- Radiosurgery
-
This article is about the medical procedure. For the album by American rock band New Found Glory, see Radiosurgery (album).
Radiosurgery Intervention 
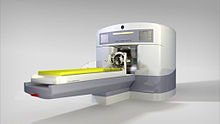
CLINAC: a model of steerable linear accelerator commonly used in radiosurgeryICD-9-CM 92.3 MeSH D016634 Radiosurgery is a medical procedure that allows non-invasive treatment of benign and malignant tumors. It is also known as stereotactic radiotherapy, (SRT) when used to target lesions in the brain, and stereotactic body radiotherapy (SBRT) when used to target lesions in the body. In addition to cancer, it has also been shown to be beneficial for the treatment of some non-cancerous conditions, including functional disorders such as arteriovenous malformations (AVMs) and trigeminal neuralgia.
Radiosurgery operates by directing highly focused beams of ionizing radiation with high precision. It is a relatively recent technique (1951), which is used to ablate, by means of a precise dosage of radiation, intracranial and extracranial tumors and other lesions that could be otherwise inaccessible or inadequate for open surgery. There are many nervous diseases for which conventional surgical treatment is difficult or inadvisable due to deleterious consequences for the patient, such as damage to nearby arteries, nerves, and other vital structures.
Contents
Medical uses
Radiosurgery has been especially helpful for the localized, highly precise treatment of brain tumors. Due to the steep fall off of the irradiation fields (isodoses) from the center of the target to be ablated, normal structures such as the brain, and other vascular and neural structures around it, are relatively spared. This is achieved through the high mechanical precision of the radiation source, and the assured reproducibility of the target. The precision in the positioning of the patient, in the calculation of dosages, and in the safety of the patient, are all extremely high.
Radiosurgery is indicated primarily for the therapy of tumors, vascular lesions and functional disorders. Significant clinical judgment must be used with this technique and considerations must include lesion type, pathology if available, size, location and age and general health of the patient. General contraindications to radiosurgery include excessively large size of the target lesion or lesions too numerous for practical treatment.
The non-interference with the quality of life of the patient in the post-operatory period competes with the inconvenience of the latency of months until the result of the radiosurgery is accomplished.
Outcome may not be evident for months after the treatment. Since radiosurgery does not remove the tumor, but results in a biological inactivation of the tumor, lack of growth of the lesion is normally considered to be treatment success. General indications for Radiosurgery include many kinds of brain tumors, such as acoustic neuromas, germinomas, meningiomas, metastases , trigeminal neuralgia, arteriovenous malformations and skull base tumors among others. Expansion of stereotactic radiotherapy to extracranial lesions is increasing, and includes metastases, liver cancer, lung cancer, pancreatic cancer, etc. It has been demonstrated by the thousands of successfully treated cases, that radiosurgery can be a very safe and efficient method for the management of many difficult brain lesions, while it avoids the loss in quality of life associated to other more invasive methods.
Gamma knife
The Gamma Knife (also known as the Leksell Gamma Knife) is a creation of Elekta AB, a Swedish public company, used to treat brain tumors by administering high-intensity radiation therapy in a manner that concentrates the radiation over a small volume. The device was invented at the Karolinska Institute in Stockholm, Sweden, in 1967 by Lars Leksell, a neurosurgeon, and Börje Larsson, a radiobiologist from Sweden's Uppsala University.
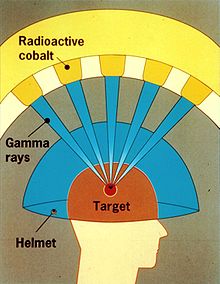
A Gamma Knife typically contains 201 cobalt-60 sources of approximately 30 curies (1.1 TBq), each placed in a circular array in a heavily shielded assembly. The device aims gamma radiation through a target point in the patient's brain. The patient wears a specialized helmet that is surgically fixed to the skull, so that the brain tumor remains stationary at the target point of the gamma rays. An ablative dose of radiation is thereby sent through the tumor in one treatment session, while surrounding brain tissues are relatively spared.
Radiosurgery uses high doses of radiation to kill cancer cells and shrink tumors, delivered precisely to avoid damaging healthy brain tissue. Gamma Knife radiosurgery is able to accurately focus many beams of high-intensity gamma radiation to converge on one or more tumors. Each individual beam is of relatively low intensity, so the radiation has little effect on intervening brain tissue and is concentrated only at the tumor itself.
Gamma Knife radiosurgery has proven effective for patients with benign or malignant brain tumors up to 4 centimeters in size, vascular malformations such as an arteriovenous malformation (AVM), pain or other functional problems.[1][2][3][4] For treatment of trigeminal neuralgia, the procedure may be used repeatedly on patients.
The risks of gamma knife radiosurgery treatment are very low[5], and complications are related to the condition being treated.[6][7]
Risks
According to the New York Times, radiation overdoses have occurred with the linear accelerator method of radiosurgery, in large part due to inadequate safeguards in equipment retrofitted for stereotactic radiosurgery.[8] The U.S. Food and Drug Administration (FDA) regulates these devices, whereas the Gamma Knife is regulated by the Nuclear Regulatory Commission. The NYT article focuses on Varian equipment and associated software, but the problem is not likely limited to that manufacturer.
Definition and applications
Radiation oncologists make use of highly sophisticated, highly precise and complex instruments, such as stereotactic devices, linear accelerators, the gamma knife, computers and laser beams. The highly precise irradiation of targets within the brain is planned by the radiation oncologist based on images, such as computed tomography (CT), magnetic resonance imaging (MRI), and angiography of the brain and body. The radiation is applied from an external source, under precise mechanical orientation by a specialized apparatus. Multiple beams are directed (collimated) and centered at the intracranial or extracranial lesion to be treated. In this way, healthy tissues around the target are relatively spared.
Patients can be treated within one to five days and as an outpatient. By comparison, the average hospital stay for a craniotomy (conventional neurosurgery, requiring the opening of the skull) is about 15 days. Radiosurgery costs less than conventional surgery, and with much less morbidity, e.g. mortality, pain and post-surgical complications, such as hemorrhage and infection. The period of recovery is minimal, and in the day following the treatment the patient may return to his or her normal life style, without any discomfort. However, radiosurgery is not without limitations and disadvantges. It is difficult and dangerous to treat masses larger than 3 cm because it will require very high doses of radiation. Fractionated radiotherapy may be a better option ideally combined with surgical debulking. The duration of time required to achieve the desired effects is much longer than surgery; it can take up to two years for arteriovenous malformations. During that time, the patient remains at risk for a rebleed. For treatment of tumors, it is important to remember that radiosurgery does not physically remove the tumor, rather stops it from growing larger. Therefore, it is not a good option when the tumor presents with significant mass effect on vital structures of the brain or spinal cord and when it causes increased intracranial apressure. Open surgery is needed to relieve pressure, remove the tumor totally or debulk (reduce it in size) it to make it a better target for radiotherapy or radiosurgery. Open surgery and radiosurgery are often used in conjunction for many types of brain tumors. Radiosurgery is a particularly good option for patients who are poor surgical risks due to their medical co-morbidities.
Mechanism of action
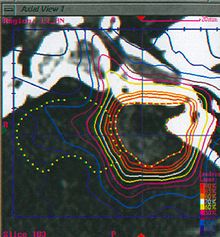 Planning CT scan with IV contrast in a patient with left cerebellopontine angle vestibular schwannoma
Planning CT scan with IV contrast in a patient with left cerebellopontine angle vestibular schwannoma
The fundamental principle of radiosurgery is that of selective ionization of tissue, by means of high-energy beams of radiation. Ionization is the production of ions and free radicals which are usually deleterious to the cells. These ions and radicals, which may be formed from the water in the cell or from the biological materials can produce irreparable damage to DNA, proteins, and lipids, resulting in the cell's death. Thus, biological inactivation is carried out in a volume of tissue to be treated, with a precise destructive effect. The radiation dose is usually measured in grays, where one gray (Gy) is the absorption of one joule per kilogram of mass. A unit that attempts to take into account both the different organs that are irradiated and the type of radiation is the sievert, a unit that describes both the amount of energy deposited and the biological effectiveness.
In order to perform optimal radiosurgery, the radiation oncologist chooses the best type of radiation to be used and how it will be delivered. In order to plan the radiation incidence and dosage, the physicists calculate a map portraying the lines of equal absorbed dose of radiation upon the patient's head (this is called an isodose map). Information about the tumor's location is obtained from a series of computerized tomograms, which are then fed to special planning computer software.
Stereotactic radiosurgery generally utilizes gamma rays or x-rays. There is also increasing interest in using particle therapy such as protons and carbon ions for radiosurgery, though this is not widely available.
The emission head (called "gantry") is mechanically rotated around the patient, in a full or partial circle. The table where the patient is lying, the 'couch', can also be moved in small linear or angular steps. The combination of the movements of the gantry and of the couch makes possible the computerized planning of the volume of tissue that is going to be irradiated. Devices with an energy of 6 MeV are the most suitable for the treatment of the brain, due to the depth of the target. In addition, the diameter of the energy beam leaving the emission head can be adjusted to the size of the lesion by means of interchangeable collimators (an orifice with different diameters, varying from 5 to 40 mm, in steps of 5 mm). There are also multileaf collimators, which consist of a number of metal leaflets that can be moved dynamically during treatment in order to shape the radiation beam to conform to the mass to be ablated. Latest generation Linacs are capable of achieving extremely narrow beam geometries, such as 0.15 to 0.3 mm. Therefore, they can be used for several kinds of surgeries which hitherto have been carried out by open or endoscopic surgery, such as for trigeminal neuralgia, etc. The exact mechanism of its effectiveness for trigemial neuralgia is not known; however, its use for this purpose has become very common. Long term followup data has shown it to be as effective as radiofrequency ablation but inferior to surgery as far as recurrence rate for pain is concerned.
Protons, may also be used in radiosurgery Proton Beam Therapy (PBT). Protons are produced by a medical synchrotron or cyclotron, extracting them from proton donor materials and accelerating them in successive travels through a circular, evacuated conduit or cavity, using powerful magnets, until they reach sufficient energy (usually about 200 MeV) to enable them to approximately traverse a human body, then stop. They are then released toward the irradiation target which is region in the patient's body. In some machines, which deliver only a certain energy of protons, a custom mask made of plastic will be interposed between the initial beam and the patient, in order to adjust the beam energy for a proper amount of penetration. Because of the Bragg Peak effect, proton therapy has advantages over other the other forms of radiation, since most of the proton's energy is deposited within a limited distance, so tissue beyond this range (and to some extent also tissue inside this range) is spared from the effects of radiation. This property of protons, which has been called the "depth charge effect" allows for conformal dose distributions to be created around even very irregularly shaped targets, and for higher doses to targets surrounded or backstopped by radiation-sensitive structures such as the optic chiasm or brainstem. In recent years, however, "intensity modulated" techniques have allowed for similar conformities to be attained using linear accelerator radiosurgery.
The selection of the proper kind of radiation and device depends on many factors including lesion type, size and location in relation to critical structures. Data suggests that similar clinical outcomes are possible with all of these methods. More important than the device used are issues regarding indications for treatment, total dose delivered, fractionation schedule and conformity of the treatment plan.
History
Radiosurgery was first developed at the Karolinska Institute of Stockholm, Sweden in 1949. It was jointly developed by Dr. Lars Leksell, a neurosurgeon and Bjorn Larsson, a radiobiologist from Uppsala University. Leksell initially used protons from a cyclotron to irradiate brain tumor lesions.
In 1968, they developed the Gamma Knife, a new device exclusively for radiosurgery, which consisted of radioactive sources of Cobalt-60 placed in a kind of helmet with central channels for irradiation, using gamma rays. In the latest version of this device, 192 sources of radioactive cobalt direct gamma radiation to the center of a helmet, where the patient's head is inserted. This is called the Leksell Gamma Knife Perfexion.
In order to achieve a high degree of precision, the patient's head is placed on a rigid frame of reference called a stereotactic frame that is inserted into a metal helmet.
A linear accelerator (LINAC) may also be used to deliver radiosurgery. LINAC based radiosurgery was pioneered at the University of Florida College of Medicine and introduced by Betti and Colombo in the mid 1980s. Modern LINACs optimized for radiosurgery applications include the Trilogy machine from Varian Medical Systems, and the Novalis Tx radiosurgery platform, produced by Varian and BrainLAB.
These systems differ from the Gamma Knife in a variety of ways. The Gamma Knife produces gamma rays from the decay of Co-60 of an average energy of 1.25 MeV. A LINAC produces x-rays from the impact of accelerated electrons striking a high z target (usually tungsten). A LINAC therefore can generate any number of energy x-rays, though usually 6 MV photons are used. The Gamma Knife has over ~200 sources arrayed in the helmet to deliver a variety of treatment angles. On a LINAC, the gantry moves in space to change the delivery angle. Both can move the patient in space to also change the delivery point. Both systems use a stereotactic frame to restrict the patient's movement, although on the Novalis Shaped Beam Radiosurgery system and the Novalis Tx radiosurgery platform, BrainLAB pioneered a frameless, non-invasive technique with X-ray imaging that has proven to be both comfortable for the patient and accurate. The Trilogy, from Varian, can also be used with non-invasive immobilization devices coupled with real-time imaging to detect any patient motion during a treatment.
At some medical centers such as in Boston and in California, particle accelerators built for doing research in high energy physics have been used since the 1960s for the treatment of brain tumors and arteriovenous malformations of the brain in humans.
Several generations of the frameless robotic Cyberknife system have been developed since its initial inception in 1990. It was invented by John R. Adler, a Stanford University Professor of Neurosurgery and Radiation Oncology and Russell and Peter Schonberg at SCHONBERG RESEARCH, and is sold by the Accuray company, located in Sunnyvale, California. Many such CyberKnife systems are available world-wide, and more recently it has been introduced in countries like India at leading cancer care hospitals like HCG Bangalore Institute of Oncology.
Varian Medical Systems of Palo Alto, California, made its first linear accelerator optimized for stereotactic radiosurgery in 1992, the Clinac 600SR. The Trilogy is another platform offered by Varian that incorporates tools for delivering highly-accurate image-guided radiotherapy and radiosurgery treatments, including cone-beam (3-D) and kV (2-D) imaging as well as respiratory gating to compensate for tumor motion during treatment. The Trilogy machine can also be outfitted with RapidArc for faster treatment delivery.
In 2007, the Novalis Tx radiosurgery platform was introduced by Varian and BrainLAB. The Novalis Tx radiosurgery platform incorporates sophisticated beam shaping technology, precision targeting computers and robotics that sculpt the treatment beam so that it envelops the tumor while avoiding the surrounding tissues and organs as much as possible. The Novalis Tx radiosurgery platform also offers a broad range of image-guidance tools to further enhance treatment precision. Clinicians are able to generate 3-D scans of the tumor and surrounding tissues prior to every treatment, to ensure that tumors are targeted accurately. The Novalis Shaped Beam Radiosurgery and Novalis Tx radiosurgery platforms are available worldwide, including the US, Europe, Japan, India, Australia, the Asia Pacific region, and the Middle East.
The latest radiosurgery technology available as of 2009 included the CyberKnife and Gamma Knife systems, the Novalis Tx radiosurgery platform, and the Trilogy linear accelerator.[9]
Stereotactic radiosurgery can successfully treat many different types of tumors, both benign and malignant. The malignant brain tumors treated most often are the "brain metastases" or tumors that have spread to the brain.[10] A study in 2008 by the University of Texas M. D. Anderson Cancer Center indicated that stereotactic radiosurgery (SRS) and whole brain radiation therapy (WBRT) for the treatment of metastatic brain tumours have more than twice the risk of developing learning and memory problems than those treated with SRS alone. “While both approaches are in practice and both are equally acceptable, data from this study suggest that oncologists should offer SRS alone as the upfront, initial therapy for patients with up to three brain metastases,”[11]
References
- ^ Régis J, Bartolomei F, Hayashi M, Chauvel P (2002). "What role for radiosurgery in mesial temporal lobe epilepsy". Zentralbl. Neurochir. 63 (3): 101–5. doi:10.1055/s-2002-35824. PMID 12457334.
- ^ Kwon Y, Whang CJ (1995). "Stereotactic Gamma Knife radiosurgery for the treatment of dystonia". Stereotact Funct Neurosurg 64 Suppl 1: 222–7. PMID 8584831.
- ^ Donnet A, Valade D, Régis J (February 2005). "Gamma knife treatment for refractory cluster headache: prospective open trial". J. Neurol. Neurosurg. Psychiatr. 76 (2): 218–21. doi:10.1136/jnnp.2004.041202. PMC 1739520. PMID 15654036. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1739520.
- ^ Herman JM, Petit JH, Amin P, Kwok Y, Dutta PR, Chin LS (May 2004). "Repeat gamma knife radiosurgery for refractory or recurrent trigeminal neuralgia: treatment outcomes and quality-of-life assessment". Int. J. Radiat. Oncol. Biol. Phys. 59 (1): 112–6. doi:10.1016/j.ijrobp.2003.10.041. PMID 15093906.
- ^ Chin LS, Lazio BE, Biggins T, Amin P (May 2000). "Acute complications following gamma knife radiosurgery are rare". Surg Neurol 53 (5): 498–502; discussion 502. doi:10.1016/S0090-3019(00)00219-6. PMID 10874151. http://linkinghub.elsevier.com/retrieve/pii/S0090-3019(00)00219-6.
- ^ Stafford SL, Pollock BE, Foote RL, et al. (November 2001). "Meningioma radiosurgery: tumor control, outcomes, and complications among 190 consecutive patients". Neurosurgery 49 (5): 1029–37; discussion 1037–8. doi:10.1097/00006123-200111000-00001. PMID 11846894. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0148-396X&volume=49&issue=5&spage=1029.
- ^ Cho DY, Tsao M, Lee WY, Chang CS (May 2006). "Socioeconomic costs of open surgery and gamma knife radiosurgery for benign cranial base tumors". Neurosurgery 58 (5): 866–73; discussion 866–73. doi:10.1227/01.NEU.0000209892.42585.9B. PMID 16639320.
- ^ "A Pinpoint Beam Strays Invisibly, Harming Instead of Healing". The New York Times. 2010-12-28. http://www.nytimes.com/2010/12/29/health/29radiation.html.
- ^ Latest radiosurgery treatments
- ^ John Hopkins - Stereotactic Radiosurgery
- ^ Whole brain radiation ups cancer patients learning, memory problems risk
- Principles and Practice of Stereotactic Radiosurgery, Lawrence Chin, MD and William Regine, MD, Editors (2008)
External links
- International RadioSurgery Association
- Understanding Stereotactic Radiosurgery. University of Florida.
- Academic Clinical Oncology & Radiobiology Research Network An NCRI initiative to revitalise radiotherapy research in the UK
- Computer Assisted Neurosurgery, University of Alabama at Birmingham
- Proton-Beam Radiosurgery, Massachusetts General Hospital, Harvard University.
- Gamma Knife Surgery for Tumors and Arteriovenous Malformations - University of Virginia Radiosurgical Center
- RTAnswers - Answers to Your Radiation Therapy Questions
- Gamma Knife Radiosurgery - Neurologic & Orthopedic Hospital of Chicago
- Sutter Gamma Knife Center - About Gamma Knife Radiosurgery, Physicians, Neurological Diseases Treated, Gamma Knife Video, FAQs
- Linear Particle Accelerator (Linac) Animation by Ionactive
- Novalis Circle - Novalis Circle worldwide network of clinicians dedicated to the advancement of radiosurgery
Manufacturers
- Elekta Instruments AB Home Page: manufacturer of Leksell's Gamma Knife
- Video: How Gamma Knife Works. University of Pennsylvania Gamma Knife Radiosurgery
- How Gamma Knife Works (Video)
- Varian Medical Systems: manufacturer of the Trilogy stereotactic linear accelerator and, with BrainLAB, the Novalis Tx radiosurgery platform
- Video: The Novalis Tx radiosurgery platform, about stereotactic body radiosurgery for lung cancer. University of California at Los Angeles.
- BrainLAB Manufacturer of the Novalis Shaped Beam Radiosurgery system and, with Varian Medical Systems, the Novalis Tx radiosurgery platform
- Accuray, Makers of the CyberKnife System
- Siemens Corporation's Oncology Care Systems Home Page: manufacturer of linear accelerators and radiation planning systems.
- Mevis Home Page: manufacturer of MNPS, a planning system with support for several stereotactic devices.
- Varian Oncology Systems Home Page: manufacturer of linear accelerators
- Radionics Stereotactic Radiosurgery System: XKnife System
- TomoTherapy Home Page Manufacturer of the TomoTherapy Hi·Art System
- Gammastar Home Page Manufacturer of the Gyro Knife - new generation of gamma knife
Nuclear technology Science Fuel Deuterium · Fertile material · Fissile · Isotope separation · Plutonium · Thorium · Tritium · Uranium (enriched • depleted)Neutron Activation · Capture · Cross-section · Fast · Fusion · Generator · Poison · Radiation · Reflector · Temp · ThermalReactors Boiling (BWR · ABWR) · Heavy (CANDU · PHWR · SGHWR) · Natural (NFR) · Pressurized (PWR · VVER · EPR) · Supercritical (SCWR)Advanced gas-cooled (AGR) · Magnox · Pebble bed (PBMR) · RBMK · UHTREX · Very high temperature (VHTR)FLiBeNone
(Fast)Breeder (FBR) · Integral (IFR) · Liquid-metal-cooled (LMFR) · SSTAR · Traveling Wave (TWR)
Generation IV by coolant: (Gas (GFR) · Lead (LFR) · Sodium (SFR))OtherPower Medicine TherapyWeapon TopicsListsWaste ProductsActinide: (Reprocessed uranium · Reactor-grade plutonium · Minor actinide) · Activation · Fission (LLFP)DisposalDebate Nuclear power debate · Nuclear weapons debate · Anti-nuclear movement · Uranium mining debate · Nuclear power phase-outRadiation oncology (ICD-9-CM V3 92.2-92.3, ICD-10-PCS D) Specific therapies 125I/103Pd (Prostate brachytherapy) · 125I (Plaque radiotherapy) · 90Y (Selective internal radiation therapy, SIR-Spheres, TheraSphere)131I (Iobenguane) · 90Y · 153Sm (Samarium (153Sm) lexidronam) · 89Sr
Radioimmunotherapy: 90Y (Ibritumomab tiuxetan)UngroupedConditions Other/ungrouped BEAMnrc · Bolus · Bragg peak · D50 · Dose profile · Dose verification system · Dose-volume histogram · Dosimetry · Isocenter · Mobetron · Monitor unit · Multileaf collimator · Nanoimpellers · Neutron generator · Oxygen enhancement ratio · Pencil · Pencil-beam scanning · Percentage depth dose curve · Radiation oncologist · Radiation treatment planning · Radiopharmacology · Tissue to Air RatioCategories:- Neurology procedures
- Radiobiology
- Radiation oncology
Wikimedia Foundation. 2010.