of the human malaria parasite Plasmodium falciparum in gorillas". Nature 467 (7314): 420–425. doi:10.1038/nature09442. PMC 2997044. PMID 20864995. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2997044.
- ^ Rich SM, Leendertz FH, Xu G, et al. (September 2009). "The origin of malignant malaria". Proc. Natl. Acad. Sci. U.S.A. 106 (35): 14902–7. doi:10.1073/pnas.0907740106. PMC 2720412. PMID 19666593. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2720412.
- ^ a b Krief S, Escalante AA, Pacheco MA, Mugisha L, André C, Halbwax M, Fischer A, Krief JM, Kasenene JM et al. (2010). Sibley, L. David. ed. "On the Diversity of malaria parasites in African apes and the origin of Plasmodium falciparum from bonobos". PloS Pathog 6 (2): e1000765. doi:10.1371/journal.ppat.1000765. PMC 2820532. PMID 20169187. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2820532.
- ^ Ricklefs RE, Outlaw DC (2010). "A molecular clock for malaria parasites". Science 329 (5988): 226–229. doi:10.1126/science.1188954. PMID 20616281.
- ^ Sutherland CJ, Tanomsing N, Nolder D, Oguike M, Jennison C, Pukrittayakamee S, Dolecek C, Hien TT, do Rosário VE, Arez AP, Pinto J, Michon P, Escalante AA, Nosten F, Burke M, Lee R, Blaze M, Otto TD, Barnwell JW, Pain A, Williams J, White NJ, Day NP, Snounou G, Lockhart PJ, Chiodini PL, Imwong M, Polley SD (2010). "Two nonrecombining sympatric forms of the human malaria parasite Plasmodium ovale occur globally". J Infect Dis 201 (10): 1544–50. doi:10.1086/652240. PMID 20380562.
- ^ dos Santos LC, Curotto SM, de Moraes W, et al. (July 2009). "Detection of Plasmodium sp. in capybara". Vet. Parasitol. 163 (1–2): 148–51. doi:10.1016/j.vetpar.2009.03.042. PMID 19411142.
- ^ Ollomo B, Durand P, Prugnolle F, Douzery E, Arnathau C et al. (2009). Holmes, Edward C.. ed. "A New Malaria Agent in African Hominids". PLoS Pathog 5 (5): e1000446. doi:10.1371/journal.ppat.1000446. PMC 2680981. PMID 19478877. http://www.plospathogens.org/article/info%3Adoi%2F10.1371%2Fjournal.ppat.1000446.
- ^ Corradetti, A.; Garnham, P. C. C.; Laird, M. (1963). "New classification of the avian malaria parasites". Parassitologia 5: 1–4. ISSN 0048-2951.
- ^ Valkiunas G. (1997). Bird Haemosporidia. Institute of Ecology, Vilnius
- ^ Martinsen ES, Waite JL, Schall JJ (April 2007). "Morphologically defined subgenera of Plasmodium from avian hosts: test of monophyly by phylogenetic analysis of two mitochondrial genes". Parasitology 134 (Pt 4): 483–90. doi:10.1017/S0031182006001922. PMID 17147839.
- ^ Martinsen, ES; Waite, JL; Schall, JJ; Waite, J. L.; Schall, J. J. (2007). "Morphologically defined subgenera of Plasmodium from avian hosts: test of monophyly by phylogenetic analysis of two mitochondrial genes". Parasitol. 134 (4): 483–490. doi:10.1017/S0031182006001922. PMID 17147839.
- ^ Garnham P.C.C. (1966) Malaria parasites and other haemospordia. Oxford, Blackwell
- ^ Telford, S. (1988). "A contribution to the systematics of the reptilian malaria parasites, family Plasmodiidae (Apicomplexa: Haemosporina)". Bulletin of the Florida State Museum Biological Sciences 34 (2): 65–96. http://ufdc.ufl.edu/UF00095820.
- ^ Ayala S.C. (1978). "Checklist, host index, and annotated bibliography of Plasmodium from reptiles". J. Euk. Micro 25 (1): 87–100. doi:10.1111/j.1550-7408.1978.tb03874.x.
Further reading
- Standard reference books for the identification of Plasmodium species
- Laird, Marshall (1998). Avian Malaria in the Asian Tropical Subregion. Santa Clara, CA: Springer-Verlag TELOS. ISBN 981-3083-19-0.
- Valkiūnas G. (2004). Avian Malaria Parasites and Other Haemosporidia. CRC Press. ISBN 978-0-415-30097-1.
- Garnham PCC (1966). Malaria Parasites and Other Haemosporidia. Oxford: Blackwell Science Ltd. ISBN 0-632-01770-8.
-
- This book is the standard reference work on malarial species classification even if it a little dated now. A number of additional species have been described since its publication.
- Hewitt R (1942). Bird Malaria. Baltimore, MD: The Johns Hopkins Press.
- Other useful references
- Shortt HE (1951). "Life-cycle of the mammalian malaria parasite". Br. Med. Bull. 8 (1): 7–9. PMID 14944807. http://bmb.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=14944807.
- Baldacci P, Ménard R (October 2004). "The elusive malaria sporozoite in the mammalian host". Mol. Microbiol. 54 (2): 298–306. doi:10.1111/j.1365-2958.2004.04275.x. PMID 15469504. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0950-382X&date=2004&volume=54&issue=2&spage=298.
- Bledsoe GH (December 2005). "Malaria primer for clinicians in the United States". South. Med. J. 98 (12): 1197–204; quiz 1205, 1230. doi:10.1097/01.smj.0000189904.50838.eb. PMID 16440920. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0038-4348&volume=98&issue=12&spage=1197.
External links
Some history of malaria - http://muse.jhu.edu/journals/bulletin_of_the_history_of_medicine/v079/79.2slater.html
Ciliophora Spirotrichea (Stylonychia) · Litostomatea (Didinium, Balantidium) · Phyllopharyngea (Tokophrya) · Nassophorea (Nassula) · Colpodea (Colpoda) · Oligohymenophorea (Tetrahymena, Ichthyophthirius, Vorticella, Paramecium) · Plagiopylea (Plagiopyla) · Prostomatea (Coleps)OtherMyzozoa Plasmodiidae/Haemosporida (Plasmodium, Haemoproteus, Leucocytozoon)
Piroplasmida (Babesia, Theileria)Adele-Haemogregarina, Hepatozoon, KaryolysusEimeri-Cryptosporidiidae (Cryptosporidium)
Eimeriidae (Isospora, Cyclospora, Eimeria)
Sarcocystidae (Toxoplasma, Sarcocystis, Besnoitia, Neospora)Agamo-Rhytidocystidae (Rhytidocystis)GregariniaGregarinasina (Gregarina)ColpodellidaeChromeridaChromera velia, Vitrella brassicaformisWith a theca: Peridiniales (Pfiesteria, Peridinium) · Gonyaulacales (Ceratium, Gonyaulax) · Prorocentrales (Prorocentrum) · Dinophysiales (Dinophysis, Histioneis, Ornithocercus, Oxyphysis)
Without theca: Gymnodiniales (Gymnodinium, Karenia, Karlodinium, Amphidinium) · Suessiales (Polarella, Symbiodinium)
Noctilucales (Noctiluca)Syndiniales: Amoebophryaceae (Amoebophyra) · Duboscquellaceae (Duboscquella) · Syndiniaceae (Hematodinium, Syndinium)OtherRelatedCategories:
Wikimedia Foundation. 2010.
