- Xeroderma pigmentosum
-
"XP1" redirects here. For the phone, see Sonim XP1 ToughPhone.
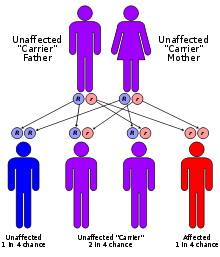
Xeroderma pigmentosum Classification and external resources ICD-10 Q82.1 ICD-9 757.33 DiseasesDB 14198 eMedicine derm/462 neuro/399 MeSH D014983 Xeroderma pigmentosum, or XP, is an autosomal recessive genetic disorder of DNA repair in which the ability to repair damage caused by ultraviolet (UV) light is deficient.[1]:574 In extreme cases, all exposure to sunlight must be forbidden, no matter how small. Multiple basal cell carcinomas (basaliomas) and other skin malignancies frequently occur at a young age in those with XP. In fact, metastatic malignant melanoma and squamous cell carcinoma[2] are the two most common causes of death in XP victims. This disease involves both sexes and all races, with an incidence of 1:250,000 and a gene frequency of 1:200. XP is roughly six times more common in Japanese people[2] than in other groups.
The most common defect in xeroderma pigmentosum is an autosomal recessive genetic defect in which nucleotide excision repair (NER) enzymes are mutated, leading to a reduction in or elimination of NER.[3] If left unchecked, damage caused by ultraviolet (UV) light can cause mutations in individual cell's DNA. If tumor suppressor genes (e.g. p53) or proto oncogenes are affected, the result may be cancer. Patients with XP are at a high risk for developing skin cancers, such as basal cell carcinoma, for this reason.
Normally, damage to DNA in epidermal cells occurs during exposure to UV light. The absorption of the high energy light leads to the formation of pyrimidine dimers, namely cyclobutane-pyrimidine dimers) and pyrimidine-6-4-pyrimidone photoproducts). In a healthy, normal human being, the damage is first excised by endonucleases. DNA polymerase then repairs the missing sequence, and ligase "seals" the transaction. This process is known as nucleotide excision repair.
Contents
Types
There are seven complementation groups, plus one variant form:
Type Diseases Database OMIM Gene Locus Also known as/Description Type A, I, XPA 29877 278700 XPA 9q22.3 Xeroderma pigmentosum group A - the classical form of XP Type B, II, XPB 29878 133510 XPB 2q21 Xeroderma pigmentosum group B Type C, III, XPC 29879 278720 XPC 3p25 Xeroderma pigmentosum group C Type D, IV, XPD 29880 278730 278800 XPD ERCC6 19q13.2-q13.3 , 10q11 Xeroderma pigmentosum group D or De Sanctis-Cacchione syndrome (can be considered a subtype of XPD) Type E, V, XPE 29881 278740 DDB2 11p12-p11 Xeroderma pigmentosum group E Type F, VI, XPF 29882 278760 ERCC4 16p13.3-p13.13 Xeroderma pigmentosum group F Type G, VII, XPG 29883 278780 133530 RAD2 ERCC5 13q33 Xeroderma pigmentosum group G and COFS syndrome type 3 Type V, XPV 278750 POLH 6p21.1-p12 Xeroderma pigmentosum variant - these patients suffer from mutation in a gene that codes for a specialized DNA polymerase called polymerase-η (eta). Polymerase-η can replicate over the damage and is needed when cells enter S-phase in the presence of a DNA-damage. Symptoms
Some of the most common symptoms of XP include:
- A severe sunburn when exposed to only small amounts of sunlight. Often occurring during a child's first exposure to sunlight.
- Development of many freckles at an early age
- Rough-surfaced growths (solar keratoses), and skin cancers
- Eyes that are painfully sensitive to the sun and may easily become irritated, bloodshot, and clouded
- Blistering or freckling on minimum sun exposure
- Spidery blood vessels
- Oozing raw skin surfaces
- Limited growth of hair on chest and legs
- Scaly skin
- Irregular dark spots on the skin
Treatment
The most obvious, and often important part of treatment, is avoiding exposure to sunlight. Keratoses can also be treated using cryotherapy or fluorouracil.[4] A few places specialize in XPS treatment, one of most notable being Camp Sundown in Craryville, New York.
Prognosis
Fewer than 40% of individuals with the disease survive beyond age 20 years. Some XP victims with less severe cases do manage to live well into their 40s.
In popular culture
These fictional characters have XP:
- Christopher Snow in Dean Koontz's Moonlight Bay Trilogy
- In the 2002 novel Going Out by Scarlett Thomas, Luke
- Children of the main character in Alejandro Amenábar's 2001 film, The Others
- In the Japanese movie Taiyou no Uta also known as Midnight Sun, the main character (Kaoru Amane)
- In the ITV series Ultraviolet, one of the humans is mistaken for a vampire because he avoids sunlight, when in fact he has XP.
- In the independent film Dark Side of the Sun (1988) with Brad Pitt as the main character suffering from XP.
- In the 2003 novel Second Glance by Jodi Picoult, Ethan Wakeman, the 9-year-old nephew of Ross Wakeman (the main protagonist)
- The 2003 Angela Johnson novel, A Cool Moonlight, centers on a girl who has XP and can never be in the sun. The family has gone to drastic measures to help make her life easier, and to make her feel like a normal 8-year-old.
- The 2011 film La permission de minuit by French director Delphine Gleize centers on a teenage boy with XP.
See also
- Biogerontology
- Cockayne syndrome
- Photophobia
- Senescence
- List of cutaneous conditions
References
- ^ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0721629210.
- ^ a b Li, Lei (January 8, 2007). "Chapter 3 Nucleotide Excision Repair". DNA REPAIR, GENETIC INSTABILITY, AND CANCER. World Scientific Publishing. pp. 75–76. ISBN 9812700145.
- ^ E. C. Friedberg, G. C. Walker, W. Siede, R. D. Wood, R. A. Schultz and T. Ellenberger (2006). DNA repair and mutagenesis. Washington: ASM Press. p. 1118. ISBN 978-1555813192.
- ^ Halpern, J.; Hopping, B.; Brostoff, J. (2008). "Photosensitivity, corneal scarring and developmental delay: Xeroderma Pigmentosum in a tropical country". Cases journal 1 (1): 254. doi:10.1186/1757-1626-1-254. PMC 2577106. PMID 18937855. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2577106.
External links
- Information
- GeneReviews/NCBI/NIH/UW entry on Xeroderma pigmentosum
- An article about this disorder from DigiLander.iol.it (in English and Italian)
- DermNet systemic/xeroderma-pigmentosum
- Charities
- XP Society
- XP Family Support Group
- UK Patient Support Group
- An article about an untreated XP patient with no access to modernized medical care, with photos.
-
-
- Halpern, J.; Hopping, B.; Brostoff, J. (2008). "Photosensitivity, corneal scarring and developmental delay: Xeroderma Pigmentosum in a tropical country". Cases journal 1 (1): 254. doi:10.1186/1757-1626-1-254. PMC 2577106. PMID 18937855. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2577106.
-
- Short films
- Sloan Science and Film / Short Films / XP by David Barba 10 minutes
- Web Site of a Short Film about an Xeroderma pigmentosum (XP) Patient. Film is directed by Kimberly Williams Paisley
Congenital malformations and deformations of integument / skin disease (Q80–Q82, 757.0–757.3) Genodermatosis Congenital ichthyosis/
erythrokeratodermiaADARUngroupedIchthyosis bullosa of Siemens · Ichthyosis follicularis · Ichthyosis prematurity syndrome · Ichthyosis–sclerosing cholangitis syndrome · Nonbullous congenital ichthyosiform erythroderma · Ichthyosis linearis circumflexa · Ichthyosis hystrixEB
and relatedJEB (JEB-H, Mitis, Generalized atrophic, JEB-PA)related: Costello syndrome · Kindler syndrome · Laryngoonychocutaneous syndrome · Skin fragility syndrome ·Naegeli syndrome/Dermatopathia pigmentosa reticularis · Hay–Wells syndrome · Hypohidrotic ectodermal dysplasia · Focal dermal hypoplasia · Ellis–van Creveld syndrome · Rapp–Hodgkin syndrome/Hay–Wells syndromeEhlers–Danlos syndrome · Cutis laxa (Gerodermia osteodysplastica) · Popliteal pterygium syndrome · Pseudoxanthoma elasticum · Van Der Woude syndromeHyperkeratosis/
keratinopathydiffuse: Diffuse epidermolytic palmoplantar keratoderma • Diffuse nonepidermolytic palmoplantar keratoderma • Palmoplantar keratoderma of Sybert • Mal de Meleda •syndromic (connexin (Bart–Pumphrey syndrome • Clouston's hidrotic ectodermal dysplasia • Vohwinkel syndrome) • Corneodermatoosseous syndrome • plakoglobin (Naxos syndrome) • Scleroatrophic syndrome of Huriez • Olmsted syndrome • Cathepsin C (Papillon–Lefèvre syndrome • Haim–Munk syndrome) • Camisa diseasefocal: Focal palmoplantar keratoderma with oral mucosal hyperkeratosis • Focal palmoplantar and gingival keratosis • Howel–Evans syndrome • Pachyonychia congenita (Pachyonychia congenita type I • Pachyonychia congenita type II) • Striate palmoplantar keratoderma • Tyrosinemia type II)punctate: Acrokeratoelastoidosis of Costa • Focal acral hyperkeratosis • Keratosis punctata palmaris et plantaris • Keratosis punctata of the palmar creases • Schöpf–Schulz–Passarge syndrome • Porokeratosis plantaris discreta • Spiny keratodermaungrouped: Palmoplantar keratoderma and spastic paraplegia • desmoplakin (Carvajal syndrome) • connexin (Erythrokeratodermia variabilis • HID/KID)OtherMeleda disease · Keratosis pilaris · ATP2A2 (Darier's disease) · Dyskeratosis congenita · Lelis syndromeDyskeratosis congenita · Keratolytic winter erythema · Keratosis follicularis spinulosa decalvans · Keratosis linearis with ichthyosis congenital and sclerosing keratoderma syndrome · Keratosis pilaris atrophicans faciei · Keratosis pilarisOthercadherin (EEM syndrome) · immune system (Hereditary lymphedema, Mastocytosis/Urticaria pigmentosa) · Hailey–Hailey
see also Template:Congenital malformations and deformations of skin appendages, Template:Phakomatoses, Template:Pigmentation disorders, Template:DNA replication and repair-deficiency disorderDevelopmental
anomaliesMidlineOther/ungroupedAplasia cutis congenita · Amniotic band syndrome · Branchial cyst · Cavernous venous malformation
Accessory nail of the fifth toe · Bronchogenic cyst · Congenital cartilaginous rest of the neck · Congenital hypertrophy of the lateral fold of the hallux · Congenital lip pit · Congenital malformations of the dermatoglyphs · Congenital preauricular fistula · Congenital smooth muscle hamartoma · Cystic lymphatic malformation · Median raphe cyst · Melanotic neuroectodermal tumor of infancy · Mongolian spot · Nasolacrimal duct cyst · Omphalomesenteric duct cyst · Poland anomaly · Rapidly involuting congenital hemangioma · Rosenthal–Kloepfer syndrome · Skin dimple · Superficial lymphatic malformation · Thyroglossal duct cyst · Verrucous vascular malformation · BirthmarkMetabolic disease: DNA replication and DNA repair-deficiency disorder DNA replication Separation/initiation: RNASEH2A (Aicardi–Goutières syndrome 4)
Termination/telomerase: DKC1 (Dyskeratosis congenita)DNA repair Cockayne syndrome/DeSanctis–Cacchione syndrome · Thymine dimer (Xeroderma pigmentosum) · IBIDS syndromeOtherRecQ helicase (Bloom syndrome, Werner syndrome, Rothmund–Thomson syndrome/Rapadilino syndrome) · Fanconi anemia · Li-Fraumeni syndrome · Severe combined immunodeficiencysee also DNA replication, DNA repair
B structural (perx, skel, cili, mito, nucl, sclr) · DNA/RNA/protein synthesis (drep, trfc, tscr, tltn) · membrane (icha, slcr, atpa, abct, othr) · transduction (iter, csrc, itra), trfkCategories:- Genodermatoses
- Hereditary cancers
- Autosomal recessive disorders
Wikimedia Foundation. 2010.