- Methemoglobinemia
-
Methemoglobinemia Classification and external resources ICD-10 D74 ICD-9 289.7 DiseasesDB 8100 eMedicine med/1466 emerg/313 ped/1432 MeSH D008708 Methemoglobinemia (or methaemoglobinaemia) is a disorder characterized by the presence of a higher than normal level of methemoglobin (metHb) in the blood. Methemoglobin is an oxidized form of hemoglobin that has an increased affinity for oxygen, resulting in a reduced ability to release oxygen to tissues. The oxygen–hemoglobin dissociation curve is shifted to the left. When methemoglobin concentration is elevated in red blood cells, tissue hypoxia can occur.
Contents
Overview
Normally, methemoglobin levels are <1%, as measured by the co-oximetry test. Elevated levels of methemoglobin in the blood are caused when the mechanisms that defend against oxidative stress within the red blood cell are overwhelmed and the oxygen carrying ferrous ion (Fe2+) of the heme group of the hemoglobin molecule is oxidized to the ferric state (Fe3+). This converts hemoglobin to methemoglobin, resulting in a reduced ability to release oxygen to tissues and thereby hypoxia. This can give the blood a bluish or chocolate-brown color. Spontaneous formation of methemoglobin is normally reduced (via electron donation) by protective enzyme systems, e.g. NADH methemoglobin reductase (cytochrome-b5 reductase) (major pathway), NADPH methemoglobin reductase (minor pathway) and to a lesser extent the ascorbic acid and glutathione enzyme systems. Disruptions with these enzyme systems lead to the condition.
Types
Congenital methemoglobinemia
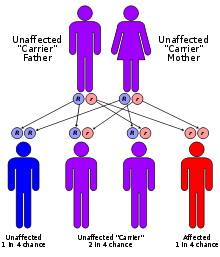
Due to a deficiency of the enzyme diaphorase I (NADH methemoglobin reductase), methemoglobin levels rise and the blood of met-Hb patients has reduced oxygen-carrying capacity. Instead of being red in color, the arterial blood of met-Hb patients is brown. This results in the skin of Caucasian patients gaining a bluish hue. Hereditary met-Hb is caused by a recessive gene. If only one parent has this gene, offspring will have normal-hued skin, but if both parents carry the gene there is a chance the offspring will have blue-hued skin.
Another cause of congenital methemoglobinemia is seen in patients with abnormal hemoglobin variants such as hemoglobin M (HbM), or hemoglobin H (HbH), which are not amenable to reduction despite intact enzyme systems.
Methemoglobinemia can also arise in patients with pyruvate kinase deficiency due to impaired production of NADH – the essential cofactor for diaphorase I. Similarly, patients with Glucose-6-phosphate dehydrogenase (G6PD) deficiency may have impaired production of another co-factor, NADPH.
Acquired methemoglobinemia
Methemoglobinemia can also be acquired.[1] The protective enzyme systems normally present in red blood cells maintain methemoglobin levels at less than one percent of the total hemoglobin in healthy people. Exposure to exogenous oxidizing drugs and their metabolites (such as benzocaine, dapsone and nitrates) may accelerate the rate of formation of methemoglobin up to one-thousandfold, overwhelming the protective enzyme systems and acutely increasing methemoglobin levels.
Other classical drug causes of methemoglobinemia include antibiotics (trimethoprim, sulfonamides and dapsone[2]), local anesthetics (especially articaine and prilocaine[3]), and others such as aniline dyes, metoclopramide, chlorates and bromates. Ingestion of compounds containing nitrates (such as the patina chemical bismuth nitrate) can also cause methemoglobinemia.
Infants under 6 months of age are particularly susceptible to methemoglobinemia caused by nitrates ingested in drinking water[citation needed] (called blue-baby syndrome), dehydration usually caused by gastroenteritis with diarrhea, sepsis, and topical anesthetics containing benzocaine or prilocaine. Nitrates used in agricultural fertilizers may leak into the ground and may contaminate well water. The current EPA standard of 10 ppm nitrate-nitrogen for drinking water is specifically designed to protect infants[citation needed].
Benzocaine applied to the gums or throat (as commonly used in baby teething gels) can cause methemoglobinemia.[1]
Treatment
Methemoglobinemia can be treated with supplemental oxygen and methylene blue[4] 1% solution (10 mg/ml) 1 to 2 mg/kg administered intravenously slowly over five minutes followed by IV flush with normal saline. Methylene blue restores the iron in hemoglobin to its normal (reduced) oxygen-carrying state.
This is achieved by providing an artificial electron acceptor (such as methylene blue, or flavin) for NADPH methemoglobin reductase (RBCs usually don't have one; the presence of methylene blue allows the enzyme to function at 5x normal levels[5]) The NADPH is generated via the hexose monophosphate shunt.
Diaphorase II normally contributes only a small percentage of the red blood cells reducing capacity but is pharmacologically activated by exogenous cofactors, such as methylene blue, to 5 times its normal level of activity. Genetically induced chronic low-level methemoglobinemia may be treated with oral methylene blue daily. Also, vitamin C can occasionally reduce cyanosis associated with chronic methemoglobinemia but has no role in treatment of acute acquired methemoglobinemia.
Symptoms
Signs and symptoms of methemoglobinemia (methemoglobin >1%) include shortness of breath, cyanosis, mental status changes (~50%), headache, fatigue, exercise intolerance, dizziness and loss of consciousness. Arterial blood with elevated methemoglobin levels has a characteristic chocolate-brown color as compared to normal bright red oxygen containing arterial blood.[6]
Severe methemoglobinemia (methemoglobin >50%) patients have dysrhythmias, seizures, coma and death (>70%).[6] Healthy people may not have many symptoms with methemoglobin levels < 15%, however patients with co-morbidities such as anemia, cardiovascular disease, lung disease, sepsis, or presence of other abnormal hemoglobin species (e.g. carboxyhemoglobin, sulfehemoglobin or sickle hemoglobin) may experience moderate to severe symptoms at much lower levels (as low as 5-8%).
Carriers
The Fugates, a family that lived in the hills of Kentucky, are the most famous example of this hereditary genetic condition. They are known as the "Blue Fugates." Martin Fugate settled near Hazard, Kentucky, circa 1800. His wife was a carrier of the recessive methemoglobinemia (met-H) gene, as was a nearby clan with whom the Fugates intermarried. As a result, many descendants of the Fugates were born with met-H.[7][8]
The "blue men of Lurgan" were a pair of Lurgan men suffering from what was described as "familial idiopathic methaemoglobinaemia" who were treated by Dr. James Deeny in 1942. Deeny, who would later become the Chief Medical Officer of the Republic of Ireland, prescribed a course of ascorbic acid and sodium bicarbonate. In case one, by the eighth day of treatment there was a marked change in appearance and by the twelfth day of treatment the patient's complexion was normal. In case two, the patient's complexion reached normality over a month-long duration of treatment.[9]
References
- ^ Ash-Bernal R, Wise R, Wright SM (2004). "Acquired methemoglobinemia: a retrospective series of 138 cases at 2 teaching hospitals". Medicine (Baltimore) 83 (5): 265–273. PMID 15342970. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0025-7974&volume=83&issue=5&spage=265.
- ^ Zosel A, Rychter K, Leikin JB (2007). "Dapsone-induced methemoglobinemia: case report and literature review". Am J Ther 14 (6): 585–587. doi:10.1097/MJT.0b013e3180a6af55. PMID 18090884. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?an=00045391-200711000-00012.
- ^ Adams V, Marley J, McCarroll C (2007). "Prilocaine induced methaemoglobinaemia in a medically compromised patient. Was this an inevitable consequence of the dose administered?". Br Dent J 203 (10): 585–587. doi:10.1038/bdj.2007.1045. PMID 18037845.
- ^ Yusim Y, Livingstone D, Sidi A (2007). "Blue dyes, blue people: the systemic effects of blue dyes when administered via different routes". J Clin Anesth 19 (4): 315–321. doi:10.1016/j.jclinane.2007.01.006. PMID 17572332. http://linkinghub.elsevier.com/retrieve/pii/S0952-8180(07)00085-2.
- ^ Yubisui T; Takeshita M; Yoneyama Y. Reduction of methemoglobin through flavin at the physiological concentration by NADPH-flavin reductase of human erythrocytes. J Biochem (Tokyo) 1980 Jun;87(6):1715-20. PMID 7400118
- ^ a b "eMedicine - Methemoglobinemia". http://www.emedicine.com/med/topic1466.htm. Retrieved 2008-09-13.
- ^ Straight Dope article on the Fugates of Appalachia, an extended family of blue-skinned people
- ^ Tri City Herald, November 7, 1974 p.32 Newspaper reports on the Blue Fugates
- ^ Deeny, James (1995). The End of an Epidemic. Dublin: A.& A.Farmar. ISBN 1-899047-06-9.
External links
- ATSDR Case Studies in Environmental Medicine: Nitrate/Nitrite Toxicity U.S. Department of Health and Human Services (public domain)
- The Blue People of Troublesome Creek
Categories:- Red blood cell disorders
- Autosomal recessive disorders
Wikimedia Foundation. 2010.