- Thalassemia
-
Thalassemia Classification and external resources ICD-10 D56 ICD-9 282.4 MedlinePlus 000587 eMedicine ped/2229 radio/686 MeSH D013789 Thalassemia (British English: thalassaemia) is an inherited autosomal recessive blood disease that originated in the Mediterranean region. In thalassemia the genetic defect, which could be either mutation or deletion, results in reduced rate of synthesis or no synthesis of one of the globin chains that make up hemoglobin. This can cause the formation of abnormal hemoglobin molecules, thus causing anemia, the characteristic presenting symptom of the thalassemias.
Thalassemia is a quantitative problem of too few globins synthesized, whereas sickle-cell disease (a hemoglobinopathy) is a qualitative problem of synthesis of an incorrectly functioning globin. Thalassemias usually result in underproduction of normal globin proteins, often through mutations in regulatory genes. Hemoglobinopathies imply structural abnormalities in the globin proteins themselves.[1] The two conditions may overlap, however, since some conditions that cause abnormalities in globin proteins (hemoglobinopathy) also affect their production (thalassemia). Thus, some thalassemias are hemoglobinopathies, but most are not. Either or both of these conditions may cause anemia.
The two major forms of the disease, alpha- and beta- (see below), are prevalent in discrete geographical clusters around the world - it is presumed associated with malarial endemicity in ancient times. Alpha is prevalent in peoples of Western African and South Asian descent. It is nowadays found in populations living in Africa and in the Americas. It is also found in Tharu in the Terai region of Nepal and India.[2] It is believed to account for much lower malaria morbidity and mortality,[3] accounting for the historic ability of Tharus to survive in heavily malarial areas where others could not.
Beta thalassemia is particularly prevalent among Mediterranean peoples, and this geographical association is responsible for its naming: Thalassa (θάλασσα) is Greek for the sea, Haema (αἷμα) is Greek for blood. In Europe, the highest concentrations of the disease are found in Greece, coastal regions in Turkey, in particular, Aegean Region such as Izmir, Balikesir, Aydin, Mugla, and Mediterranean Region such as Antalya, Adana, Mersin, in parts of Italy, in particular, Southern Italy and the lower Po valley. The major Mediterranean islands (except the Balearics) such as Sicily, Sardinia, Malta, Corsica, Cyprus, and Crete are heavily affected in particular. Other Mediterranean people, as well as those in the vicinity of the Mediterranean, also have high rates of thalassemia, including people from West Asia and North Africa. Far from the Mediterranean, South Asians are also affected, with the world's highest concentration of carriers (16% of the population) being in the Maldives.
The thalassemia trait may confer a degree of protection against malaria, which is or was prevalent in the regions where the trait is common, thus conferring a selective survival advantage on carriers (known as heterozygous advantage), and perpetuating the mutation. In that respect, the various thalassemias resemble another genetic disorder affecting hemoglobin, sickle-cell disease.[4] [5]
Contents
Etymology
First use: 1932
Origin: New Latin, from Greek thalassa, meaning "sea" and New Latin -emia, meaning "blood". The etymology indicates the epidemiology of the disorder in that it is commonly seen in patients of Mediterranean descent.
Epidemiology
Generally, thalassemias are prevalent in populations that evolved in humid climates where malaria was endemic. It affects all races, as thalassemias protected these people from malaria due to the blood cells' easy degradation.
Thalassemias are particularly associated with people of Mediterranean origin, Arabs, and Asians.[6] The Maldives has the highest incidence of Thalassemia in the world with a carrier rate of 18% of the population. The estimated prevalence is 16% in people from Cyprus, 1%[7] in Thailand, and 3-8% in populations from Bangladesh, China, India, Malaysia and Pakistan. There are also prevalences in descendants of people from Latin America and Mediterranean countries (e.g. Greece, Italy, Portugal, Spain, and others). A very low prevalence has been reported from people in Northern Europe (0.1%) and Africa (0.9%), with those in North Africa having the highest prevalence. It is also particularly common in populations of indigenous ethnic minorities of Upper Egypt such as the Beja, Hadendoa, Sa'idi and also peoples of the Nile Delta, Red Sea Hill Region and especially amongst the Siwans.
Pathophysiology
Normal hemoglobin is composed of four protein chains, two α and two β globin chains arranged into a heterotetramer. Thalassemia patients produce a deficiency of either α or β globin, unlike sickle-cell disease, which produces a specific mutant form of β globin.
The thalassemias are classified according to which chain of the hemoglobin molecule is affected. In α thalassemias, production of the α globin chain is affected, while in β thalassemia production of the β globin chain is affected.
The β globin chains are encoded by a single gene on chromosome 11; α globin chains are encoded by two closely linked genes on chromosome 16. Thus, in a normal person with two copies of each chromosome, there are two loci encoding the β chain, and four loci encoding the α chain. Deletion of one of the α loci has a high prevalence in people of African or Asian descent, making them more likely to develop α thalassemias. β Thalassemias are common in Africans, but also in Greeks and Italians.
Alpha (α) thalassemias
Main article: Alpha-thalassemiaThe α thalassemias involve the genes HBA1[8] and HBA2,[9] inherited in a Mendelian recessive fashion. There are two gene loci and so four alleles. It is also connected to the deletion of the 16p chromosome. α Thalassemias result in decreased alpha-globin production, therefore fewer alpha-globin chains are produced, resulting in an excess of β chains in adults and excess γ chains in newborns. The excess β chains form unstable tetramers (called Hemoglobin H or HbH of 4 beta chains), which have abnormal oxygen dissociation curves.
Beta (β) thalassemias
Main article: Beta-thalassemiaBeta thalassemias are due to mutations in the HBB gene on chromosome 11 ,[10] also inherited in an autosomal-recessive fashion. The severity of the disease depends on the nature of the mutation. Mutations are characterized as either βo or β thalassemia major if they prevent any formation of β chains, the most severe form of β thalassemia. Also, they are characterized as β+ or β thalassemia intermedia if they allow some β chain formation to occur. In either case, there is a relative excess of α chains, but these do not form tetramers: Rather, they bind to the red blood cell membranes, producing membrane damage, and at high concentrations they form toxic aggregates.
Delta (δ) thalassemia
Main article: Delta-thalassemiaAs well as alpha and beta chains present in hemoglobin, about 3% of adult hemoglobin is made of alpha and delta chains. Just as with beta thalassemia, mutations that affect the ability of this gene to produce delta chains can occur[citation needed].
In combination with other hemoglobinopathies
Thalassemia can co-exist with other hemoglobinopathies. The most common of these are:
- hemoglobin E/thalassemia: common in Cambodia, Thailand, and parts of India; clinically similar to β thalassemia major or thalassemia intermedia.
- hemoglobin S/thalassemia, common in African and Mediterranean populations; clinically similar to sickle cell anemia, with the additional feature of splenomegaly
- hemoglobin C/thalassemia: common in Mediterranean and African populations, hemoglobin C/βo thalassemia causes a moderately severe hemolytic anemia with splenomegaly; hemoglobin C/β+ thalassemia produces a milder disease.
Cause
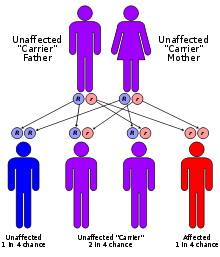
Both α and β thalassemias are often inherited in an autosomal recessive fashion, although this is not always the case. Cases of dominantly inherited α and β thalassemias have been reported, the first of which was in an Irish family with two deletions of 4 and 11 bp in exon 3 interrupted by an insertion of 5 bp in the β-globin gene. For the autosomal recessive forms of the disease, both parents must be carriers in order for a child to be affected. If both parents carry a hemoglobinopathy trait, there is a 25% risk with each pregnancy for an affected child. Genetic counseling and genetic testing is recommended for families that carry a thalassemia trait.
There are an estimated 60-80 million people in the world carrying the beta thalassemia trait alone.[citation needed] This is a very rough estimate; the actual number of thalassemia major patients is unknown due to the prevalence of thalassemia in less developed countries.[citation needed] Countries such as India and Pakistan are seeing a large increase of thalassemia patients due to lack of genetic counseling and screening.[citation needed] There is growing concern that thalassemia may become a very serious problem in the next 50 years, one that will burden the world's blood bank supplies and the health system in general.[citation needed] There are an estimated 1,000 people living with thalassemia major in the United States and an unknown number of carriers.[citation needed] Because of the prevalence of the disease in countries with little knowledge of thalassemia, access to proper treatment and diagnosis can be difficult.[citation needed]
Treatment
Medical care
- Mild thalassemia : patients with thalassemia traits do not require medical or follow-up care after the initial diagnosis is made.[11] Patients with β-thalassemia
trait should be warned that their blood picture resembles iron deficiency and can be misdiagnosed. They should eschew empirical use of Iron therapy; yet iron deficiency can develop during pregnancy or from chronic bleeding.[12] Counseling is indicated in all persons with genetic disorders, especially when the family is at risk of a severe form of disease that may be prevented.[13]
- Severe thalassemia : patients with severe thalassemia require medical treatment, and a blood transfusion regimen was the first measure effective in prolonging life.[11]
Medication
Medical therapy for beta thalassemia primarily involves iron chelation. Deferoxamine is the intravenously or subcutaneously administered chelation agent currently approved for use in the United States. Deferasirox (Exjade) is an oral iron chelation drug also approved in the US in 2005. Deferiprone is an oral iron chelator that has been approved in Europe since 1999 and many other countries. It is available under compassionate use guidelines in the United States.
The antioxidant indicaxanthin, found in beets, in a spectrophotometric study showed that indicaxanthin can reduce perferryl-Hb generated in solution from met-Hb and hydrogen peroxide, more effectively than either Trolox or Vitamin C. Collectively, results demonstrate that indicaxanthin can be incorporated into the redox machinery of β-thalassemic RBC and defend the cell from oxidation, possibly interfering with perferryl-Hb, a reactive intermediate in the hydroperoxide-dependent Hb degradation.[14]
Carrier detection
- A screening policy exists in Cyprus to reduce the incidence of thalassemia, which since the program's implementation in the 1970s (which also includes pre-natal screening and abortion) has reduced the number of children born with the hereditary blood disease from 1 out of every 158 births to almost zero.[15]
- In Iran as a premarital screening, the man's red cell indices are checked first, if he has microcytosis (mean cell hemoglobin < 27 pg or mean red cell volume < 80 fl), the woman is tested. When both are microcytic their hemoglobin A2 concentrations are measured. If both have a concentration above 3.5% (diagnostic of thalassemia trait) they are referred to the local designated health post for genetic counseling.[16]
In 2008, in Spain, a baby was selectively implanted in order to be a cure for his brother's thalassemia. The child was born from an embryo screened to be free of the disease before implantation with In vitro fertilization. The baby's supply of immunocompatible cord blood was saved for transplantation to his sister. The transplantation was considered successful.[17] In 2009, a group of doctors and specialists in Chennai and Coimbatore registered the successful treatment of thalassemia in a child using a sibling's umbilical cord blood.[18]
Benefits
Epidemiological evidence from Kenya suggests another reason: protection against severe malarial anemia may be the advantage.[19]
People diagnosed with heterozygous (carrier) β thalassemia have some protection against coronary heart disease.[20]
Complications
- Iron overload: People with thalassemia can get too much iron in their bodies, either from the disease itself or from frequent blood transfusions. Too much iron can result in damage to the heart, liver and endocrine system, which includes glands that produce hormones that regulate processes throughout the body. The damage is characterized by excessive iron deposition. Without adequate iron chelation therapy, almost all patients with beta-thalassemia will accumulate potentially fatal iron levels.[21]
- Infection: people with thalassemia have an increased risk of infection. This is especially true if the spleen has been removed.
- Bone deformities: Thalassemia can make the bone marrow expand, which causes bones to widen. This can result in abnormal bone structure, especially in the face and skull. Bone marrow expansion also makes bones thin and brittle, increasing the risk of broken bones.
- Enlarged spleen: the spleen aids in fighting infection and filters unwanted material, such as old or damaged blood cells. Thalassemia is often accompanied by the destruction of a large number of red blood cells, and the task of removing these cells causes the spleen to enlarge. Splenomegaly can make anemia worse, and it can reduce the life of transfused red blood cells. Severe enlargement of the spleen may necessitate its removal.
- Slowed growth rates: anemia can cause a child's growth to slow. Puberty also may be delayed in children with thalassemia.
- Heart problems: such as congestive heart failure and abnormal heart rhythms (arrhythmias), may be associated with severe thalassemia.[22]
References
- ^ Hemoglobinopathies and Thalassemias
- ^ Modiano, G. et al. (1991). "Protection against malaria morbidity: Near-fixation of the α-thalassemia gene in a Nepalese population". American Journal of Human Genetics 48 (2): 390–397. PMC 1683029. PMID 1990845. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1683029.
- ^ Terrenato, L. et al. (1988). "Decreased Malaria Morbidity in the Tharu People Compared to Sympatric Populations in Nepal". Annals of Tropical Medicine and Parasitology 82 (1): 1–11. PMID 3041928.
- ^ Weatherall David J, "Chapter 47. The Thalassemias: Disorders of Globin Synthesis" (Chapter). Lichtman MA, Kipps TJ, Seligsohn U, Kaushansky K, Prchal, JT: Williams Hematology, 8e: http://www.accessmedicine.com/content.aspx?aID=6123722.
- ^ Mayoclinic. http://www.mayoclinic.com/health/thalassemia/DS00905/DSECTION=complications. Retrieved 20 September 2011.
- ^ E. Goljan, Pathology, 2nd ed. Mosby Elsevier, Rapid Review Series.
- ^ http://www.dmsc.moph.go.th/webrOOt/ri/Npublic/p04.htm
- ^ Online 'Mendelian Inheritance in Man' (OMIM) 141800
- ^ Online 'Mendelian Inheritance in Man' (OMIM) 141850
- ^ Online 'Mendelian Inheritance in Man' (OMIM) 141900
- ^ a b "Pediatric Thalassemia Treatment & Management". Medical Care. Open Publishing. 30 April 2010. http://emedicine.medscape.com/article/958850-treatment/. Retrieved 27 September 2011.
- ^ Claude Owen Burdick. "Separating Thalassemia Trait and Iron Deficiency by Simple Inspection". American Society for Clinical Pathology. http://ajcp.ascpjournals.org/content/131/3/444.short/. Retrieved 27 September 2011.
- ^ * Harrison's Principles of Internal Medicine 17th Edition. McGraw-Hill medical. September 2008. pp. 776. ISBN 0-07-164114-9.
- ^ Tesoriere L, Allegra M, Butera D, Gentile C, Livrea MA (July 2006). "Cytoprotective effects of the antioxidant phytochemical indicaxanthin in beta-thalassemia red blood cells". Free Radical Research 40 (7): 753–61. doi:10.1080/10715760600554228. PMID 16984002.
- ^ Leung TN, Lau TK, Chung TKh (April 2005). "Thalassaemia screening in pregnancy". Current Opinion in Obstetrics & Gynecology 17 (2): 129–34. doi:10.1097/01.gco.0000162180.22984.a3. PMID 15758603.
- ^ Samavat A, Modell B (November 2004). "Iranian national thalassaemia screening programme". BMJ (Clinical Research Ed.) 329 (7475): 1134–7. doi:10.1136/bmj.329.7475.1134. PMC 527686. PMID 15539666. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=527686.
- ^ Spanish Baby Engineered To Cure Brother
- ^ His sister's keeper: Brother's blood is boon of life, Times of India, 17 September 2009
- ^ Wambua S, Mwangi TW, Kortok M et al. (May 2006). "The Effect of α +-Thalassaemia on the Incidence of Malaria and Other Diseases in Children Living on the Coast of Kenya". PLoS Medicine 3 (5): e158. doi:10.1371/journal.pmed.0030158. PMC 1435778. PMID 16605300. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1435778.
- ^ Tassiopoulos S, Deftereos S, Konstantopoulos K et al. (2005). "Does heterozygous beta-thalassemia confer a protection against coronary artery disease?". Annals of the New York Academy of Sciences 1054: 467–70. doi:10.1196/annals.1345.068. PMID 16339699.
- ^ Ospedale S. Eugenio; Deftereos, Spyros; Konstantopoulos, Kostas; Farmakis, Dimitris; Tsironi, Maria; Kyriakidis, Michalis; Aessopos, Athanassios (2008). "Treatment of iron overload in thalassemia". Pubmed 1054: 208–13. doi:10.1196/annals.1345.068. PMID 19337180.
- ^ "Thalassemia Complications". Thalassemia. Open Publishing. http://www.mayoclinic.com/health/thalassemia/DS00905/DSECTION=complications/. Retrieved 27 September 2011.
External links
- GeneReviews/NCBI/NIH/UW entry on Alpha-Thalassemia
- OMIM etries on Alpha-Thalassemia
- Thalassemia at the Open Directory Project
- Cooley's Anemia Foundation
- Information on Thalassemia
- Learning About Thalassemia published by the National Human Genome Research Institute.
- [1] - A patients' help group and support forum
- Northern California's Comprehensive Thalassemia Center
- Thalassemia Community Forum
- FerriScan - MRI-based test to measure iron overload
Categories:- Autosomal recessive disorders
- Hereditary hemolytic anemias
- Disorders of globin and globulin proteins
Wikimedia Foundation. 2010.