- Supraventricular tachycardia
-
Supraventricular tachycardia Classification and external resources
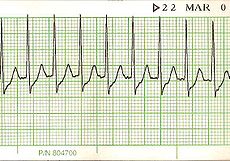
Lead II electrocardiogram strip showing SVT with a heart rate of about 150.ICD-10 I47.1 ICD-9 427.89, 427.0 MeSH D013617 Supraventricular tachycardia (SVT) is a general term that refers to any rapid heart rhythm originating above the ventricular tissue. Although technically an SVT can be due to any supraventricular cause, the term is often used by clinicians to refer to one specific cause of SVT, namely Paroxysmal supraventricular tachycardia (PSVT) which is due to AV nodal reentrant tachycardia. Supraventricular tachycardias can be contrasted to the potentially more dangerous ventricular tachycardias - rapid rhythms that originate within the ventricular tissue.
Contents
Signs and symptoms
Symptoms can come on suddenly and may go away without treatment. Stress, exercise, and emotion can all result in a normal or physiological increase in heart rate, but can also, though more rarely, precipitate SVT. Episodes can last a few minutes or as long as 1 or 2 days, sometimes persisting until treated. The rapid beating of the heart during SVT can make the heart a less-effective pump, decreasing cardiac output and blood pressure. The following symptoms are typical with a rapid pulse of 150–270 or more beats per minute:
- Pounding heart
- Shortness of breath
- Chest pain
- Rapid breathing
- Dizziness
- Loss of consciousness (in serious cases)
- Numbness of various body parts
Terminology
The term supraventricular tachycardia is often used differently in different settings.
- Theoretically, it refers to any tachycardia that is not ventricular in origin. This definition includes physiological sinus tachycardia which can be a normal reaction to stress and a variety of non-cardiac conditions such as fever and hyperthyroidism. In the widest useful sense supraventricular tachycardia includes abnormal sinus tachycardia, ectopic atrial tachycardia (that is, not from the sinoatrial node), atrial fibrillation/atrial flutter (though if identified these are usually considered separately) and junctional tachycardia.[1]
- Often, however, in a clinical setting, it is used practically as a synonym for paroxysmal supraventricular tachycardia (PSVT). This term refers to those SVTs that have a sudden, almost immediate onset [2] and are regular. A person experiencing PSVT may feel their heart rate go from 60 to 200 beats per minute instantaneously, often in response to a quick movement such as picking something up from the floor. Because physiological sinus tachycardias have a gradual (i.e. non-immediate) onset and AF is usually obviously irregular they are excluded from the PSVT category. PSVTs are most commonly AV nodal reentrant tachycardias or part of Wolff-Parkinson-White syndrome (WPW) - which may be "concealed", i.e. not evident on the resting electrocardiogram.
Types
The following are types of supraventricular tachycardias, each with a different mechanism of impulse maintenance. It should be noted that whilst all of the below terms are technically causes of SVT, clinicians usually use the specific term/diagnosis, when possible:
SVTs from a sinoatrial source:
- Inappropriate sinus tachycardia
- Sinoatrial node reentrant tachycardia (SANRT)
SVTs from an atrial source:
- Ectopic (unifocal) atrial tachycardia (EAT)
- Multifocal atrial tachycardia (MAT)
- Atrial fibrillation with a rapid ventricular response
- Atrial flutter with a rapid ventricular response
- Without rapid ventricular response, fibrillation and flutter are usually not classified as SVT
SVTs from an atrioventricular source (junctional tachycardia):
- AV nodal reentrant tachycardia (AVNRT) or junctional reciprocating tachycardia (JRT)
- Permanent (or persistent) junctional reciprocating tachycardia (PJRT), a form of JRT which occurs predominantly in infants and children but can occasionally occur in adults
- AV reentrant tachycardia (AVRT) - visible or concealed (including Wolff-Parkinson-White syndrome)
- Junctional ectopic tachycardia
Diagnosis
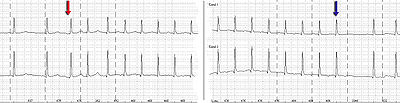 Holter monitor-Imaging with start (red arrow) and end (blue arrow) of a SV-tachycardia with a pulse frequency of about 128/min.
Holter monitor-Imaging with start (red arrow) and end (blue arrow) of a SV-tachycardia with a pulse frequency of about 128/min.
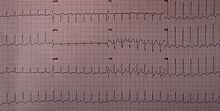
The individual subtypes of SVT can be usually be distinguished from each other by the physiological and electrical characteristics that are present in the patient's electrocardiogram (ECG).
Most supraventricular tachycardias have a narrow QRS complex on ECG, but supraventricular tachycardia with aberrant conduction (SVTAC) can produce a wide-complex tachycardia that may mimic ventricular tachycardia (VT). In the clinical setting, it is important to determine whether a wide-complex tachycardia is an SVT or a ventricular tachycardia, since they are treated differently. Ventricular tachycardia has to be treated appropriately, since it can quickly degenerate to ventricular fibrillation and death. A number of different algorithms have been devised to determine whether a wide-complex tachycardia is supraventricular or ventricular in origin.[3] In general, a history of structural heart disease dramatically increases the likelihood that the tachycardia is ventricular in origin.
- Sinus tachycardia is considered physiological or "appropriate" when a reasonable stimulus, such as the catecholamine surge associated with fright, stress, or physical activity, provokes the tachycardia. It is distinguished by a presentation identical to a normal sinus rhythm except for its fast rate (>100 beats per minute in adults).
- Sinoatrial node reentrant tachycardia (SANRT) is caused by a reentry circuit localised to the SA node, resulting in a normal morphology P-wave that falls before a regular, narrow QRS complex. It is therefore impossible to distinguish on the ECG from physiological sinus tachycardia unless the sudden onset is observed (or recorded on Holter monitor. It may sometimes be distinguished by its prompt response to vagal manoeuvres.
- Ectopic (unifocal) atrial tachycardia is tachycardia resultant from one ectopic focus within the atria, distinguished by a consistent P-wave of abnormal morphology that falls before a narrow, regular QRS complex.
- Multifocal atrial tachycardia (MAT) is tachycardia resultant from at least three ectopic foci within the atria, distinguished by P-waves of at least three different morphologies that all fall before irregular, narrow QRS complexes.
- Atrial fibrillation is not, in itself, a tachycardia, but when it is associated with a rapid ventricular response greater than 100 beats per minute, it becomes a tachycardia. A-fib is characteristically an "irregularly irregular rhythm" both in its atrial and ventricular depolarizations. It is distinguished by fibrillatory P-waves that, at some point in their chaos, stimulate a response from the ventricles in the form of irregular, narrow QRS complexes.
- Atrial flutter, is caused by a re-entry rhythm in the atria, with a regular rate of about 300 beats per minute. On the ECG, this appears as a line of "sawtooth" P-waves. The AV node will not usually conduct such a fast rate, and so the P:QRS usually involves a 2:1 or 4:1 block pattern, (though rarely 3:1, and sometimes 1:1 in the setting of class IC antiarrhythmic drug use). Because the ratio of P to QRS is usually consistent, A-flutter is often regular in comparison to its irregular counterpart, A-fib. Atrial Flutter is also not necessarily a tachycardia unless the AV node permits a ventricular response greater than 100 beats per minute.
- AV nodal reentrant tachycardia (AVNRT) is also sometimes referred to as junctional reciprocating tachycardia (JRT), since the atrioventricular junction (AV junction) includes the AV node. It involves a reentry circuit forming just next to or within the AV node itself. The circuit most often involves two tiny pathways one faster than the other, within the AV node. Because the AV node is immediately between the atria and the ventricle, the re-entry circuit often stimulates both, meaning that a retrogradely conducted P-wave is buried within or occurs just after the regular, narrow QRS complexes.
- Atrioventricular reentrant tachycardia (AVRT), also known as circus movement tachycardia (CMT), also results from a reentry circuit, although one physically much larger than AVNRT. One portion of the circuit is usually the AV node, and the other, an abnormal accessory pathway from the atria to the ventricle. Wolff-Parkinson-White syndrome is a relatively common abnormality with an accessory pathway, the Bundle of Kent crossing the AV valvular ring.
- In orthodromic AVRT, atrial impulses are conducted down through the AV node and retrogradely re-enter the atrium via the accessory pathway. A distinguishing characteristic of orthodromic AVRT can therefore be a P-wave that follows each of its regular, narrow QRS complexes, due to retrograde conduction.
- In antidromic AVRT, atrial impulses are conducted down through the accessory pathway and re-enter the atrium retrogradely via the AV node. Because the accessory pathway initiates conduction in the ventricles outside of the bundle of His, the QRS complex in antidromic AVRT is often wider than usual, with a delta wave.
- Finally, junctional ectopic tachycardia (JET) is a rare tachycardia caused by increased automaticity of the AV node itself initiating frequent heart beats. On the ECG, junctional tachycardia often presents with abnormal morphology P-waves that may fall anywhere in relation to a regular, narrow QRS complex. It is often due to drug toxicity.
Treatment
In general, SVT is rarely life threatening, but episodes can be treated or prevented. While some treatment modalities can be applied to all SVTs with impunity, there are specific therapies available to cure some of the different sub-types. Cure requires intimate knowledge of how and where the arrhythmia is initiated and propagated.
The SVTs can be separated into two groups, based on whether they involve the AV node for impulse maintenance or not. Those that involve the AV node can be terminated by slowing conduction through the AV node. Those that do not involve the AV node will not usually be stopped by AV nodal blocking maneuvers. These maneuvers are still useful however, as transient AV block will often unmask the underlying rhythm abnormality.
AV nodal blocking can be achieved in at least three different ways:
Physical maneuver
A number of physical maneuvers cause increased AV nodal block, principally through activation of the parasympathetic nervous system, conducted to the heart by the vagus nerve. These manipulations are therefore collectively referred to as vagal maneuvers.
The Valsalva maneuver should be the first vagal maneuver tried.[4] It works by increasing intra-thoracic pressure and affecting baro-receptors (pressure sensors) within the arch of the aorta. It is carried out by asking the patient to hold their breath and try to exhale forcibly as if straining during a bowel movement, or by getting them to hold their nose and blow out against it.[5]
There are many other vagal maneuvers including: holding ones breath for a few seconds, coughing, plunging the face into cold water,[5] (via the diving reflex[6]), drinking a glass of ice cold water, and standing on one's head. Carotid sinus massage, carried out by firmly pressing the bulb at the top of one of the carotid arteries in the neck, is effective but is often not recommended due to risks of stroke in those with plaque in the carotid arteries.
Medications
Adenosine, an ultra short acting AV nodal blocking agent, is indicated if vagal maneuvers are not effective.[7] If this works, followup therapy with diltiazem, verapamil or metoprolol may be indicated. SVT that does not involve the AV node may respond to other anti-arrhythmic drugs such as sotalol or amiodarone.
In pregnancy, adenosine is the treatment of choice as recommended by the ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias.[8]
Cardioversion
If the patient is unstable or other treatments have not been effective, cardioversion may be used, and is almost always effective.
Prevention
Once the acute episode has been terminated, ongoing treatment may be indicated to prevent a recurrence of the arrhythmia. Patients who have a single isolated episode, or infrequent and minimally symptomatic episodes usually do not warrant any treatment except observation.
Patients who have more frequent or disabling symptoms from their episodes generally warrant some form of preventive therapy. A variety of drugs including simple AV nodal blocking agents like beta-blockers and verapamil, as well as anti-arrhythmics may be used, usually with good effect, although the risks of these therapies need to be weighed against the potential benefits.
A limited study has demonstrated that acupuncture can also be effective in preventing paroxysmal supraventricular tachycardia[9].
Radiofrequency ablation has revolutionized the treatment of tachycardia caused by a re-entrant pathway. This is a low risk procedure that uses a catheter inside the heart to deliver radio frequency energy to locate and destroy the abnormal electrical pathways. Ablation has been shown to be highly effective: around 90% effective in eliminating AVNRT. Similar high rates of success are achieved with radio frequency ablation in eliminating AVRT and typical Atrial Flutter.
There is a newer treatment for SVT involving the AV node directly. This treatment is called Cryoablation. SVT involving the AV node is often a contraindication for using radiofrequency ablation due to the small (1%) incidence of injuring the AV node requiring a permanent pacemaker. With Cryoablation, a supercooled catheter is used (cooled by nitrous oxide gas), and the tissue is frozen to -10 °C. This provides the same result as radiofrequency ablation but does not carry the same risk. If you freeze the tissue and then realize you are in a dangerous spot, you can halt freezing the tissue and allow the tissue to spontaneously rewarm and the tissue is the same as if you never touched it. If after freezing the tissue to -10 °C, you get the desired result, then you freeze the tissue down to a temperature of -73 °C and you permanently ablate the tissue.
This therapy has further improved the treatment options for people with AVNRT (and other SVTs with pathways close to the AV node), widening the application of curative ablation to young patients with relatively mild but still troublesome symptoms who would not have accepted the risk of requiring a pacemaker.
Notable cases
After being successfully diagnosed and treated, Bobby Julich went on to place third in the 1998 Tour de France and win a Bronze Medal in the 2004 Summer Olympics.[10] Women's Olympic volleyball player Tayyiba Haneef-Park underwent an ablation for SVT just two months before competing in the 2008 Summer Olympics.[11] Tony Blair, former PM of the UK, was also operated on for atrial flutter. Anastacia was diagnosed with the disease.[12] Women's Olympic gold medalist swimmer, Rebecca Soni has had SVT and has had heart surgery for it. In addition, Neville Fields had corrective surgery for SVT in early 2006.
See also
- Tachycardia
- AV nodal reentrant tachycardia (AVNRT)
- Inappropriate sinus tachycardia
- Ashman phenomenonnn
- Junctional rhythm
- Wolff-Parkinson-White syndrome
References
- ^ "supraventricular tachycardia" at Dorland's Medical Dictionary
- ^ "paroxysmal supraventricular tachycardia" at Dorland's Medical Dictionary
- ^ Lau EW, Ng GA (2002). "Comparison of the performance of three diagnostic algorithms for regular broad complex tachycardia in practical application". Pacing and clinical electrophysiology : PACE 25 (5): 822–7. doi:10.1046/j.1460-9592.2002.00822.x. PMID 12049375.
- ^ "BestBets: Comparing Valsalva manoeuvre with carotid sinus massage in adults with supraventricular tachycardia". http://www.bestbets.org/bets/bet.php?id=930.
- ^ a b Vibhuti N, Singh; Monika Gugneja (2005-08-22). "Supraventricular Tachycardia". eMedicineHealth.com. http://www.emedicinehealth.com/supraventricular_tachycardia/page7_em.htm. Retrieved 2008-11-28.
- ^ Mathew PK (January 1981). "Diving reflex. Another method of treating paroxysmal supraventricular tachycardia". Arch. Intern. Med. 141 (1): 22–3. doi:10.1001/archinte.141.1.22. PMID 7447580.
- ^ "Adenosine vs Verapamil in the acute treatment of supraventricular tachycardias". http://www.bestbets.org/bets/bet.php?id=996.
- ^ Blomström-Lundqvist ET AL., MANAGEMENT OF PATIENTS WITH Supraventricular Arrhythmias. J Am Coll Cardiol 2003;42:1493–531 [1]
- ^ Wu RD, Lin LF. Clinical observation on wrist-ankle acupuncture for treatment of paroxysmal supraventricular tachycardia (PSVT). Zhongguo Zhen Jiu. 2006 Dec;26(12):854-6. [2]
- ^ An athlete's experience with Re-entrant Supraventricular Tachycardia
- ^ USA Volleyball 2008 Olympic Games Press Kit
- ^ "Anastacia delays heart surgery". News of the World. 3 Nov 2008. http://www.nowmagazine.co.uk/celebrity-news/279923/anastacia-delays-heart-surgery/1/. Retrieved 30 Apr 2010.
External links
- Supraventricular Tachycardia information from Seattle Children's Hospital Heart Center
Categories:
Wikimedia Foundation. 2010.