- Meningioma
-
Meningioma Classification and external resources 
A contrast enhanced CT scan of the brain, demonstrating the appearance of a Meningioma.ICD-10 C70, D32 ICD-9 225.2 ICD-O: M9530/0 OMIM 607174 DiseasesDB 8008 eMedicine neuro/209 radio/439 MeSH D008579 The word meningioma was first used by Harvey Cushing in 1922 to describe a tumor originating from the meninges, the membranous layers surrounding the CNS [1]. Meningiomas are the second most common primary neoplasm of the central nervous system, arising from the arachnoid "cap" cells of the arachnoid villi in the meninges.[2] These tumors are usually benign in nature; however, they can be malignant.[3]
Contents
Causes
Most cases are sporadic while some are familial. Persons who have undergone radiation to the scalp are more at risk for developing meningiomas.[4]
The most frequent genetic mutations involved in meningiomas are inactivation mutations in the neurofibromatosis 2 gene (merlin) on chromosome 22q.
Other possible genes/loci include:
Signs and symptoms
Small tumors (e.g., < 2.0 cm) are usually incidental findings at autopsy without having caused symptoms. Larger tumors can cause symptoms depending on the size and location.
- Focal seizures may be caused by meningiomas that overlie the cerebrum.
- Progressive spastic weakness in legs and incontinence may be caused by tumors that overlie the parasagittal frontoparietal region.
- Sylvian tumors may cause myriad motor, sensory, aphasic, and seizure symptoms, depending on the location.
- Increased intracranial pressure eventually occurs, but is less frequent than in gliomas.
Mechanism
Meningiomas arise from arachnoidal cells,[8] most of which are near the vicinity of the venous sinuses, and this is the site of greatest prevalence for meningioma formation. They are most frequently attached to the dura over the superior parasagittal surface of frontal and parietal lobes, along the sphenoid ridge, in the olfactory grooves, the sylvian region, superior cerebellum along the falx cerebri, cerebellopontine angle, and the spinal cord. The tumor is usually gray, well-circumscribed, and takes on the form of space it occupies. They are usually dome-shaped, with the base lying on the dura.
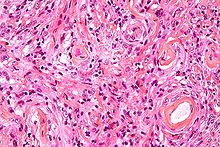
Histologically, the cells are relatively uniform, with a tendency to encircle one another, forming whorls and psammoma bodies (laminated calcific concretions).[9] They have a tendency to calcify and are highly vascularized.
Meningiomas are often considered benign tumors curable by surgery, but most recurrent meningiomas correspond to histologic benign tumors. The metabolic phenotype of these benign recurrent meningiomas indicated an aggressive metabolism resembling that observed for atypical meningioma [10] .
Diagnosis
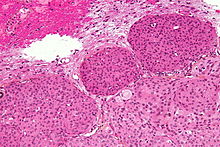 Micrograph of a meningioma with brain invasion (WHO Grade II); the tumour (bottom/right of image) has the typical "pushing border" invasion into the cerebral cortex (top/left of image). HPS stain.
Micrograph of a meningioma with brain invasion (WHO Grade II); the tumour (bottom/right of image) has the typical "pushing border" invasion into the cerebral cortex (top/left of image). HPS stain.
Meningiomas are readily visualized with contrast CT, MRI with gadolinium,[11] and arteriography, all attributed to the fact that meningiomas are extra-axial and vascularized. CSF protein is usually elevated if lumbar puncture is attempted.
Though the majority of meningiomas are benign, they can have malignant presentations. Classification of meningiomas are based upon the WHO classification system.[12]
- Benign (Grade I) - (90%) - meningothelial, fibrous, transitional, psammomatous, angioblastic (most aggressive)
- Atypical (Grade II) - (7%) - chordoid, clear cell, atypical (includes brain invasion)
- Anaplastic/malignant (Grade III) - (2%) - papillary, rhabdoid, anaplastic
In a recent retrospective review of atypical and anaplastic meningioma cases, the mean overall survival for atypical meningiomas was found to be 11.9 years vs. 3.3 years for anaplastic meningiomas. Mean relapse free survival for atypical meningiomas was 11.5 years vs. 2.7 years for anaplastic meningiomas.[13]
Malignant Anaplastic meningioma is an especially malignant tumor with aggressive behavior. Even if - by general rule - neoplasms of the nervous systems (brain tumors) cannot metastasize into the body (because of the blood-brain barrier) Anaplastic Meningioma can. Although they are inside the cerebral cavity, they are located on the bloodside of the BBB, because meningioma tend to "connect" themselves to bloodvessels to "feed". Cancerized cells can escape into the bloodstream. This is why meningioma when they metastasize often turn up around the lungs. It should be noted that Anaplastic meningioma and hemangiopericytoma are difficult to distinguish (even by pathological means), as they look similar, especially if the first occurrence is a meningeal tumor, and both tumors occur in the same places (same type of tissue)
Treatment
Observation
Observation with close imaging follow-up can be used in select cases if a meningioma is small and asymptomatic. In a retrospective study on 43 patients, 63% of patients were found to have no growth on follow-up, and the 37% found to have growth grew at an average of 4 mm / year.[14] In this study, younger patients were found to have tumors that were more likely to grow on repeat imaging, thus are poorer candidates for observation. In another study, clinical outcomes were compared for 213 patients undergoing surgery vs. 351 patient under watchful observation.[15] Only 6% of the conservatively treated patients later developed symptoms, while among the surgically treated patients, 5.6% developed persistent morbid condition, and 9.4% developed surgery-related morbid condition.
Observation is not recommended in tumors already causing symptoms. Furthermore, close follow-up with imaging is required with an observation strategy to rule out an enlarging tumor.[16]
Surgical resection
Meningiomas can usually be surgically resected with permanent cure if the tumor is superficial on the dural surface and easily accessible. Transarterial embolization has become a standard preoperative procedure in the preoperative management.[17] If invasion of the adjacent bone occurs, total removal is nearly impossible. Malignant transformation is rare.
The probability of tumor recurrence or growth after surgical resection can be estimated by the tumor's WHO Grade and by the extent of surgery by the Simpson Criteria.[18]
Simpson Grade Completeness of Resection 10-year Recurrence Grade I complete removal including resection of underlying bone and associated dura 9% Grade II complete removal + coagulation of dural attachment 19% Grade III complete removal w/o resection of dura or coagulation 29% Grade IV subtotal resection 40% Radiation therapy
Radiation therapy may include photon beam or proton beam treatment, or fractionated external beam radiation. Radiosurgery can be used in lieu of surgery in small tumors located away from critical structures.[19] Fractionated external beam radiation can also be used as primary treatment for tumors that are surgically unresectable, or for patients who are inoperable for medical reasons.
Radiation therapy is often considered for WHO Grade I meningiomas after subtotal (incomplete) tumor resections. The clinical decision to irradiate after a subtotal resection is somewhat controversial, as no class I randomized controlled trials exist on the subject.[20] Numerous retrospective studies, however, have strongly suggested the addition of postoperative radiation to incomplete resections improves both progression free survival (i.e. prevents tumor recurrence) and improves overall survival.[21]
In the case of a Grade III meningioma, the current standard of care involves postoperative radiation treatment regardless of the degree of surgical resection.[22] This is due to the proportionally higher rate of local recurrence for these higher grade tumors. Grade II tumors can behave variably and there is no standard of whether to give radiotherapy following a gross total resection. Subtotally resected grade II tumors should be radiated.
Conventional chemotherapy
Current chemotherapies are likely not effective. Antiprogestin agents have been used, but with variable results.[23] Recent evidence that hydroxyurea has the capacity to shrink unresectable or recurrent meningiomas is being further evaluated.[24]
References
- ^ Cushing H. (1922). "The meningiomas (dural endotheliomas): their source, and favoured seats of origin". Brain (45): 282–316. http://www.medmerits.com/index.php/article/meningiomas/P1.
- ^ Buetow MP, Buetow PC, Smirniotopoulos JG (November 1991). "Typical, atypical, and misleading features in meningioma". Radiographics 11 (6): 1087–106. PMID 1749851. http://radiographics.rsnajnls.org/cgi/pmidlookup?view=long&pmid=1749851. Retrieved 2008-12-01.
- ^ Goldsmith BJ, Wara WM, Wilson CB, Larson DA (February 1994). "Postoperative irradiation for subtotally resected meningiomas. A retrospective analysis of 140 patients treated from 1967 to 1990". J. Neurosurg. 80 (2): 195–201. doi:10.3171/jns.1994.80.2.0195. PMID 8283256.
- ^ Rabin BM; Meyer, JR; Berlin, JW; Marymount, MH; Palka, PS; Russell, EJ (September 1996). "Radiation-induced changes in the central nervous system and head and neck". Radiographics 16 (5): 1055–72. PMID 8888390. http://radiographics.rsnajnls.org/cgi/reprint/16/5/1055.
- ^ Lekanne Deprez RH, Riegman PH, Groen NA, et al. (April 1995). "Cloning and characterization of MN1, a gene from chromosome 22q11, which is disrupted by a balanced translocation in a meningioma". Oncogene 10 (8): 1521–8. PMID 7731706.
- ^ Staal FJ, van der Luijt RB, Baert MR, et al. (May 2002). "A novel germline mutation of PTEN associated with brain tumours of multiple lineages". Br. J. Cancer 86 (10): 1586–91. doi:10.1038/sj.bjc.6600206. PMC 2746590. PMID 12085208. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2746590.
- ^ Zattara-Cannoni H, Roll P, Figarella-Branger D, et al. (April 2001). "Cytogenetic study of six cases of radiation-induced meningiomas". Cancer Genet. Cytogenet. 126 (2): 81–4. doi:10.1016/S0165-4608(00)00398-8. PMID 11376799. http://linkinghub.elsevier.com/retrieve/pii/S0165-4608(00)00398-8.
- ^ "moon.ouhsc.edu". http://moon.ouhsc.edu/kfung/jty1/Com/Com306-1-Diss.htm. Retrieved 2008-11-30.
- ^ "Neuropathology For Medical Students". http://www.pathology.vcu.edu/WirSelfInst/neuro_medStudents/tumor-1.html. Retrieved 2008-11-30.
- ^ Monleón D, Morales JM, Gonzalez-Segura A, Gonzalez-Darder JM, Gil-Benso R, Cerdá-Nicolás M, López-Ginés C (November 2010). "Metabolic aggressiveness in benign meningiomas with chromosomal instabilities". Cancer Research 70 (21): 8426–8434. doi:10.1158/0008-5472.CAN-10-1498. PMID 20861191. http://cancerres.aacrjournals.org/content/70/21/8426.long.
- ^ Meningioma from Radiopaedia.org.
- ^ Wrobel G, Roerig P, Kokocinski F, et al. (March 2005). "Microarray-based gene expression profiling of benign, atypical and anaplastic meningiomas identifies novel genes associated with meningioma progression". Int. J. Cancer 114 (2): 249–56. doi:10.1002/ijc.20733. PMID 15540215.
- ^ Yang SY et al.: Atypical and anaplastic meningiomas: prognostic implications of clinicopathological features. J Neurol Neurosurg Psychiatry. 2008 May;79(5):574-80. Epub 2007 Aug 31.
- ^ Herscovici Z, et al.: Natural history of conservatively treated meningiomas." Neurology. 2004 Sep 28;63(6):1133-4.
- ^ Yano S, Kuratsu J.: Indications for surgery in patients with asymptomatic meningiomas based on an extensive experience. J Neurosurgery. 2006 Oct 105(4):538-43.
- ^ Olivero WC et al.: "The natural history and growth rate of asymptomatic meningiomas: a review of 60 patients." J Neurosurg. 1995 Aug;83(2):222-4
- ^ http://www.aans.org/education/journal/neurosurgical/july03/15-1-10.pdf
- ^ Simpson D. "The recurrence of intracranial meningiomas after surgical treatment." J Neurol Neurosurg Psychiatry. 1957 Feb;20(1):22-39.
- ^ Kullova A et al.: Radiosurgery for benign meningioma. J Neurosurg. 2007 Aug;107(2):325-36.
- ^ Taylor BW et al.: The meningioma controversy: postoperative radiation therapy. Int J Radiat Oncol Biol Phys. 1988 Aug;15(2):299-304.
- ^ Goldsmith BJ et al.: Postoperative irradiation for subtotally resected meningiomas. A retrospective analysis of 140 patients treated from 1967 to 1990. J Neurosurg. 1994 Feb;80(2):195-201.
- ^ Goyal LK et al. "Local control and overall survival in atypical meningioma: a retrospective study," Int J Radiat Oncol Biol Phys. 2000 Jan 1;46(1):57-61.
- ^ Wahab M et al.: Meningioma and hormonal influences. Climacteric. 2003 Dec;6(4):285-92.
- ^ Newton HB. Hydroxyurea chemotherapy in the treatment of meningiomas. Neurosurg Focus. 2007;23(4):E11.
External links
- Meningioma Information from the American Brain Tumor Association
- Meningioma information from the Mayo Clinic
- MR/CT scans of meningioma from MedPix
- CancerBackup
- MR/CT scans of pneumosinus dilatans from MedPix
- [1]
Nervous tissue tumors/NS neoplasm/Neuroectodermal tumor (ICD-O 9350–9589) (C70–C72, D32–D33, 191–192/225) Endocrine/
sellar (9350–9379)other: PinealomaCNS
(9380–9539)Astrocytoma (Pilocytic astrocytoma, Pleomorphic xanthoastrocytoma, Fibrillary (also diffuse or lowgrade) astrocytomas, Anaplastic astrocytoma, Glioblastoma multiforme)Multiple/unknownNeuroblastoma (Esthesioneuroblastoma, Ganglioneuroblastoma) · Medulloblastoma · Atypical teratoid rhabdoid tumorPrimitiveMeningioma, HemangiopericytomaHematopoieticPNS: NST
(9540–9579)cranial and paraspinal nerves: Neurofibroma (Neurofibrosarcoma, Neurofibromatosis) · Neurilemmoma/Schwannoma (Acoustic neuroma) · Malignant peripheral nerve sheath tumornote: not all brain tumors are of nervous tissue, and not all nervous tissue tumors are in the brain (see brain metastases)
Categories:- Nervous system neoplasia
- Brain tumor
Wikimedia Foundation. 2010.