- Emphysema
-
For the condition describing air trapped under the skin, see subcutaneous emphysema.
Emphysema Classification and external resources
A lateral chest x-ray of a person with emphysema. Note the barrel chest and flat diaphragm.ICD-10 J43 ICD-9 492 DiseasesDB 4190 MedlinePlus 000136 eMedicine med/654 MeSH D011656 Emphysema is a long-term, progressive disease of the lungs that primarily causes shortness of breath. In people with emphysema, the tissues necessary to support the physical shape and function of the lungs are destroyed. It is included in a group of diseases called chronic obstructive pulmonary disease or COPD (pulmonary refers to the lungs). Emphysema is called an obstructive lung disease because the destruction of lung tissue around smaller sacs, called alveoli, makes these air sacs unable to hold their functional shape upon exhalation. It is often caused by long-term exposure to air pollution or smoking.
The term emphysema means swelling and comes from the Greek ἐμφυσᾶν emphysan meaning inflate, itself composed of ἐν en meaning in and φυσᾶν physan meaning breath, blast.[1]
Contents
Classification
Emphysema can be classified into primary and secondary. However, it is more commonly classified by location into panacinary and centroacinary (or panacinar and centriacinar,[2] or centrilobular and panlobular).[3]
- Panacinar (or panlobular) emphysema: The entire respiratory acinus, from respiratory bronchiole to alveoli, is expanded. Occurs more commonly in the lower lobes, especially basal segments, and anterior margins of the lungs.[2]
- Centriacinar (or centrilobular) emphysema: The respiratory bronchiole (proximal and central part of the acinus) is expanded. The distal acinus or alveoli are unchanged. Occurs more commonly in the upper lobes.[2]
Other types include distal acinar and irregular.[2] A special type is congenital lobar emphysema (CLE).
Congenital lobar emphysema
CLE results in overexpansion of a pulmonary lobe and resultant compression of the remaining lobes of the ipsilateral lung, and possibly also the contralateral lung. There is bronchial narrowing because of weakened or absent bronchial cartilage.[4] There may be congenital extrinsic compression, commonly by an abnormally large pulmonary artery. This causes malformation of bronchial cartilage, making them soft and collapsible.[4] CLE is potentially reversible, yet possibly life-threatening, causing respiratory distress in the neonate.[4]
Paraseptal emphysema
Paraseptal emphysema is a type of emphysema which involves the alveolar ducts and sacs at the lung periphery. The emphysematous areas are subpleural in location and often surrounded by interlobular septa (hence the name). It may be an incidental finding in young adults, and may be associated with spontaneous pneumothorax. It may also be seen in older patients with centrilobular emphysema. Both centrilobular and paraseptal emphysema may progress to bullous emphysema. A bulla is defined as being at least 1 cm in diameter, and with a wall less than 1mm thick. Bullae are thought to arise by air trapping in emphysematous spaces, causing local expansion.[5]
Signs and symptoms
Emphysema is a disease of the lung tissue caused by destruction of structures feeding the alveoli, in some cases owing to the action of alpha 1-antitrypsin deficiency. Smoking is one major cause of this destruction, which causes the small airways in the lungs to collapse during forced exhalation. As a result, airflow is impeded and air becomes trapped, just as in other obstructive lung diseases. Symptoms include shortness of breath on exertion, and an expanded chest.
People with this disease do not get enough oxygen and cannot remove carbon dioxide from their blood; they therefore exhibit dyspnea (shortness of breath). At first this occurs only during physical activity. Eventually it will occur after any physical exertion. Later the patient may be dyspneic all the time, even when relaxing. Because breathing is difficult, the patient must use accessory muscles to help them breathe; tachypnea (rapid breathing) may occur when they try to extend their exertion. They may have trouble coughing and lowered amounts of sputum. They may also lose weight.
The anteroposterior diameter of their chest may increase; this symptom is sometimes referred as "barrel chest." The patient may lean forward with arms extended or resting on something to help them breathe.
When lung auscultation and chest percussion is performed a hyperresonant sound is heard.
The patient may also exhibit symptoms of hypoxia-induced cyanosis, or the appearance of a blue to purplish discoloration of the skin, due to increased levels of deoxyhemoglobin in the blood.
Causes
The majority of all emphysema cases are caused by smoking tobacco. Emphysema cases that are caused by other etiologies are referred to as secondary emphysema.[citation needed]
In some cases it may be due to alpha 1-antitrypsin deficiency. Severe cases of A1AD may also develop cirrhosis of the liver, where the accumulated A1AT leads to a fibrotic reaction.
Some types of emphysema are considered a normal part of aging and are found in the elderly whose lungs have deteriorated due to age. At about 20 years of age, people stop developing new alveoli tissue. In the years following the cessation of the development of new alveoli, lung tissue can start to deteriorate. This is a normal, natural part of aging in healthy people. Alveoli will die, the number of lung capillaries will decline and the elastin of the lungs will begin to break down causing a loss of pulmonary elasticity. As people age, they will also lose strength and mass in their chest muscles causing these muscles to become weaker. In addition, bones can start to deteriorate and a person’s posture can change. Together, all of these age-related manifestations can cause the development of emphysema. Though not all elderly people will develop emphysema, they are all at risk of having decreased respiratory function.
Other causes of emphysema can be anything that causes the body to be unable to inhibit proteolytic enzymes in the lung. This could be exposure to air pollution, second hand smoke or other chemicals and toxins.[citation needed]
Pathophysiology
In normal breathing, air is drawn in through the bronchi and into the alveoli, which are tiny sacs surrounded by capillaries. Alveoli absorb oxygen and then transfer it into the blood. When toxicants, such as cigarette smoke, are breathed into the lungs, the harmful particles become trapped in the alveoli, causing a localized inflammatory response. Chemicals released during the inflammatory response (e.g., elastase) can eventually cause the alveolar septum to disintegrate. This condition, known as septal rupture, leads to significant deformations of the lung architecture[6][7] (video) that have important functional consequences. The key mechanical event consequent to septal rupture is that the resulting cavity is larger than the sum of the two alveolar spaces (see figure); in fact because of the lacking mechanical support of the broken septa the lung elastic recoil further enlarges this new space, necessarily at the expenses of the surrounding healthy parenchyma. In other words, as immediate and spontaneous consequence of septal rupture, the elastic lung recoil resets healthy parenchyma expansion at a lower level, in proportion to the amount of septal disruption. The large cavities left by the septal rupture are known as bullae. These deformations result in a large decrease of alveoli surface area used for gas exchange, as well as decreased ventilation of the surrounding healthy parenchyma. This results in a decreased Transfer Factor of the Lung for Carbon Monoxide (TLCO). To accommodate the decreased surface area, thoracic cage expansion (barrel chest) and diaphragm contraction (flattening) take place. Expiration, which physiologically depends completely on lung elastic recoil, increasingly depends on the thoracic cage and abdominal muscle action, particularly in the end expiratory phase. Due to decreased ventilation, the ability to exude carbon dioxide is significantly impaired. In the more serious cases, oxygen uptake is also impaired. As the alveoli continue to break down, hyperventilation is unable to compensate for the progressively shrinking surface area, and the body is not able to maintain high enough oxygen levels in the blood. The body's last resort is vasoconstricting appropriate vessels. This leads to pulmonary hypertension, which places increased strain on the right side of the heart, the side responsible for pumping deoxygenated blood to the lungs. The heart muscle thickens in order to pump more blood. This condition is often accompanied by the appearance of jugular venous distension. Eventually, as the heart continues to fail, it becomes larger and blood backs up in the liver.
Patients with alpha 1-antitrypsin deficiency (A1AD) are more likely to suffer from emphysema. A1AT inhibits inflammatory enzymes (such as elastase) from destroying the alveolar tissue. Most A1AD patients do not develop clinically significant emphysema, but smoking and severely decreased A1AT levels (10-15%) can cause emphysema at a young age. The type of emphysema caused by A1AD is known as panacinar emphysema (involving the entire acinus) as opposed to centrilobular emphysema, which is caused by smoking. Panacinar emphysema typically affects the lower lungs, while centrilobular emphysema affects the upper lungs. A1AD causes about 2% of all emphysema. Smokers with A1AD are at the greatest risk for emphysema. Mild emphysema can often develop into a severe case over a short period of time (1–2 weeks).
While A1AD provides some insight into the pathogenesis of the disease, hereditary A1AT deficiency only accounts for a small proportion of the disease. Studies for the better part of the past century have focused mainly upon the putative role of leukocyte elastase (also neutrophil elastase), a serine protease found in neutrophils, as a primary contributor to the connective tissue damage seen in the disease. This hypothesis, a result of the observation that neutrophil elastase is the primary substrate for A1AT, and A1AT is the primary inhibitor of neutrophil elastase, together have been known as the "protease-antiprotease" theory, implicating neutrophils as an important mediator of the disease. However, more recent studies have brought into light the possibility that one of the many other numerous proteases, especially matrix metalloproteases might be equally or more relevant than neutrophil elastase in the development of non-hereditary emphysema.
The better part of the past few decades of research into the pathogenesis of emphysema involved animal experiments where various proteases were instilled into the trachea of various species of animals. These animals developed connective tissue damage, which was taken as support for the protease-antiprotease theory. However, just because these substances can destroy connective tissue in the lung, as anyone would be able to predict, doesn't establish causality. More recent experiments have focused on more technologically advanced approaches, such as ones involving genetic manipulation. One particular development with respect to our understanding of the disease involves the production of protease "knock-out" animals, which are genetically deficient in one or more proteases, and the assessment of whether they would be less susceptible to the development of the disease. Often individuals who are unfortunate enough to contract this disease have a very short life expectancy, often 0–3 years at most.
Diagnosis
The diagnosis is usually confirmed by pulmonary function testing (e.g. spirometry); however, X-ray radiography may aid in the diagnosis. A DLCO test may be used to differentiate Emphysema from other types of Obstructive disorders such as Chronic Bronchitis and Asthma. DLCO is a test that measures the ability of gases to diffuse across the alveolar-capillary membrane. A DLCO will be decreased in Emphysema whereas it will be normal or increased in Asthma and Chronic Bronchitis.
-
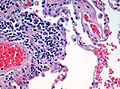
Micrograph demonstrating emphysema (left of image - large empty spaces) and lung tissue with relative preservation of the alveoli (right of image). H&E stain.
Management
Emphysema is an irreversible degenerative condition. Patients who think they may have contracted the disease are recommended to seek medical attention as soon as possible. The most important measure to slow its progression is for the patient to stop smoking and avoid all exposure to cigarette smoke and lung irritants. Pulmonary rehabilitation can be very helpful to optimize the patient's quality of life and teach the patient how to actively manage his or her care.
Emphysema is also treated by supporting the breathing with anticholinergics, bronchodilators, steroid medication (inhaled or oral), effective body positioning (high Fowler's), and supplemental oxygen as required. Treating the patient's other conditions including gastric reflux and allergies may improve lung function. Supplemental oxygen used as prescribed (usually more than 20 hours per day) is the only non-surgical treatment which has been shown to prolong life in emphysema patients. There are lightweight portable oxygen systems which allow patients increased mobility. Patients can fly, cruise, and work while using supplemental oxygen. Other medications are being researched.
Lung volume reduction surgery (LVRS) can improve the quality of life for certain carefully selected patients. It can be done by different methods, some of which are minimally invasive. In July 2006 a new treatment, placing tiny valves in passages leading to diseased lung areas, was announced to have good results, but 7% of patients suffered partial lung collapse.
The only known "cure" for emphysema is lung transplant, but few patients are strong enough physically to survive the surgery. The combination of a patient's age, oxygen deprivation and the side-effects of the medications used to treat emphysema cause damage to the kidneys, heart and other organs. Surgical transplantation also requires the patient to take an anti-rejection drug regimen which suppresses the immune system, and can lead to microbial infection of the patient.
With the discovery of multipotent lung stem cells in 2011, a new treatment option may soon become available. Scientists injected human lung stem cells into mice with damaged lungs. The stem cells formed human bronchioles, alveoli, and pulmonary vessels integrated structurally and functionally with the damaged mouse organ. The May 2011 report in the New England Journal of Medicine [8] concluded that human lung stem cells "have the undemonstrated potential to promote tissue restoration in patients with lung disease".
Notable cases
- Amy Winehouse[9]
- Dick York[10]
- Don Imus[11]
- Johnny Carson[12][13]
- Leonard Nimoy[14]
- Paul Avery[15]
- R. J. Reynolds, R. J. Reynolds Jr., R. J. Reynolds, III,[16]
- Spencer Tracy[17]
Footnotes
- ^ emphysema at dictionary.com
- ^ a b c d "Emphysema". http://www.meddean.luc.edu/Lumen/MedEd/MEDICINE/PULMONAR/pathms/mpath6.htm. Retrieved 2008-11-20.
- ^ Anderson AE, Foraker AG (September 1973). "Centrilobular emphysema and panlobular emphysema: two different diseases". Thorax 28 (5): 547–50. doi:10.1136/thx.28.5.547. PMC 470076. PMID 4784376. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=470076.
- ^ a b c eMedicine Specialties > Radiology > Pediatrics --> Congenital Lobar Emphysema Author: Beverly P Wood, MD, MS, PhD, University of Southern California. Updated: December 1, 2008
- ^ Webb WR, Higgins CB. Thoracic Imaging. Lippincott, Williams & Wilkins 2005.
- ^ S. Nazari : Mechanical Events In Physiopathology Of Idiopathic Pulmonary Emphysema: A Theoretical Analysis. The Internet Journal of Thoracic and Cardiovascular Surgery. 2002 Volume 5 Number 2
- ^ Nazari S.The surgical physiopathology of essential pulmonary emphysema and volume-reduction intervention. Minerva Chir. 1998 Nov;53(11):899-918. PMID: 9973794
- ^ "Evidence for Human Lung Stem Cells". New England Journal of Medicine. http://www.nejm.org/doi/full/10.1056/NEJMoa1101324. Retrieved 07-12-2011.
- ^ "Amy Winehouse Health Problems". http://en.wikipedia.org/wiki/Amy_Winehouse#Health_problems.
- ^ Secter, Bob (1989-02-08). "Bewitched by a Cause : Dick York Is Dying of Emphysema but He Lives to Help the Homeless". Los Angeles Times. http://articles.latimes.com/1989-02-08/news/vw-2079_1_dick-york. Retrieved 2011-07-12.
- ^ "Don Imus's Last Stand: Politics & Power". Vanityfair.com. 2009-01-06. http://www.vanityfair.com/politics/features/2006/02/imus200602?currentPage=2. Retrieved 2009-09-12.
- ^ Longtime host of ‘Tonight Show’ dies at 79 Associated Press, February 8, 2005
- ^ Net mourns death of Johnny Carson Jeff Pelline CNET News February 8, 2005
- ^ "Girth and Nudity, a Pictorial Mission". Nytimes.com. 2007-05-13. http://www.nytimes.com/2007/05/13/fashion/13nimoy.html. Retrieved 2010-10-02.
- ^ music (2008-10-27). "Amy Winehouse rushed to hospital". Entertainment.uk.msn.com. http://entertainment.uk.msn.com/music/news/nme/article.aspx?cp-documentid=10434337>1=61501. Retrieved 2009-09-12.[dead link]
- ^ "Death from Smoking in the R. J. Reynolds Family by Patrick Reynolds". Tobaccofree.org. http://www.tobaccofree.org/famobit.htm. Retrieved 2009-09-12.
- ^ "Spencer Tracy". Hollywood.com. http://www.hollywood.com/celebrity/Spencer_Tracy/196686. Retrieved 2009-09-12.
External links
- Images of Emphysema http://www.radrounds.com/photo/paraseptal-and-centrilobular-1
- The Internet Pathology Laboratory for Medical Education of Mercer University School of Medicine
Categories:- Chronic lower respiratory diseases
- Smoking
Wikimedia Foundation. 2010.