- Ciliary muscle
-
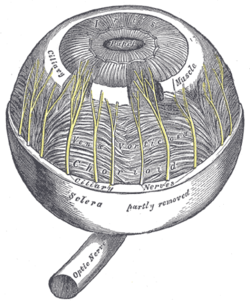
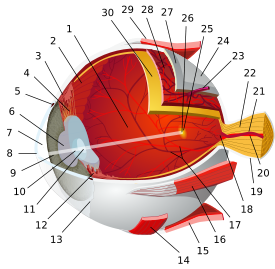
Ciliary muscle The choroid and iris. (Ciliary muscle is labeled near top.) Latin musculus ciliaris Gray's subject #225 1011 Origin 1) longitudinal fibers → scleral spur; 2) circular fibers → encircle root of iris[1] Insertion 1) longitudinal fibers → ciliary process, 2) circular fibers → encircle root of iris[1] Artery long posterior ciliary arteries Nerve short ciliary Actions 1) accommodation, 2) regulation of trabecular meshwork pore size The ciliary muscle (
 /ˈsɪli.ɛəri/) is a ring of striated smooth muscle[2] in the eye's middle layer (vascular layer) that controls accommodation for viewing objects at varying distances and regulates the flow of aqueous humour into Schlemm's canal. The muscle has parasympathetic and sympathetic innervation.
/ˈsɪli.ɛəri/) is a ring of striated smooth muscle[2] in the eye's middle layer (vascular layer) that controls accommodation for viewing objects at varying distances and regulates the flow of aqueous humour into Schlemm's canal. The muscle has parasympathetic and sympathetic innervation.Contents
Etymology
The word ciliary had its origins around 1685–1695.[3] The term cilia originated a few years later in 1705–1715, and is the Neo-Latin plural of cilium meaning eyelash. In Latin, cilia means upper eyelid and is perhaps a back formation from supercilium, meaning eyebrow. The suffix -ary originally occurred in loanwords from Middle English (-arie), Old French (-er, -eer, -ier, -aire, -er), and Latin (-ārius); it can generally mean "pertaining to, connected with," "contributing to," and "for the purpose of."[4] Taken together, cili(a)-ary pertains to various anatomical structures in and around the eye, namely the ciliary body and annular suspension of the lens of the eye.[5]
Embryologic development
Forms from the mesoderm within the choroid[6] and considered a cranial neural crest derivative.
Mode of action
Accommodation
Main article: accommodation of the eyeThe ciliary fibers have circular (Ivanoff),[7] longitudinal (meridional) and radial orientations.[8]
According to Hermann von Helmholtz's theory, the circular ciliary muscle fibers affect zonular fibers in the eye (fibers that suspend the lens in position during accommodation), enabling changes in lens shape for light focusing. When the ciliary muscle contracts, it pulls itself forward and moves the frontal region toward the axis of the eye. This releases the tension on the lens caused by the zonular fibers (fibers that hold or flatten the lens). This release of tension of the zonular fibers causes the lens to become more spherical, adapting to short range focus. The other way around, relaxation of the ciliary muscle causes the zonular fibers to become taut, flattening the lens, increasing the focal distance,[9] increasing long range focus. Although Helmholtz's theory has been widely accepted since 1855, its mechanism still remains controversial. Alternative theories of accommodation have been proposed by others, including L. Johnson, M. Tscherning, and Ronald A. Schachar.[2]
Trabecular meshwork pore size
Contraction and relaxation of the longitudinal fibers, which insert into the trabecular meshwork in the anterior chamber of the eye, cause an increase and decrease in the meshwork pore size, respectively, facilitating and impeding aqueous humour flow into the canal of Schlemm.[10]
Innervation
The ciliary muscle receives both parasympathetic and sympathetic fibers from the ciliary ganglion called short ciliary nerves. These postganglionic fibers are part of cranial nerve III (Oculomotor nerve).[11]
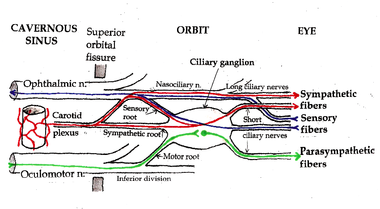 Ciliary ganglion with sympathetic and parasympathetic fibers of ciliary nerves.
Ciliary ganglion with sympathetic and parasympathetic fibers of ciliary nerves.
Postsynaptic sympathetic signals that originate in the superior cervical ganglion are carried by the nasociliary nerve or directly extend from the internal carotid plexus and pass through the ciliary ganglion. Sympathetic (adrenergic) activation of the muscle's beta-2 receptors result in relaxation and increase in ciliary body size.
Presynaptic parasympathetic signals that originate in the Edinger-Westphal nucleus are carried by cranial nerve III (the oculomotor nerve) and synapse on the ciliary ganglion. Parasympathetic activation of the M3 muscarinic receptors causes ciliary muscle contraction and consequent reduction in the size of the ciliary body.
The adrenergic tone is dominant over the parasympathetic tone.[9]
Role in the treatment of glaucoma
Open-angle glaucoma (OAG) and closed-angle glaucoma (CAG) may be treated by muscarinic receptor agonists (e.g., pilocarpine), which cause rapid miosis and contraction of the ciliary muscles, opening the trabecular meshwork, facilitating drainage of the aqueous humour into the canal of Schlemm and ultimately decreasing intraocular pressure.[12]
Additional images
See also
References
- ^ a b Gest, Thomas R; Burkel, William E. "Anatomy Tables - Eye." Medical Gross Anatomy. 2000. University of Michigan Medical School. January 5, 2010 Umich.edu
- ^ a b Kleinmann, Guy MD; Kim, Hee Joon MD; Yee, Richard W. MD (2006). "Scleral Expansion Procedure for the Correction of Presbyopia." (article) International Ophthalmology Clinics. 46(3):1-12. Lippincott Williams & Wilkins, Inc.. ISSN: 0020-8167.
- ^ "cilia", Unabridged. Source location: Random House, Inc. Reference.com, Accessed: January 16, 2010
- ^ Dictionary.com, "-ary," in The American Heritage Dictionary of the English Language, Fourth Edition. Source location: Houghton Mifflin Company, 2004. Reference.com, Accessed: January 16, 2010.
- ^ "ciliary," in Dictionary.com Unabridged. Source location: Random House, Inc. Reference.com, Accessed: January 16, 2010.
- ^ Dudek RW, Fix JD (2004). "Eye" (chapter 9). Embryology - Board Review Series (3rd edition, illustrated). Lippincott Williams & Wilkins. p. 92. ISBN 0781757266, 9780781757263. Books.Google.com, Retrieved January 17, 2010.
- ^ Sampaolesi R, Sampaolesi JR, Zárate G (2009). "Ocular Embryology with Special Reference to Chamber Angle Development" (chapter 8). The Glaucomas - Pediatric Glaucomas (volume 1). Springer Berlin Heidelberg. pp. 61–69. ISBN 978-3-540-69146-4. Springerlink.com
- ^ Riordan-Eva Paul, "Chapter 1. Anatomy & Embryology of the Eye" (Chapter). Riordan-Eva P, Whitcher JP (2008). Vaughan & Asbury's General Ophthalmology (17th ed.). McGraw-Hill. AccessMedicine.com
- ^ a b Hardman JG, Limbird LE, Gilman AG (2006). "Table 6-1". Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th Edition ed.). New York: McGraw-Hill. pp. 143–145. ISBN 0-07-142280-3.
- ^ Salmon John F, "Chapter 11. Glaucoma" (Chapter). Riordan-Eva P, Whitcher JP (2008). Vaughan & Asbury's General Ophthalmology (17th ed.). McGraw-Hill. AccessMedicine.com
- ^ Moore KL, Dalley AF (2006). "Head (chapter 7)". Clinically Oriented Anatomy (5th ed.). Lippincott Williams & Wilkins. p. 972. ISBN 0-7817-3639-0.
- ^ Le, Tao T.; Cai, Xumei; Waples-Trefil, Flora. "QID: 22067". USMLERx. MedIQ Learning, LLC. 2006–2010. 13 January 2010 Usmlerx.com
External links
Sensory system – visual system – globe of eye (TA A15.2.1–6, TH 3.11.08.0-5, GA 10.1005) Fibrous tunic (outer) Episcleral layer • Schlemm's canal • Trabecular meshworkUvea/vascular tunic (middle) Ciliary processes • Ciliary muscleRetina (inner) LayersCellsPhotoreceptor cells (Cone cell, Rod cell) → (Horizontal cell) → Bipolar cell → (Amacrine cell) → Retina ganglion cell (Midget cell, Parasol cell, Bistratified cell, Giant retina ganglion cells, Photosensitive ganglion cell) → Diencephalon: P cell, M cell, K cell
Muller gliaOtherAnterior segment Posterior segment Other M: EYE
anat(g/a/p)/phys/devp/prot
noco/cong/tumr, epon
proc, drug(S1A/1E/1F/1L)
Sensory system: Visual system and eye movement pathways Visual perception 1° (Bipolar cell of Retina) → 2° (Ganglionic cell) → 3° (Optic nerve → Optic chiasm → Optic tract → LGN of Thalamus) → 4° (Optic radiation → Cuneus and Lingual gyrus of Visual cortex → Blobs → Globs)Muscles of orbit TrackingHorizontal gazeVertical gazePupillary reflex Pupillary dilation1° (Posterior hypothalamus → Ciliospinal center) → 2° (Superior cervical ganglion) → 3° (Sympathetic root of ciliary ganglion → Nasociliary nerve → Long ciliary nerves → Iris dilator muscle)1° (Retina → Optic nerve → Optic chiasm → Optic tract → Visual cortex → Brodmann area 19 → Pretectal area) → 2° (Edinger-Westphal nucleus) → 3° (Short ciliary nerves → Ciliary ganglion → Ciliary muscle)Circadian rhythm M: EYE
anat(g/a/p)/phys/devp/prot
noco/cong/tumr, epon
proc, drug(S1A/1E/1F/1L)
Categories:- Muscles of the head and neck
- Eye anatomy
Wikimedia Foundation. 2010.