- Medulloblastoma
-
Medulloblastoma Classification and external resources 
CT scan, showing a tumorous mass in the posterior fossa, giving rise to obstructive hydrocephalus, in a six year old girl.ICD-O: M9470/3 OMIM 155255 DiseasesDB 31105 eMedicine neuro/624 ped/1396 radio/434 MeSH D008527 Medulloblastoma is a highly malignant primary brain tumor that originates in the cerebellum or posterior fossa.
Previously, medulloblastomas were thought to represent a subset of primitive neuroectodermal tumor (PNET) of the posterior fossa. However, gene expression profiling has shown that medulloblastomas have a distinct molecular profile and are distinct from other PNET tumors.
Tumors that originate in the cerebellum are referred to as infratentorial because they occur below the tentorium, a thick membrane that separates the cerebral hemispheres of the brain from the cerebellum. Another term for medulloblastoma is infratentorial PNET. Medulloblastoma is the most common PNET originating in the brain.[1]
All PNET tumors of the brain are invasive and rapidly growing tumors that, unlike most brain tumors, spread through the cerebrospinal fluid (CSF) and frequently metastasize to different locations in the brain and spine.
Contents
Incidence
Brain tumors are the second most common malignancy among people under 20 years of age. Medulloblastoma is the most common malignant brain tumor, comprising 14.5% of newly diagnosed cases.[2] In adults, medulloblastoma is rare, comprising fewer than 2% of CNS malignancies.[3]
The incidence of childhood medulloblastoma is higher in males (62%) than females (38%).[4] Medulloblastoma and other PNET tumors are more prevalent in younger children than older children. 40% of medulloblastoma patients are diagnosed before the age of 5, 31% are between the ages of 5 and 9, 18.3% are between the ages of 10 and 14, and 12.7% are between the ages of 15 and 19.[5]
Pathogenesis
Medulloblastomas usually form in the vicinity of the fourth ventricle, between the brainstem and the cerebellum. Tumors with similar appearance and characteristics originate in other parts of the brain, but they are not identical to medulloblastoma.[6]
Although it is thought that medulloblastomas originate from immature or embryonal cells at their earliest stage of development, the exact cell of origin, or "medulloblast" has yet to be identified.[citation needed]
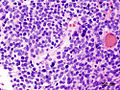
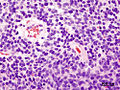
It is currently thought that medulloblastoma arises from cerebellar stem cells that have been prevented from dividing and differentiating into their normal cell types. This accounts from the varying histologic variants seen on biopsy. Both perivascular pseudorosette and Homer-Wright rosette pseudorosettes formation are highly characteristic of medulloblastoma and is seen in up to half of the cases. Homer-Wright rosettes are pseudorosettes consisting of tumor cells surrounding a fibrillar area.[7] Also, the classic rosette with tumor cells around a central lumen can be seen.[8]
Molecular genetics reveal a loss of genetic information on the distal part of chromosome 17, distal to the p53 gene, possibly accounting for the neoplastic transformation of the undifferentiated cerebellar cells. Medulloblastomas are also seen in Gorlin syndrome as well as Turcot syndrome. Other research has strongly implicated the JC virus, the virus that causes multifocal leukoencephalopathy.
Clinical manifestation
Symptoms are mainly due to secondary increased intracranial pressure due to blockage of the fourth ventricle and are usually present for 1 to 5 months before diagnosis is made. The child typically becomes listless, with repeated episodes of vomiting, and a morning headache, which may lead to a misdiagnosis of gastrointestinal disease or migraine. Soon, the child will develop a stumbling gait, frequent falls, diplopia, papilledema, and sixth cranial nerve palsy. Positional dizziness and nystagmus are also frequent and facial sensory loss or motor weakness may be present. Decerebrate attacks appear late in the disease.
Extraneural metastases to the rest of the body is rare, but usually only after craniotomy.
Diagnosis
The tumor is distinctive on T1 and T2-weighted MRI with heterogeneous enhancement and typical location adjacent to and extension into the fourth ventricle.
Histologically, the tumor is solid, pink-gray in color, and is well circumscribed. The tumor is very cellular, many mitoses, little cytoplasm, and has the tendency to form clusters and rosettes.
Correct diagnosis of medulloblastoma may require ruling out atypical teratoid rhabdoid tumor (ATRT)[9]
Treatment and prognosis
Treatment begins with maximal resection of the tumor. The addition of radiation to the entire neuraxis and chemotherapy may increase the disease-free survival. This combination may permit a 5 year survival in more than 80% of cases. The presence of desmoplastic features such as connective tissue formation offers a better prognosis. Prognosis is worse if the child is less than 3 years old, there is an inadequate degree of resection, or if there is any CSF, spinal, supratentorial or systemic spread. Dementia post radiotherapy and chemotherapy is a common outcome appearing two to four years following treatment.
Increased intracranial pressure may be controlled with corticosteroids or a ventriculoperitoneal shunt.
Chemotherapy
Chemotherapy is now an important part of treatment for all patients with medulloblastoma. It can significantly reduce risk of recurrence (which is typically fatal). There are a couple of different chemotheraputic regimens for medulloblastoma, but most involve a combination of lomustine, cisplatin, carboplatin, vincristine or cyclophosphamide. In younger patients (less than 3–4 years of age), chemotherapy can delay, or in some cases possibly even eliminate, the need for radiotherapy.[10]
Currently an NCI supported Phase I clinical trial involving the Curis/Genentech compound vismodegib (GDC-0449) is being evaluated in pediatric medulloblastoma patients, and has been tested in some PNET patients as well. This compound targets a cellular signalling pathway of the cancer cells, which controls how they divide and grow.
Outcome Prediction Based on Cytogenetic Subgroups
Array-based karyotyping of 260 medulloblastomas by Pfister S, et al. resulted in the following clinical subgroups based on cytogenetic profiles[11]:
- Poor prognosis: gain of 6q or amplification of MYC or MYCN
- Intermediate: gain of 17q or an i(17q) without gain of 6q or amplfication of MYC or MYCN
- Excellent prognosis: 6q and 17q balanced or 6q deletion
See also: Virtual KaryotypeSurvival
Patients diagnosed with a medulloblastoma or PNET are 50 times more likely to die than a matched member of the general population. The most recent population-based (SEER) 5-year relative survival rates are 69% overall, but 72% in children (1-9 years) and 67% in adults (20+ years). The 20 year survival rate is 51% in children. Children and adults have different survival profiles, with adults faring worse than children only after the 4th year post-diagnosis (after controlling for increased background mortality). Before the 4th year, survival probabilities are nearly identical.[12] Longterm sequalae of standard treatment include hypothalamic-pituitary and thyroid dysfunction and intellectual impairment. The hormonal and intellectual deficits created by these therapies causes significant impairment of the survivors.[13]
Model
Using gene transfer of SV40 large T-antigen in neuronal precursor cells of rats, a brain tumor model was established. The PNETs were histologically indistinguishable from the human counterparts and have been used to identify new genes involved in human brain tumor carcinogenesis.[14] The model was used to confirm p53 as one of the genes involved in human medulloblastomas, but since only about 10 % of the human tumors showed mutations in that gene, the model can be used to identify the other binding partners of SV40 Large T- antigen, other than p53.[15]
See also
- primitive neuroectodermal tumor
- malignant brain tumor
References
- ^ Chris Hinz, Deneen Hesser, Focusing On Brain Tumors: Medulloblastoma, American Brain Tumor Association 2006, ISBN 0-944093-67-1.
- ^ James G. Gurney, Malcolm A. Smith, Greta R. Bunin, CNS and Miscellaneous Intracranial and Intraspinal Neoplasms, SEER Pediatric Monograph, National Cancer Institute
- ^ Selected Primary Brain and Central Nervous System Tumor Age-Specific Incidence Rates, Central Brain Tumor Registry of the United States, 1998-2002.
- ^ Selected Childhood Primary Brain and Central Nervous System Tumor Incidence Rates by Major Histology Groupings, Histology and Gender Central Brain Tumor Registry of the United States, 1998-2002.
- ^ Selected Childhood Primary Brain and Central Nervous System Tumor Age-Specific Incidence Rates, Central Brain Tumor Registry of the United States, 1998-2002.
- ^ Roger Packer M.D, Medulloblastoma Clinical Trials and Noteworthy Treatments for Brain Tumors 2002.
- ^ White Lucile E, Levy Ross M, Alam Murad, "Chapter 127. Neoplasias and Hyperplasias of Muscular and Neural Origin" (Chapter). Wolff K, Goldsmith LA, Katz SI, Gilchrest B, Paller AS, Leffell DJ: Fitzpatrick's Dermatology in General Medicine, 7e: http://www.accessmedicine.com/content.aspx?aID=2983360.
- ^ Ropper AH, Samuels MA, "Chapter 31. Intracranial Neoplasms and Paraneoplastic Disorders" (Chapter). Ropper AH, Samuels MA: Adams and Victor's Principles of Neurology, 9e: http://www.accessmedicine.com/content.aspx?aID=3637579.
- ^ Burger PC; Yu I, Tihan T, et al. (1998). "Atypical teratoid rhabdoid tumors of the central nervous system: a highly malignant tumor of infancy and childhood frequently mistaken for medulloblastoma: a Pediatric Oncology Group Study.". Am J Surg Pathol 1998 22 (22:): 1083–92. doi:10.1097/00000478-199809000-00007. PMID 9737241.
- ^ www.ABTA.org
- ^ Pfister S, et al. Outcome Prediction in Pediatric Medulloblastoma based on DNA Copy Number Aberrations of Chromosomes 6q and 17q and the MYC and MYCN Loci. J Clin Oncol 2009 Apr(27)10;1627-1636.
- ^ Smoll NR (August 2011). "Relative survival of childhood and adult medulloblastomas and primitive neuroectodermal tumors (PNETs)". Cancer. doi:10.1002/cncr.26387. PMID 21837678.
- ^ Medulloblastoma by Roger J. Packer, MD Senior Vice-President, Neuroscience and Behavioral Medicine Director, Brain Tumor Institute Director, Gilbert Neurofibromatosis Institute Children’s National Medical Center Washington, DC Written for the Childhood Brain Tumor Foundation, Germantown, Maryland 20876, (Updated 1/2010)
- ^ Eibl RH, Kleihues P, Jat PS, Wiestler OD (1994) A model for primitive neuroectodermal tumors in transgenic neural transplants harboring the SV40 large T antigen. Am J Pathol. 1994 Mar;144(3):556-64.
- ^ Ohgaki H, Eibl RH, Wiestler OD, Yasargil MG, Newcomb EW, Kleihues P: p53 mutations in nonastrocytic human brain tumors. Cancer Res (1991) 51:6202-5
Additional images
External links
- Samantha Dickson Brain Tumour Trust: brain tumour research and support charity
- Brain and Spinal Tumors: Hope Through Research (National Institute of Neurological Disorders and Stroke)
- Medulloblastoma support resources
- 00905 at CHORUS
- HELP KIDS NOW WITH MEDULLOBLASTOMA
- I'll get better tomorrow (2009) a documentary film following for 16 months the treatments of 3 children with medulloblastoma.
- Medulloblastoma Images MedPix Medical Image Database
- Latest news and research on medulloblastoma
Nervous tissue tumors/NS neoplasm/Neuroectodermal tumor (ICD-O 9350–9589) (C70–C72, D32–D33, 191–192/225) Endocrine/
sellar (9350–9379)other: PinealomaCNS
(9380–9539)Astrocytoma (Pilocytic astrocytoma, Pleomorphic xanthoastrocytoma, Fibrillary (also diffuse or lowgrade) astrocytomas, Anaplastic astrocytoma, Glioblastoma multiforme)Multiple/unknownNeuroblastoma (Esthesioneuroblastoma, Ganglioneuroblastoma) · Medulloblastoma · Atypical teratoid rhabdoid tumorPrimitiveHematopoieticPNS: NST
(9540–9579)cranial and paraspinal nerves: Neurofibroma (Neurofibrosarcoma, Neurofibromatosis) · Neurilemmoma/Schwannoma (Acoustic neuroma) · Malignant peripheral nerve sheath tumornote: not all brain tumors are of nervous tissue, and not all nervous tissue tumors are in the brain (see brain metastases)
B-cell chronic lymphocytic leukemia · Hepatoblastoma · Rhabdomyosarcoma · Ewing's sarcoma · Neuroblastoma · Retinoblastoma · Wilms' tumor · Desmoplastic small round cell tumor · Medulloblastoma · Primitive neuroectodermal tumor (PNET)Categories:- Small blue round cell tumor
- Brain tumor
Wikimedia Foundation. 2010.