- Cyclooxygenase
-
"COX" redirects here. For other meanings, see Cox (disambiguation).
prostaglandin-endoperoxide synthase Identifiers EC number 1.14.99.1 CAS number 9055-65-6 Databases IntEnz IntEnz view BRENDA BRENDA entry ExPASy NiceZyme view KEGG KEGG entry MetaCyc metabolic pathway PRIAM profile PDB structures RCSB PDB PDBe PDBsum Gene Ontology AmiGO / EGO Search PMC articles PubMed articles cyclooxygenase 1 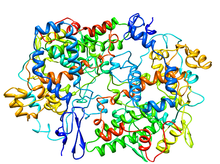
Crystallographic structure of prostaglandin H2 synthase-1 complex with flurbiprofen.[1] Identifiers Symbol PTGS1 Alt. symbols COX-1 Entrez 5742 HUGO 9604 OMIM 176805 PDB 1CQE RefSeq NM_080591 UniProt P23219 Other data EC number 1.14.99.1 Locus Chr. 9 q32-q33.3 cyclooxygenase 2 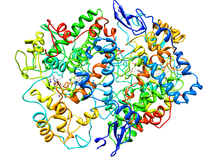
Cyclooxygenase-2 (Prostaglandin Synthase-2) in complex with a COX-2 selective inhibitor.[2] Identifiers Symbol PTGS2 Alt. symbols COX-2 Entrez 5743 HUGO 9605 OMIM 600262 PDB 6COX RefSeq NM_000963 UniProt P35354 Other data EC number 1.14.99.1 Locus Chr. 1 q25.2-25.3 Cyclooxygenase (COX) is an enzyme (EC 1.14.99.1) that is responsible for formation of important biological mediators called prostanoids, including prostaglandins, prostacyclin and thromboxane. Pharmacological inhibition of COX can provide relief from the symptoms of inflammation and pain. Non-steroidal anti-inflammatory drugs, such as aspirin and ibuprofen, exert their effects through inhibition of COX. The names "prostaglandin synthase (PHS)" and "prostaglandin endoperoxide synthetase (PES)" are still used to refer to COX.
Contents
Function
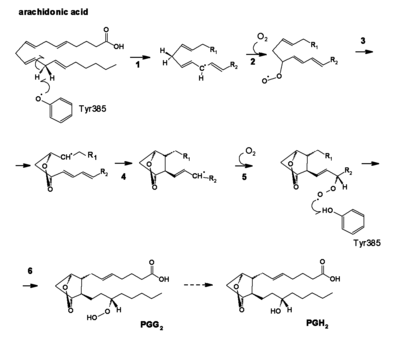
See also: Prostaglandin and EicosanoidCOX converts arachidonic acid (AA, an ω-6 PUFA) to prostaglandin H2 (PGH2), the precursor of the series-2 prostanoids. The enzyme contains two active sites: a heme with peroxidase activity, responsible for the reduction of PGG2 to PGH2, and a cyclooxygenase site, where arachidonic acid is converted into the hydroperoxy endoperoxide prostaglandin G2 (PGG2). The reaction proceeds through H atom abstraction from arachidonic acid by a tyrosine radical generated by the peroxidase active site. Two O2 molecules then react with the arachidonic acid radical, yielding PGG2.
At present, three COX isoenzymes are known: COX-1, COX-2, and COX-3. COX-3 is a splice variant of COX-1, which retains intron one and has a frameshift mutation; thus some prefer the name COX-1b or COX-1 variant (COX-1v).[3]
Different tissues express varying levels of COX-1 and COX-2. Although both enzymes act basically in the same fashion, selective inhibition can make a difference in terms of side-effects. COX-1 is considered a constitutive enzyme, being found in most mammalian cells. COX-2, on the other hand, is undetectable in most normal tissues. It is an inducible enzyme, becoming abundant in activated macrophages and other cells at sites of inflammation. More recently, it has been shown to be upregulated in various carcinomas and to have a central role in tumorigenesis.
Both COX-1 and -2 (also known as PGHS-1 and -2) also oxygenate two other essential fatty acids – DGLA (ω-6) and EPA (ω-3) – to give the series-1 and series-3 prostanoids, which are less inflammatory than those of series-2. DGLA and EPA are competitive inhibitors with AA for the COX pathways. This inhibition is a major mode of action in the way that dietary sources of DGLA and EPA (e.g., borage, fish oil) reduce inflammation.[4]
Pharmacology
In terms of their molecular biology, COX-1 and COX-2 are of similar molecular weight, approximately 70 and 72 kDa, respectively, and having 65% amino acid sequence homology and near-identical catalytic sites. The most significant difference between the isoenzymes, which allows for selective inhibition, is the substitution of isoleucine at position 523 in COX-1 with valine in COX-2. The smaller Val523 residue in COX-2 allows access to a hydrophobic side-pocket in the enzyme (which Ile523 sterically hinders). Drug molecules, such as DuP-697 and the coxibs derived from it, bind to this alternative site and are considered to be selective inhibitors of COX-2.
Classical NSAIDs
See also: Mechanism of action of aspirinThe main COX inhibitors are the non-steroidal anti-inflammatory drugs (NSAIDs).
The classical COX inhibitors are not selective and inhibit all types of COX. The resulting inhibition of prostaglandin and thromboxane synthesis has the effect of reduced inflammation, as well as antipyretic, antithrombotic and analgesic effects. The most frequent adverse effect of NSAIDs is irritation of the gastric mucosa as prostaglandins normally have a protective role in the gastrointestinal tract. Some NSAIDs are also acidic which may cause additional damage to the gastrointestinal tract.
Newer NSAIDs
Selectivity for COX-2 is the main feature of celecoxib, rofecoxib, and other members of this drug class. Because COX-2 is usually specific to inflamed tissue, there is much less gastric irritation associated with COX-2 inhibitors, with a decreased risk of peptic ulceration. The selectivity of COX-2 does not seem to negate other side-effects of NSAIDs, most notably an increased risk of renal failure, and there is evidence that indicates an increase in the risk for heart attack, thrombosis, and stroke through an increase of thromboxane unbalanced by prostacyclin (which is reduced by COX-2 inhibition). Rofecoxib (brand name Vioxx) was withdrawn in 2004 because of such concerns. Some other COX-2 selective NSAIDs, such as celecoxib, and etoricoxib, are still on the market.
Natural COX inhibition
Culinary mushrooms, like Maitake, may be able to partially inhibit COX-1 and COX-2.[5][6]
A variety of flavonoids have been found to inhibit COX-2.[7]
Cardiovascular side-effects of COX inhibitors
COX-2 inhibitors have been found to increase the risk of atherothrombosis even with short-term use. A 2006 analysis of 138 randomised trials and almost 150 000 participants[8] showed that selective COX-2 inhibitors are associated with a moderately increased risk of vascular events, mainly due to a twofold increased risk of myocardial infarction, and also that high-dose regimens of some traditional NSAIDs such as diclofenac and ibuprofen are associated with a similar increase in risk of vascular events.
See also
- COX-2 selective inhibitor
- PTGS2
- Cyclooxygenase 2 inhibitors: drug discovery and development
References
- ^ PDB 1CQE; Picot D, Loll PJ, Garavito RM (January 1994). "The X-ray crystal structure of the membrane protein prostaglandin H2 synthase-1". Nature 367 (6460): 243–9. doi:10.1038/367243a0. PMID 8121489.
- ^ PDB 6COX; Kurumbail RG, Stevens AM, Gierse JK, McDonald JJ, Stegeman RA, Pak JY, Gildehaus D, Miyashiro JM, Penning TD, Seibert K, Isakson PC, Stallings WC (1996). "Structural basis for selective inhibition of cyclooxygenase-2 by anti-inflammatory agents". Nature 384 (6610): 644–8. doi:10.1038/384644a0. PMID 8967954.
- ^ Chandrasekharan NV, Dai H, Roos KL, Evanson NK, Tomsik J, Elton TS, Simmons DL (October 2002). "COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression". Proc. Natl. Acad. Sci. U.S.A. 99 (21): 13926–31. doi:10.1073/pnas.162468699. PMC 129799. PMID 12242329. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=129799.
- ^ Simopoulos AP (December 2002). "Omega-3 fatty acids in inflammation and autoimmune diseases". J Am Coll Nutr 21 (6): 495–505. PMID 12480795.
- ^ Zhang Y, Mills GL, Nair MG (December 2002). "Cyclooxygenase inhibitory and antioxidant compounds from the mycelia of the edible mushroom Grifola frondosa". J. Agric. Food Chem. 50 (26): 7581–5. doi:10.1021/jf0257648. PMID 12475274.
- ^ Zhang Y, Mills GL, Nair MG (2003). "Cyclooxygenase inhibitory and antioxidant compounds from the fruiting body of an edible mushroom, Agrocybe aegerita". Phytomedicine 10 (5): 386–90. doi:10.1078/0944-7113-00272. PMID 12834003.
- ^ O'Leary KA, de Pascual-Tereasa S, Needs PW, Bao YP, O'Brien NM, Williamson G (July 2004). "Effect of flavonoids and vitamin E on cyclooxygenase-2 (COX-2) transcription". Mutat. Res. 551 (1-2): 245–54. doi:10.1016/j.mrfmmm.2004.01.015. PMID 15225597.
- ^ Kearney PM, Baigent C, Godwin J, Halls H, Emberson JR, Patrono C (June 2006). "Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials". BMJ 332 (7553): 1302–8. doi:10.1136/bmj.332.7553.1302. PMC 1473048. PMID 16740558. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1473048.
Further reading
- Pedro J. Silva, Pedro A. Fernandes and Maria J. Ramos (2003) A theoretical study of radical-only and combined radical/carbocationic mechanisms of arachidonic acid cyclooxygenation by prostaglandin H synthase. Theoretical Chemistry Accounts, 110, 345-351.
External links
Oxidoreductases: dioxygenases, including steroid hydroxylases (EC 1.14) 1.14.11: 2-oxoglutarate 1.14.13: NADH or NADPH Flavin-containing monooxygenase (FMO1, FMO2, FMO3, FMO4, FMO5) - Nitric oxide synthase (NOS1, NOS2, NOS3) - Cholesterol 7 alpha-hydroxylase - Methane monooxygenase - 3A4 - Lanosterol 14 alpha-demethylase1.14.14: reduced flavin or flavoprotein 1.14.15: reduced iron-sulfur protein 1.14.16: reduced pteridine (BH4 dependent) 1.14.17: reduced ascorbate 1.14.18-19: other 1.14.99 - miscellaneous Precursor Prostanoids Leukotrienes 5-Lipoxygenase activating protein/Arachidonate 5-lipoxygenase
LTC4 synthase · Gamma-glutamyl transpeptidase · DPEP2Ungrouped Categories:- Genes on chromosome 9
- Genes on chromosome 1
- EC 1.14.99
- Integral membrane proteins
Wikimedia Foundation. 2010.