- Cerebral infarction
-
Cerebral infarct Classification and external resources 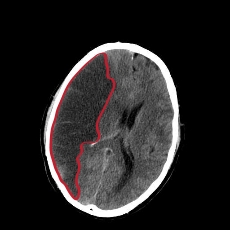
CT scan slice of the brain showing a right-hemispheric cerebral infarct (left side of image).ICD-10 I 63 ICD-9 434.01, 434.11, 434.91 eMedicine neuro/ MeSH D002544 A cerebral infarction is the ischemic kind of stroke due to a disturbance in the blood vessels supplying blood to the brain. It can be atherothrombotic or embolic.[1] Stroke caused by cerebral infarction should be distinguished from two other kinds of stroke: cerebral hemorrhage and subarachnoid hemorrhage. A cerebral infarction occurs when a blood vessel that supplies a part of the brain becomes blocked or leakage occurs outside the vessel walls. This loss of blood supply results in the death of that area of tissue. Cerebral infarctions vary in their severity with one third of the cases resulting in death.
Contents
Classification
There are various classification systems for a cerebral infarction.
- The Oxford Community Stroke Project classification (OCSP, also known as the Bamford or Oxford classification) relies primarily on the initial symptoms. Based on the extent of the symptoms, the stroke episode is classified as total anterior circulation infarct (TACI), partial anterior circulation infarct (PACI), lacunar infarct (LACI) or posterior circulation infarct (POCI). These four entities predict the extent of the stroke, the area of the brain affected, the underlying cause, and the prognosis.[2][3]
- The TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification is based on clinical symptoms as well as results of further investigations; on this basis, a stroke is classified as being due to (1) thrombosis or embolism due to atherosclerosis of a large artery, (2) embolism of cardiac origin, (3) occlusion of a small blood vessel, (4) other determined cause, (5) undetermined cause (two possible causes, no cause identified, or incomplete investigation).[4]
Symptoms
Symptoms of cerebral infarction are determined by topographical localisation of cerebral lesion. If the infarct is located in primary motor cortex- contralateral hemiparesis is said to occur. With brainstem localization, brainstem syndromes are typical: Wallenberg's syndrome, Weber's syndrome, Millard-Gubler syndrome, Benedikt syndrome or others. Infarctions will result in weakness and loss of sensation on the opposite side of the body. Physical examination of the head area will reveal abnormal pupil dilation, light reaction and lack of eye movement on opposite side. If the infarction occurs on the left side brain, speech will be slurred. Reflexes may be aggravated as well.
Causes
In thrombotic cerebral infarction a thrombus usually forms around atherosclerotic plaques. An embolic stroke refers to the blockage of an artery by an embolus, a traveling particle or debris in the arterial bloodstream originating elsewhere. An embolus is most frequently a thrombus, but it can also be a number of other substances including fat (e.g. from bone marrow in a broken bone), air, cancer cells or clumps of bacteria (usually from infectious endocarditis). The embolus may be of cardiac origin or from atherosclerotic plaque of another (or the same) large artery.
Risk factors
Risk factors for cerebral infarction are generally the same as for atherosclerosis: diabetes, tobacco smoking, hypercholesterolemia, hyperlipoproteinemia, high blood pressure, obesity.
Diagnosis
Computed tomography (CT) and MRI scanning will show damaged area in the brain, showing that the symptoms were not caused by a tumor, subdural hematoma or other brain disorder. The blockage will also appear on the angiogram.
Treatment
In last decade, similar to myocardial infarction treatment, thrombolytic drugs were introduced in the therapy of cerebral infarction. The use of intravenous rtPA therapy can be advocated in patients who arrive to stroke unit and can be fully evaluated within 3 h of the onset.
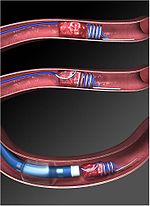
If cerebral infarction is caused by a thrombus occluding blood flow to an artery supplying the brain, definitive therapy is aimed at removing the blockage by breaking the clot down (thrombolysis), or by removing it mechanically (thrombectomy). The more rapidly blood flow is restored to the brain, the fewer brain cells die.[5] In increasing numbers of primary stroke centers, pharmacologic thrombolysis with the drug tissue plasminogen activator (tPA), is used to dissolve the clot and unblock the artery. Another intervention for acute cerebral ischaemia is removal of the offending thrombus directly. This is accomplished by inserting a catheter into the femoral artery, directing it into the cerebral circulation, and deploying a corkscrew-like device to ensnare the clot, which is then withdrawn from the body. Mechanical embolectomy devices have been demonstrated effective at restoring blood flow in patients who were unable to receive thrombolytic drugs or for whom the drugs were ineffective,[6][7][8][9] though no differences have been found between newer and older versions of the devices.[10] The devices have only been tested on patients treated with mechanical clot embolectomy within eight hours of the onset of symptoms.
Angioplasty and stenting have begun to be looked at as possible viable options in treatment of acute cerebral ischaemia. In a systematic review of six uncontrolled, single-center trials, involving a total of 300 patients, of intra-cranial stenting in symptomatic intracranial arterial stenosis, the rate of technical success (reduction to stenosis of <50%) ranged from 90-98%, and the rate of major peri-procedural complications ranged from 4-10%. The rates of restenosis and/or stroke following the treatment were also favorable.[11] This data suggests that a large, randomized controlled trial is needed to more completely evaluate the possible therapeutic advantage of this treatment.
If studies show carotid stenosis, and the patient has residual function in the affected side, carotid endarterectomy (surgical removal of the stenosis) may decrease the risk of recurrence if performed rapidly after cerebral infarction. Carotid endarterectomy is also indicated to decrease the risk of cerebral infarction for symptomatic carotid stenosis (>70 to 80 reduction in diameter). [12]
In tissue losses that are not immediately fatal, the best course of action is to make every effort to restore impairments through physical therapy, speech therapy and exercise.References
- ^ Ropper, Allan H.; Adams, Raymond Delacy; Brown, Robert F.; Victor, Maurice (2005). Adams and Victor's principles of neurology. New York: McGraw-Hill Medical Pub. Division. pp. 686–704. ISBN 0-07-141620-X.
- ^ Bamford J, Sandercock P, Dennis M, Burn J, Warlow C (June 1991). "Classification and natural history of clinically identifiable subtypes of cerebral infarction". Lancet 337 (8756): 1521–6. doi:10.1016/0140-6736(91)93206-O. PMID 1675378. http://linkinghub.elsevier.com/retrieve/pii/0140-6736(91)93206-O. Later publications distinguish between "syndrome" and "infarct", based on evidence from imaging. "Syndrome" may be replaced by "hemorrhage" if imaging demonstrates a bleed. See Internet Stroke Center. "Oxford Stroke Scale". http://www.strokecenter.org/trials/scales/oxford.html. Retrieved 2008-11-14.
- ^ Bamford JM (2000). "The role of the clinical examination in the subclassification of stroke". Cerebrovasc. Dis. 10 Suppl 4: 2–4. doi:10.1159/000047582. PMID 11070389.
- ^ Adams HP, Bendixen BH, Kappelle LJ, et al. (January 1993). "Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment" (PDF). Stroke 24 (1): 35–41. doi:10.1161/01.STR.24.1.35. PMID 7678184. http://stroke.ahajournals.org/cgi/reprint/24/1/35.
- ^ Saver JL (2006). "Time is brain - quantified". Stroke 37 (37): 263–6. doi:10.1161/01.STR.0000196957.55928.ab. PMID 16339467. http://stroke.ahajournals.org/cgi/content/abstract/01.STR.0000196957.55928.abv1.
- ^ Flint AC, Duckwiler GR, Budzik RF, Liebeskind DS, Smith WS (2007). "Mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and Multi MERCI Part I trials". Stroke 38 (4): 1274–80. doi:10.1161/01.STR.0000260187.33864.a7. PMID 17332445.
- ^ Smith WS, Sung G, Starkman S, et al. (2005). "Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial". Stroke 36 (7): 1432–8. doi:10.1161/01.STR.0000171066.25248.1d. PMID 15961709. http://stroke.ahajournals.org/cgi/content/full/36/7/1432.
- ^ Lutsep HL, Rymer MM, Nesbit GM (2008). "Vertebrobasilar revascularization rates and outcomes in the MERCI and multi-MERCI trials". J Stroke Cerebrovasc Dis 17 (2): 55–7. doi:10.1016/j.jstrokecerebrovasdis.2007.11.003. PMID 18346645.
- ^ Smith WS (June 1, 2006). "Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part I". AJNR Am J Neuroradiol 27 (6): 1177–82. PMID 16775259. http://www.ajnr.org/cgi/content/full/27/6/1177.
- ^ Smith WS, Sung G, Saver J, et al. (2008). "Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial". Stroke 39 (4): 1205–12. doi:10.1161/STROKEAHA.107.497115. PMID 18309168.
- ^ Derdeyn CP, Chimowitz MI (August 2007). "Angioplasty and Stenting for Atherosclerotic Intracranial Stenosis: Rationale for a Randomized Clinical Trial". Neuroimaging Clin. N. Am. 17 (3): 355–63, viii–ix. doi:10.1016/j.nic.2007.05.001. PMC 2040119. PMID 17826637. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2040119.
- ^ Ropper, A.H.; Brown, R.H. (2005). Adams and Victor's Principles of Neurology. pp. 698. ISBN 0-07-141620-X
Pathology: hemodynamics Decreases general: Anemic infarct · Hemorrhagic infarct
regional: Myocardial infarction · Cerebral infarction · Splenic infarction · Limb infarctionIncreases general Bruise/Hematoma: Petechia · Purpura · Ecchymosis
regional: head (Epistaxis, Hemoptysis, Intracranial hemorrhage, Hyphema, Subconjunctival hemorrhage) · torso (Hemothorax, Hemopericardium, Pulmonary hematoma) · abdomen (Gastrointestinal bleeding, Haemobilia, Hemoperitoneum, Hematocele, Hematosalpinx ) · joint (Hemarthrosis)general: Anasarca · Angioedema/Lymphedema · Exudate/Transudate
regional: Cerebral edema · Pulmonary edema · Hydrothorax · Ascites/hydroperitoneum · HydrosalpinxOtherCNS disease, Vascular disease: Cerebrovascular diseases (G45–G46 and I60–I69, 430–438) Brain ischemia/
cerebral infarction
(ischemic stroke/TIA)Intracranial hemorrhage
(hemorrhagic stroke)Extra-axialBrainstemAneurysm Other/general Categories:
Wikimedia Foundation. 2010.