- Vagus nerve
-
Nerve: Vagus nerve 
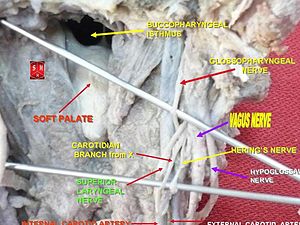
Plan of upper portions of glossopharyngeal, vagus, and accessory nerves. 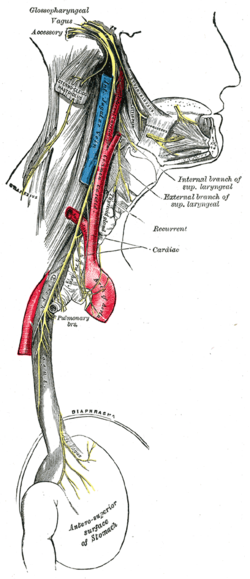
Course and distribution of the glossopharyngeal, vagus, and accessory nerves. Latin nervus vagus Gray's subject #205 910 Innervates Levator veli palatini, Salpingopharyngeus, Palatoglossus, Palatopharyngeus, Superior pharyngeal constrictor, Middle pharyngeal constrictor, Inferior pharyngeal constrictor, viscera MeSH Vagus+Nerve Cranial Nerves CN I – Olfactory CN II – Optic CN III – Oculomotor CN IV – Trochlear CN V – Trigeminal CN VI – Abducens CN VII – Facial CN VIII – Vestibulocochlear CN IX – Glossopharyngeal CN X – Vagus CN XI – Spinal Accessory CN XII – Hypoglossal The vagus nerve (
 /ˈveɪɡəs/ US dict: vā′·gəs), also called pneumogastric nerve or cranial nerve X, is the tenth of twelve (excluding CN0) paired cranial nerves. Upon leaving the medulla between the olivary nucleus and the inferior cerebellar peduncle, it extends through the jugular foramen, then passing into the carotid sheath between the internal carotid artery and the internal jugular vein down below the head, to the neck, chest and abdomen, where it contributes to the innervation of the viscera. Besides output to the various organs in the body, the vagus nerve conveys sensory information about the state of the body's organs to the central nervous system. 80-90% of the nerve fibers in the vagus nerve are afferent (sensory) nerves communicating the state of the viscera to the brain.[1]
/ˈveɪɡəs/ US dict: vā′·gəs), also called pneumogastric nerve or cranial nerve X, is the tenth of twelve (excluding CN0) paired cranial nerves. Upon leaving the medulla between the olivary nucleus and the inferior cerebellar peduncle, it extends through the jugular foramen, then passing into the carotid sheath between the internal carotid artery and the internal jugular vein down below the head, to the neck, chest and abdomen, where it contributes to the innervation of the viscera. Besides output to the various organs in the body, the vagus nerve conveys sensory information about the state of the body's organs to the central nervous system. 80-90% of the nerve fibers in the vagus nerve are afferent (sensory) nerves communicating the state of the viscera to the brain.[1]The medieval Latin word vagus means literally "Wandering" (the words vagrant, vagabond, and vague come from the same root). Sometimes the branches are spoken of in the plural and are thus called vagi (/ˈveɪdʒaɪ/, US dict: vā′·jī). The vagus is also called the pneumogastric nerve since it innervates both the lungs and the stomach.
The motor division of the vagus nerve is derived from the basal plate of the embryonic medulla oblongata, while the sensory division originates from the cranial neural crest.
The vagus nerve includes axons which emerge from or converge onto three nuclei of the medulla:
- The Dorsal nucleus of vagus nerve - which sends parasympathetic output to the viscera esp intestines
- The Nucleus ambiguus - which which sends parasympathetic output to the heart (slowing it down) and
- The Solitary nucleus - which receives afferent taste information and primary afferents from visceral organs
Contents
Branches
- Auricular nerve
- Pharyngeal nerve
- Superior laryngeal nerve
- Superior cervical cardiac branches of vagus nerve
- Inferior cervical cardiac branch
- Recurrent laryngeal nerve
- Thoracic cardiac branches
- Branches to the pulmonary plexus
- Branches to the esophageal plexus
- Anterior vagal trunk
- Posterior vagal trunk
- Hering-Breuer reflex in alveoli
The vagus runs posterior to the common carotid artery and internal jugular vein inside the carotid sheath.
Innervation
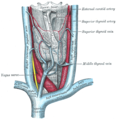
Right and left vagus nerves descend from the cranial vault through the jugular foramena, penetrating the carotid sheath between the internal and external carotid arteries, then passing posterolateral to the common carotid artery. The cell bodies of visceral afferent fibers of the vagus nerve are located bilaterally in the inferior ganglion of the vagus nerve (nodose ganglia).
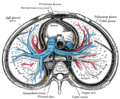
The right vagus nerve gives rise to the right recurrent laryngeal nerve, which hooks around the right subclavian artery and ascends into the neck between the trachea and esophagus. The right vagus then crosses anteriorly to the right subclavian artery and runs posterior to the superior vena cava and descends posterior to the right main bronchus and contributes to cardiac, pulmonary, and esophageal plexuses. It forms the posterior vagal trunk at the lower part of the esophagus and enters the diaphragm through the esophageal hiatus.
The left vagus nerve enters the thorax between left common carotid artery and left subclavian artery and descends on the aortic arch. It gives rise to the left recurrent laryngeal nerve, which hooks around the aortic arch to the left of the ligamentum arteriosum and ascends between the trachea and esophagus. The left vagus further gives off thoracic cardiac branches, breaks up into pulmonary plexus, continues into the esophageal plexus, and enters the abdomen as the anterior vagal trunk in the esophageal hiatus of the diaphragm.
The vagus nerve supplies motor parasympathetic fibers to all the organs except the suprarenal (adrenal) glands, from the neck down to the second segment of the transverse colon. The vagus also controls a few skeletal muscles, notable ones being:
- Cricothyroid muscle
- Levator veli palatini muscle
- Salpingopharyngeus muscle
- Palatoglossus muscle
- Palatopharyngeus muscle
- Superior, middle and inferior pharyngeal constrictors
- Muscles of the larynx (speech).
This means that the vagus nerve is responsible for such varied tasks as heart rate, gastrointestinal peristalsis, sweating, and quite a few muscle movements in the mouth, including speech (via the recurrent laryngeal nerve) and keeping the larynx open for breathing (via action of the posterior cricoarytenoid muscle, the only abductor of the vocal folds). It also has some afferent fibers that innervate the inner (canal) portion of the outer ear, via the Auricular branch (also known as Alderman's nerve) and part of the meninges. This explains why a person may cough when tickled on the ear (such as when trying to remove ear wax with a cotton swab).
The vagus nerve and the heart
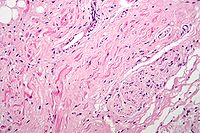 Fibres of the vagus nerve (right/bottom of image) innervate the sinoatrial node tissue (central and left of image). H&E stain.
Fibres of the vagus nerve (right/bottom of image) innervate the sinoatrial node tissue (central and left of image). H&E stain.
Parasympathetic innervation of the heart is controlled by the vagus nerve. To be specific, the vagus nerve acts to lower the heart rate. The right vagus innervates the sinoatrial node. Parasympathetic hyperstimulation predisposes those affected to bradyarrhythmias. The left vagus when hyperstimulated predisposes the heart to atrioventricular (AV) blocks.
At this location, neuroscientist Otto Loewi first proved that nerves secrete substances called neurotransmitters, which have effects on receptors in target tissues. In his experiment, Loewi electrically stimulated the vagus nerve of a frog heart, which slowed the heart. Then he took the fluid from the heart and transferred it to a second frog heart without a vagus nerve. The second heart slowed down without an electrical stimulation. Loewi described the substance released by the vagus nerve as vagusstoff, which was later found to be acetylcholine. Drugs that inhibit the muscarinic cholinergic receptor (anticholinergics) such as atropine and scopolamine are called vagolytic because they inhibit the action of the vagus nerve on the heart, gastrointestinal tract, and other organs. Anticholinergic drugs increase heart rate and are used to treat bradycardia (slow heart rate) and asystole, which is when the heart has no electrical activity.
Medical treatment involving the vagus nerve
Vagus nerve stimulation (VNS) therapy using a pacemaker-like device implanted in the chest is a treatment used since 1997 to control seizures in epilepsy patients and has recently been approved for treating drug-resistant cases of clinical depression.[2] A non-invasive VNS device that stimulates an afferent branch of the vagus nerve is also being developed and will soon undergo trials.[citation needed]
Clinical trials are currently underway in Antwerp, Belgium using VNS for the treatment of tonal tinnitus after a breakthrough study published in early 2011 by researchers at the University of Texas - Dallas showed successful tinnitus suppression in rats when tones were paired with brief pulses of stimulation of the vagus nerve. [3]
VNS may also be achieved by one of the vagal maneuvers: holding the breath for a few seconds, dipping the face in cold water, coughing, or tensing the stomach muscles as if to bear down to have a bowel movement.[3] Patients with supraventricular tachycardia,[3] atrial fibrillation, and other illnesses may be trained to perform vagal maneuvers (or find one or more on their own).
Vagus nerve blocking (VBLOC) therapy is similar to VNS but used only during the day. In a six-month open-label trial involving three medical centers in Australia, Mexico, and Norway, vagus nerve blocking has helped 31 obese participants lose an average of nearly 15 percent of their excess weight. A year-long 300-participant double-blind, phase II trial has begun.[4]
Vagotomy (cutting of the vagus nerve) is a now-obsolete therapy that was performed for peptic ulcer disease. Vagotomy is currently being researched as a less invasive alternative weight-loss procedure to gastric bypass surgery.[5] The procedure curbs the feeling of hunger and is sometimes performed in conjunction with putting bands on patients' stomachs, resulting in average weight loss of 43% at six months with diet and exercise.[6]
One serious side-effect of a Vagotomy is a Vitamin B-12 deficiency later in life - i.e., 10 years - that is similar to pernicious anemia. As one gets older, the stomach produces less acid. The acid, and one of its components called Intrinsic Factor, is needed to metabolize B-12 from food. The vagotomy reduces the acid that ultimately leads to the deficiency, which, if left untreated, causes nerve damage, tiredness, dementia, paranoia, and ultimately death.[7]
Physical and emotional effects
Activation of the vagus nerve typically leads to a reduction in heart rate, blood pressure, or both. This occurs commonly in the setting of gastrointestinal illness such as viral gastroenteritis or acute cholecystitis, or in response to other stimuli, including carotid sinus massage, Valsalva maneuver, or pain from any cause, in particular, having blood drawn. When the circulatory changes are great enough, vasovagal syncope results. Relative dehydration tends to amplify these responses.
Excessive activation of the vagal nerve during emotional stress, which is a parasympathetic overcompensation of a strong sympathetic nervous system response associated with stress, can also cause vasovagal syncope because of a sudden drop in blood pressure and heart rate. Vasovagal syncope affects young children and women more than other groups. It can also lead to temporary loss of bladder control under moments of extreme fear.
Research has shown that women having had complete spinal cord injury can experience orgasms through the vagus nerve, which can go from the uterus, cervix, and, it is presumed, the vagina to the brain.[8][9]
Liver - Insulin signaling activates the adenosine triphosphate (ATP)-sensitive potassium (KATP) channels in the Arcuate nucleus, decreases AgRP release, and through the vagus nerve, leads to decreased glucose production by the liver by decreasing gluconeogenic enzymes : Phosphoenolpyruvate carboxykinase, Glucose 6-phosphatase)[10][11]
Effects of vagus nerve lesions
The patient complains of hoarse voice, difficulty in swallowing (dysphagia), and choking when drinking fluid. There is also loss of gag reflex. Uvula deviates away from the side of lesion, and there is failure of palate elevation.
Additional images
See also
- Porphyria — This rare disorder can cause seizures and damage to the vagal nerve. Diagnosis, in some cases, may require DNA testing.
- Vagovagal reflex
- Vagus nerve stimulation
References
- ^ Functional and chemical anatomy of the afferent vagal system. Berthoud HR and Neuhuber WL
- ^ Nemeroff C, Mayberg H, Krahl S, McNamara J, Frazer A, Henry T, George M, Charney D, Brannan S (2006). "VNS therapy in treatment-resistant depression: clinical evidence and putative neurobiological mechanisms.". Neuropsychopharmacology 31 (7): 1345–55. doi:10.1038/sj.npp.1301082. PMID 16641939. link
- ^ a b Vibhuti N, Singh; Monika Gugneja (2005-08-22). "Supraventricular Tachycardia". eMedicineHealth.com. http://www.emedicinehealth.com/supraventricular_tachycardia/page7_em.htm. Retrieved 2008-11-28.
- ^ Mayo Clinic. Device Blocking Stomach Nerve Signals Shows Promise in Obesity
- ^ Ulcer surgery may help treat obesity - Diet and nutrition - MSNBC.com
- ^ . http://www.cnn.com/2007/HEALTH/conditions/07/09/obesity.nerve.ap/index.html.[dead link]
- ^ http://www.pernicious-anaemia-society.org
- ^ [1]
- ^ Komisaruk, B.R, Whipple, B., Crawford, A., Grimes, S., Liu, W-C., Kalin, A., & Mosier, K. (2004). Brain activation during vaginocervical self-stimulation and orgasm in women with complete spinal cord injury: MRI evidence of mediation by the Vagus nerves. [2]
- ^ Pocai, A; TK Lam, Gutierrez-Juarez R (2005). "Hypothalamic K(ATP) channels control hepatic glucose production". Nature 434: 1026–1031. doi:10.1038/nature03439.
- ^ Pagotto, U. (2009). "Where does insulin resistance start? The brain.". Diabetes Care 32 (2): S174-S177.
External links
- MedEd at Loyola grossanatomy/h_n/cn/cn1/cn10.htm
- Cranial Nerves at Yale 10-1
- Human anatomy at Dartmouth figures/chapter_24/24-7.HTM
- cranialnerves at The Anatomy Lesson by Wesley Norman (Georgetown University) (X)
Nerves of head and neck: the cranial nerves and nuclei (TA A14.2.01, GA 9.855) olfactory (AON->I) optic (LGN->II) oculomotor
(ON, EWN->III)trochlear (TN->IV) no significant branchestrigeminal
(PSN, TSN, MN, TMN->V)abducens (AN->VI) no significant branchesfacial (FMN, SN, SSN->VII) near originvestibulocochlear
(VN, CN->VIII)glossopharyngeal
(NA, ISN, SN->IX)before jugular fossaafter jugular fossavagus
(NA, DNVN, SN->X)before jugular fossaafter jugular fossaaccessory (NA, SAN->XI) hypoglossal (HN->XII) Categories:
Wikimedia Foundation. 2010.