- Hereditary nonpolyposis colorectal cancer
-
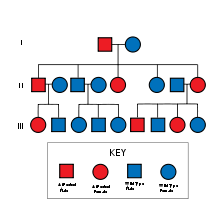
Hereditary nonpolyposis colorectal cancer Classification and external resources ICD-10 C18-C20 ICD-9 153.0-154.1 OMIM 120435 609310 114400 DiseasesDB 5812 MeSH D003123 Lynch syndrome (HNPCC or Hereditary nonpolyposis colorectal cancer ) is an autosomal dominant genetic condition which has a high risk of colon cancer[1] as well as other cancers including endometrium, ovary, stomach, small intestine, hepatobiliary tract, upper urinary tract, brain, and skin. The increased risk for these cancers is due to inherited mutations that impair DNA mismatch repair.
Contents
Terminology
Henry T. Lynch (professor of medicine at Creighton University Medical Center),[2] characterized the syndrome in 1966.[3] In his earlier work, he described the disease entity as "cancer family syndrome." The term "Lynch syndrome" was coined in 1984 by other authors, and Lynch himself coined the term HNPCC in 1985. Since then, the two terms have being used interchangeably, until more recent advances in the understanding of the genetics of the disease led to the term HNPCC falling out of favour.[4]
Other sources reserve the term "Lynch syndrome" when there is a known DNA mismatch repair defect, and use the term "Familial colorectal cancer type X" when the Amsterdam criteria are met but there is no known DNA mismatch repair defect.[5] The putative "type X" families appear to have a lower overall incidence of cancer and lower risk for non-colorectal cancers than families with documented DNA mismatch repair deficiency.[6] About 35% of patients meeting Amsterdam criteria do not have a DNA-mismatch-repair gene mutation.[7]
Complicating matters is the presence of an alternative set of criteria, known as the "Bethesda Guidelines".[8][9][10]
Classification
Three major groups of MSI-H (MSI, MicroSatellite Instability) cancers can be recognized by histopathological criteria:
- (1) right-sided poorly differentiated cancers
- (2) right-sided mucinous cancers
- (3) adenocarcinomas in any location showing any measurable level of intraepithelial lymphocyte (TIL)
Signs and symptoms
Risk of colon cancer
Individuals with HNPCC have about an 80% lifetime risk for colon cancer. Two-thirds of these cancers occur in the proximal colon. The mean age of colorectal cancer diagnosis is 44 for members of families that meet the Amsterdam criteria. Also, women with HNPCC have a 80% lifetime risk of endometrial cancer. The average age of diagnosis of endometrial cancer is about 46 years. Among women with HNPCC who have both colon and endometrial cancer, about half present first with endometrial cancer. In HNPCC, the mean age of diagnosis of gastric cancer is 56 years of age with intestinal-type adenocarcinoma being the most commonly reported pathology. HNPCC-associated ovarian cancers have an average age of diagnosis of 42.5 years-old; approximately 30% are diagnosed before age 40 years. Other HNPCC-related cancers have been reported with specific features: the urinary tract cancers are transitional carcinoma of the ureter and renal pelvis; small bowel cancers occur most commonly in the duodenum and jejunum; the central nervous system tumor most often seen is glioblastoma.
Genetics
HNPCC defects in DNA mismatch repair lead to microsatellite instability, also known as MSI-H, which is a hallmark of HNPCC. MSI is identifiable in cancer specimens in the pathology laboratory.[11] Most cases result in changes in the lengths of dinucleotide repeats of the nucleobases cytosine and adenine (sequence: CACACACACA...).[12]
HNPCC is known to be associated with mutations in genes involved in the DNA mismatch repair pathway
OMIM name Genes implicated in HNPCC Frequency of mutations in HNPCC families Locus First publication HNPCC1 (120435) MSH2 approximately 60% 2p22 Fishel et al., 1993[13] HNPCC2 (609310) MLH1 approximately 30% 3p21 Papadopoulos et al., 1994[14] HNPCC5 MSH6 7-10% 2p16 HNPCC4 PMS2 relatively infrequent,[15] <5%[citation needed] 7p22 HNPCC3 PMS1 case report[16] 2q31-q33 HNPCC6 TGFBR2 case report[17] 3p22 HNPCC7 MLH3 disputed[18] 14q24.3 Patients with MSH6 mutations are more likely to be Amsterdam criteria II-negative.[19] The presentation with MSH6 is slightly different than with MLH1 and MSH2, and the term "MSH6 syndrome" has been used to describe this condition.[20] In one study, the Bethesda guidelines were more sensitive than the Amsterdam Criteria in detecting it.[21]
Up to 39% of families with mutations in an HNPCC gene do not meet the Amsterdam criteria.[citation needed] Therefore, families found to have a deleterious mutation in an HNPCC gene should be considered to have HNPCC regardless of the extent of the family history. This also means that the Amsterdam criteria fail to identify many patients at risk for Lynch syndrome. Improving the criteria for screening is an active area of research, as detailed in the Screening Strategies section of this article.
HNPCC is inherited in an autosomal dominant manner. Most people with HNPCC inherit the condition from a parent. However, due to incomplete penetrance, variable age of cancer diagnosis, cancer risk reduction, or early death, not all patients with an HNPCC gene mutation have a parent who had cancer. Some patients develop HNPCC de-novo in a new generation, without inheriting the gene. These patients are often only identified after developing an early-life colon cancer. Parents with HNPCC have a 50% chance to pass the gene on to each child. However each person is different therefore there is no way to accurately tell who will develop the disorder.
Screening
Genetic testing for mutations in DNA mismatch repair genes is expensive and time-consuming, so researchers have proposed techniques for identifying cancer patients who are most likely to be HNPCC carriers as ideal candidates for genetic testing. The Amsterdam Criteria (see below) are useful, but do not identify up to 30% of potential Lynch syndrome carriers[citation needed]. In colon cancer patients, pathologists can measure microsatellite instability in colon tumor specimens, which is a surrogate marker for DNA mismatch repair gene dysfunction. If there is microsatellite instability identified, there is a higher likelihood for a Lynch syndrome diagnosis. Recently, researchers combined microsatellite instability (MSI) profiling and immunohistochemistry testing for DNA mismatch repair gene expression and identified an extra 32% of Lynch syndrome carriers who would have been missed on MSI profiling alone.[citation needed] Currently, this combined immunohistochemistry and MSI profiling strategy is the most advanced way of identifying candidates for genetic testing for the Lynch syndrome.
Genetic counseling and genetic testing are recommended for families that meet the Amsterdam criteria, preferably before the onset of colon cancer.
Amsterdam criteria
The following are the Amsterdam criteria in identifying high-risk candidates for molecular genetic testing:[22]
Amsterdam Criteria:
- Three or more family members with a confirmed diagnosis of colorectal cancer, one of whom is a first degree (parent, child, sibling) relative of the other two
- Two successive affected generations
- One or more colon cancers diagnosed under age 50 years
- Familial adenomatous polyposis (FAP) has been excluded
Amsterdam Criteria II:
- Three or more family members with HNPCC-related cancers, one of whom is a first degree relative of the other two
- Two successive affected generations
- One or more of the HNPCC-related cancers diagnosed under age 50 years
- Familial adenomatous polyposis (FAP) has been excluded
Diagnosis
The Amsterdam clinical criteria identifies candidates for genetic testing, and genetic testing can make a diagnosis of Lynch syndrome. Genetic testing is commercially available and consists of a blood test.
Management
Surgery remains the front-line therapists for HNPCC. There is an ongoing controversy over the benefit of 5-fluorouracil-based adjuvant therapies for HNPCC-related colorectal tumours, particularly those in stages I and II.[23]
After reporting a null finding from their randomized controlled trial of aspirin (ASA) to prevent against the colorectal neoplasia of Lynch Syndrome,[24] Burn and colleagues have recently reported new data, representing a longer follow-up period than reported in the initial NEJM paper. These new data demonstrate a reduced incidence in Lynch Syndrome patients who were exposed to at least four years of high-dose aspirin, with a satisfactory risk profile.[25] These results have been widely covered in the media; future studies will look at modifying (lowering) the dose (to reduce risk associated with the high dosage of ASA. Individuals with Lynch Syndrome may wish to discuss the application of these results with their medical care team.
Epidemiology
In the United States, about 160,000 new cases of colorectal cancer are diagnosed each year. Hereditary nonpolyposis colorectal cancer is responsible for approximately 2 percent to 7 percent of all diagnosed cases of colorectal cancer. The average age of diagnosis of cancer in patients with this syndrome is 44 years old, as compared to 64 years old in people without the syndrome.[26]
References
- ^ Kastrinos F, Mukherjee B, Tayob N, et al. (October 2009). "Risk of pancreatic cancer in families with Lynch syndrome". JAMA 302 (16): 1790–5. doi:10.1001/jama.2009.1529. PMID 19861671.
- ^ School of Medicine :: Hereditary Cancer Center :: Creighton University
- ^ Lynch HT, Shaw MW, Magnuson CW, Larsen AL, Krush AJ (February 1966). "Hereditary factors in cancer. Study of two large midwestern kindreds". Arch. Intern. Med. 117 (2): 206–12. doi:10.1001/archinte.117.2.206. PMID 5901552. http://archinte.ama-assn.org/cgi/pmidlookup?view=long&pmid=5901552.
- ^ Bellizzi AM, Frankel WL (2009). "Colorectal cancer due to deficiency in DNA mismatch repair function: a review". Advances in Anatomic Pathology 16 (6): 405–417. doi:10.1097/PAP.0b013e3181bb6bdc. PMID 19851131.
- ^ Lindor NM (October 2009). "Familial colorectal cancer type X: the other half of hereditary nonpolyposis colon cancer syndrome". Surg. Oncol. Clin. N. Am. 18 (4): 637–45. doi:10.1016/j.soc.2009.07.003. PMID 19793571. http://journals.elsevierhealth.com/retrieve/pii/S1055-3207(09)00061-1.
- ^ Lindor NM, Rabe K, Petersen GM, et al. (April 2005). "Lower cancer incidence in Amsterdam-I criteria families without mismatch repair deficiency: familial colorectal cancer type X". JAMA 293 (16): 1979–85. doi:10.1001/jama.293.16.1979. PMC 2933042. PMID 15855431. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=15855431.
- ^ Scott RJ, McPhillips M, Meldrum CJ, et al. (January 2001). "Hereditary nonpolyposis colorectal cancer in 95 families: differences and similarities between mutation-positive and mutation-negative kindreds". Am. J. Hum. Genet. 68 (1): 118–127. doi:10.1086/316942. PMC 1234904. PMID 11112663. http://linkinghub.elsevier.com/retrieve/pii/S0002-9297(07)62476-8.
- ^ Gologan A, Krasinskas A, Hunt J, Thull DL, Farkas L, Sepulveda AR (November 2005). "Performance of the revised Bethesda guidelines for identification of colorectal carcinomas with a high level of microsatellite instability". Arch. Pathol. Lab. Med. 129 (11): 1390–7. doi:10.1043/1543-2165(2005)129[1390:POTRBG]2.0.CO;2. PMID 16253017. http://journals.allenpress.com/jrnlserv/?request=get-abstract&issn=0003-9985&volume=129&page=1390.
- ^ Umar A, Boland CR, Terdiman JP, et al. (February 2004). "Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability". J. Natl. Cancer Inst. 96 (4): 261–8. doi:10.1093/jnci/djh034. PMC 2933058. PMID 14970275. http://jnci.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=14970275.
- ^ Lipton LR, Johnson V, Cummings C, et al. (December 2004). "Refining the Amsterdam Criteria and Bethesda Guidelines: testing algorithms for the prediction of mismatch repair mutation status in the familial cancer clinic". J. Clin. Oncol. 22 (24): 4934–43. doi:10.1200/JCO.2004.11.084. PMID 15611508. http://www.jco.org/cgi/pmidlookup?view=long&pmid=15611508.
- ^ Pathology of Hereditary Nonpolyposis Colorectal Cancer - JASS 910 (1): 62 - Annals of the New York Academy of Sciences
- ^ Oki, E.; Oda, S.; Maehara, Y.; Sugimachi, K. (1999). "Mutated gene-specific phenotypes of dinucleotide repeat instability in human colorectal carcinoma cell lines deficient in DNA mismatch repair". Oncogene 18 (12): 2143–2147. doi:10.1038/sj.onc.1202583. PMID 10321739.
- ^ Fishel R, Lescoe M, Rao M, Copeland N, Jenkins N, Garber J, Kane M, Kolodner R (1993). "The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer". Cell 75 (5): 1027–38. doi:10.1016/0092-8674(93)90546-3. PMID 8252616.
- ^ Papadopoulos N, Nicolaides N, Wei Y, Ruben S, Carter K, Rosen C, Haseltine W, Fleischmann R, Fraser C, Adams M (1994). "Mutation of a mutL homolog in hereditary colon cancer". Science 263 (5153): 1625–9. doi:10.1126/science.8128251. PMID 8128251.
- ^ Thompson E, Meldrum CJ, Crooks R, et al. (March 2004). "Hereditary non-polyposis colorectal cancer and the role of hPMS2 and hEXO1 mutations". Clin. Genet. 65 (3): 215–25. doi:10.1111/j.1399-0004.2004.00214.x. PMID 14756672. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0009-9163&date=2004&volume=65&issue=3&spage=215.
- ^ Nicolaides NC, Papadopoulos N, Liu B, et al. (September 1994). "Mutations of two PMS homologues in hereditary nonpolyposis colon cancer". Nature 371 (6492): 75–80. doi:10.1038/371075a0. PMID 8072530.
- ^ Lu SL, Kawabata M, Imamura T, et al. (May 1998). "HNPCC associated with germline mutation in the TGF-beta type II receptor gene". Nat. Genet. 19 (1): 17–8. doi:10.1038/ng0598-17. PMID 9590282.
- ^ Ou J, Rasmussen M, Westers H, et al. (April 2009). "Biochemical characterization of MLH3 missense mutations does not reveal an apparent role of MLH3 in Lynch syndrome". Genes Chromosomes Cancer 48 (4): 340–50. doi:10.1002/gcc.20644. PMID 19156873.
- ^ Ramsoekh D, Wagner A, van Leerdam ME, et al. (November 2008). "A high incidence of MSH6 mutations in Amsterdam criteria II-negative families tested in a diagnostic setting". Gut 57 (11): 1539–44. doi:10.1136/gut.2008.156695. PMID 18625694. http://gut.bmj.com/cgi/pmidlookup?view=long&pmid=18625694.
- ^ Suchy J, Lubinski J (2008). "MSH6 syndrome". Hered Cancer Clin Pract 6 (2): 103–104. doi:10.1186/1897-4287-6-2-103. PMC 2735474. PMID 19804606. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2735474.
- ^ Goldberg Y, Porat RM, Kedar I, et al. (October 2009). "An Ashkenazi founder mutation in the MSH6 gene leading to HNPCC". Fam. Cancer 9 (2): 141–50. doi:10.1007/s10689-009-9298-9. ISBN 1068900992989. PMID 19851887.
- ^ Vasen HF, Watson P, Mecklin JP, Lynch HT (June 1999). "New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC". Gastroenterology 116 (6): 1453–6. PMID 10348829.
- ^ Boland CR, Koi M, Chang DK, Carethers JM. The biochemical basis of microsatellite instability and abnormal immunohistochemistry and clinical behavior in Lynch Syndrome: from bench to bedside. Familial Cancer epub 2007; DOI 10.1007/s10689-007-9145-9
- ^ Burn J, Bishop DT, Mecklin JP, et al. (December 2008). "Effect of aspirin or resistant starch on colorectal neoplasia in the Lynch syndrome". N. Engl. J. Med. 359 (24): 2567–78. doi:10.1056/NEJMoa0801297. PMID 19073976. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=19073976&promo=ONFLNS19.
- ^ "Aspirin Confers Long-Term Protective Effect in Lynch Syndrome Patients". http://www.medscape.com/viewarticle/711603. Retrieved 2009-11-07.
- ^ Cancer Information, Research, and Treatment for all Types of Cancer | OncoLink
External links
- FAQs on HNPCC from the National Institute of Health
- GeneReviews/NCBI/NIH/UW entry on Lynch syndrome
- hnpcc at NIH/UW GeneTests
- National Cancer Institute: Genetics of Colorectal Cancer information summary
Tumors: digestive system neoplasia (C15–C26/D12–D13, 150–159/211) GI tract Upper GI tractGastric carcinoma · Signet ring cell carcinoma · Gastric lymphoma (MALT lymphoma) · Linitis plasticacolorectal polyp: Peutz-Jeghers syndrome · Juvenile polyposis syndrome · Familial adenomatous polyposis/Gardner's syndrome · Cronkhite–Canada syndromeneoplasm: Adenocarcinoma · Familial adenomatous polyposis · Hereditary nonpolyposis colorectal cancerUpper and/or lowerAccessory exocrine pancreas: Adenocarcinoma · Pancreatic ductal carcinoma
cystic neoplasms: Serous microcystic adenoma · Intraductal papillary mucinous neoplasm · Mucinous cystic neoplasm · Solid pseudopapillary neoplasm
PancreatoblastomaPeritoneum Metabolic disease: DNA replication and DNA repair-deficiency disorder DNA replication Separation/initiation: RNASEH2A (Aicardi–Goutières syndrome 4)
Termination/telomerase: DKC1 (Dyskeratosis congenita)DNA repair Cockayne syndrome/DeSanctis–Cacchione syndrome · Thymine dimer (Xeroderma pigmentosum) · IBIDS syndromeOtherRecQ helicase (Bloom syndrome, Werner syndrome, Rothmund–Thomson syndrome/Rapadilino syndrome) · Fanconi anemia · Li-Fraumeni syndrome · Severe combined immunodeficiencysee also DNA replication, DNA repair
B structural (perx, skel, cili, mito, nucl, sclr) · DNA/RNA/protein synthesis (drep, trfc, tscr, tltn) · membrane (icha, slcr, atpa, abct, othr) · transduction (iter, csrc, itra), trfkCategories:- Gastrointestinal cancer
- Hereditary cancers
Wikimedia Foundation. 2010.