- Aortic aneurysm
-
Aortic aneurysm Classification and external resources 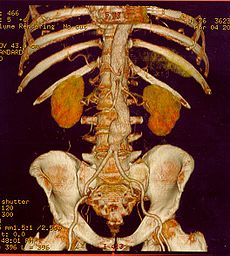
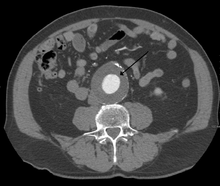
CT reconstruction image of an abdominal aortic aneurysmICD-10 I71 ICD-9 441 OMIM 100070 DiseasesDB 792 eMedicine emerg/942 med/2783 emerg/27 radio/1 med/3443 MeSH D001014 An aortic aneurysm is a general term for any swelling (dilation or aneurysm) of the aorta to greater than 1.5 times normal, usually representing an underlying weakness in the wall of the aorta at that location. While the stretched vessel may occasionally cause discomfort, a greater concern is the risk of rupture, which causes severe pain; massive internal hemorrhage; and, without prompt treatment, death occurs rapidly.
Contents
Classification
Aortic aneurysms are classified by where on the aorta they occur; aneurysms can appear anywhere.
- An aortic root aneurysm, or aneurysm of sinus of Valsalva, appears on the sinuses of Valsalva or aortic root.
- Thoracic aortic aneurysms are found on the thoracic aorta; these are further classified as ascending, aortic arch, or descending aneurysms depending on the location on the thoracic aorta involved.
- Abdominal aortic aneurysms, the most common form of aortic aneurysm, are found on the abdominal aorta, and thoracoabdominal aortic aneurysms involve both the thoracic and abdominal aorta. There are other classifications that might help treatment.
Signs and symptoms
Most intact aortic aneurysms do not produce symptoms. As they enlarge, symptoms such as abdominal pain and back pain may develop. Compression of nerve roots may cause leg pain or numbness. Untreated, aneurysms tend to become progressively larger, although the rate of enlargement is unpredictable for any individual. Rarely, clotted blood which lines most aortic aneurysms can break off and result in an embolus. They may be found on physical examination. Medical imaging is necessary to confirm the diagnosis. Signs may include: anxiety or feeling of stress; nausea and vomiting; clammy skin; rapid heart rate.[1]
In patients presenting with aneurysm of the arch of the aorta, a common sign is a hoarse voice as the left recurrent laryngeal nerve (a branch of the vagus nerve) is stretched. This is due to the recurrent laryngeal nerve winding around the arch of the aorta.
Abdominal aortic aneurysm
Abdominal aortic aneurysms (AAAs) are the most common type of aortic aneurysm. One reason for this is that elastin, the principal load-bearing protein present in the wall of the aorta, is reduced in the abdominal aorta as compared to the thoracic aorta (nearer the heart). Another is that the abdominal aorta does not possess vasa vasorum, hindering repair. Most are true aneurysms that involve all three layers (tunica intima, tunica media and tunica adventitia), and are generally asymptomatic before rupture.
An AAA may remain asymptomatic indefinitely. There is a large risk of rupture once the size has reached 5 cm, though some AAAs may swell to over 15 cm in diameter before rupturing. Before rupture, an AAA may present as a large, pulsatile mass above the umbilicus. A bruit may be heard from the turbulent flow in a severe atherosclerotic aneurysm or if thrombosis occurs. Unfortunately, however, rupture is usually the first hint of AAA. Once an aneurysm has ruptured, it presents with a classic pain-hypotension-mass triad. The pain is classically reported in the abdomen, back or flank. It is usually acute, severe and constant, and may radiate through the abdomen to the back.
The diagnosis of an abdominal aortic aneurysm can be confirmed at the bedside by the use of ultrasound. Rupture could be indicated by the presence of free fluid in potential abdominal spaces, such as Morison's pouch, the splenorenal space (between the spleen and left kidney), subdiaphragmatic spaces(underneath the diaphragm) and peri-vesical spaces. A contrast-enhanced abdominal CT scan is needed for confirmation.
Only 10–25% of patients survive rupture due to large pre- and post-operative mortality. Annual mortality from ruptured aneurysms in the United States is about 15,000. Most are due to abdominal aneurysms, with thoracic and thoracoabdominal aneurysms making up 1% to 4% of the total. Another important complication of AAA is formation of a thrombus in the aneurysm. The prevalence of AAAs increases with age, with an average age of 65–70 at the time of diagnosis. AAAs have been attributed to atherosclerosis, though other factors are involved in their formation.
Risk factors
- CAD
- Hypertension
- Hypercholesterolemia
- Hyperhomocysteinemia
- Elevated C-reactive protein
- Tobacco use
- Peripheral vascular disease
- Marfan syndrome
- Ehlers-Danlos type IV
Pathophysiology
The physical change in the aortic diameter can occur secondary to trauma, infection, an intrinsic defect in the protein construction of the aortic wall, or due to progressive destruction of aortic proteins by enzymes.
Screening
Treatment
Surgery is the definite treatment of aortic aneurysm, while medical therapy is typically supportive.
Surgery
The definitive treatment for an aortic aneurysm may be surgical or endovascular repair. The determination of surgical intervention is complex and determined on a per-case basis. Risk of aneurysm rupture is weighed against procedural risk. The diameter of the aneurysm, its rate of growth, the presence or absence of Marfan Syndrome, Vascular Ehlers-Danlos or similar connective tissue disorders, and other co-morbidities are all important factors in the overall treatment.
A rapidly expanding aneurysm should under normal circumstances be operated on as soon as feasible, since it has a greater chance of rupture. Slowly expanding aortic aneurysms may be followed by routine diagnostic testing (i.e.: CT scan or ultrasound imaging).
For abdominal aneurysms, the current treatment guidelines for abdominal aortic aneurysms suggest elective surgical repair when the diameter of the aneurysm is greater than 5 cm. However, recent data suggest medical management for abdominal aneurysms with a diameter of less than 5.5 cm.[2]
Open
Open surgery typically involves dissection of the dilated portion of the aorta and insertion of a synthetic (Dacron or Gore-Tex) patch tube. Once the tube is sewn into the proximal and distal portions of the aorta, the aneurysmal sac is closed around the artificial tube. Instead of sewing, the tube ends, made rigid and expandable by nitinol wireframe, can be much more simply, quickly and effectively ("airtight" seal) inserted into the vascular stumps and there permanently fixed by external ligature (video) [1][3][4][5]
The aorta and possibly also its branching arteries are cross-clamped during open surgery. This can lead to inadequate blood supply to the spinal cord, resulting in neurological deficits. Cerebrospinal fluid drainage (CSFD), when performed in experienced centers, reduce this risk of ischaemic spinal cord injury, as evidenced by randomized trials,[6] by increasing the perfusion pressure to the spinal cord.[7]
Endovascular
- AAA
In the recent years, the endoluminal treatment of abdominal aortic aneurysms has emerged as a minimally invasive alternative to open surgery repair. The first endoluminal exclusion of an aneurysm took place in Argentina by Dr. Parodi and his colleagues in 1991. The endovascular treatment of aortic aneurysms involves the placement of an endo-vascular stent via a percutaneous technique (usually through the femoral arteries) into the diseased portion of the aorta. This technique has been reported to have a lower mortality rate compared to open surgical repair, and is now being widely used in individuals with co-morbid conditions that make them high risk patients for open surgery. Some centers also report very promising results for the specific method in patients that do not constitute a high surgical risk group.
There have also been many reports concerning the endovascular treatment of ruptured Abdominal Aortic Aneurysms, which are usually treated with an open surgery repair due to the patient's impaired overall condition. Mid-term results have been quite promising.[citation needed] However, due to the time frame of the emerging, the long term benefit of the EVAR procedure against open surgery has not yet been identified.[8]
In spite aneurysms have been treated by endovascular techniques in virtually all aortic segments, better than open aortic repair results were statistically documented only in uncomplicated, elective descending thoracic and infrarenal aorta. Moreover recent USA Nationwide Inpatient Sample data 2006–2007 review of isolated descending thoracic aorta aneurysm cases[9] showed that only 23% (2,563/11,669) of ideal candidate (uncomplicated, elective descending aortic aneurysms) underwent to TEVAR, the remaining 77% (9,106/11,669) still underwent open surgical repair. Although results were better with TEVAR than with OAR it is clear that still the vast majority of thoracic aortic aneurisms is treated by standard open repair
- Other
The endoluminal exclusion of aortic aneurysms has seen a real revolution in the very recent years. It is now possible to treat thoracic aortic aneurysms, abdominal aortic aneurysms and other aneurysms in most of the body's major arteries (such as the iliac and the femoral arteries) using endovascular stents and avoiding big incisions. Still, in most cases the technique is applied in patients at high risk for surgery as more trials are required in order to fully accept this method as the gold standard for the treatment of aneurysms.
Medical therapy
Medical therapy of aortic aneurysms involves strict blood pressure control. This does not treat the aortic aneurysm per se, but control of hypertension within tight blood pressure parameters may decrease the rate of expansion of the aneurysm.
Prevention
Attention to patient's general blood pressure, smoking and cholesterol risks helps reduce the risk on an individual basis. There have been proposals to introduce ultrasound scans as a screening tool for those most at risk: men over the age of 65.[10][11] The tetracycline antibiotic Doxycycline is currently being investigated for use as a potential drug in the prevention of aortic aneurysm due to its metalloproteinase inhibitor and collagen stabilising properties.
See also
References
- ^ "Rush University Medical Center". http://www.rush.edu/rumc/page-1160429744171.html. Retrieved 2008-03-12.
- ^ "Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. The UK Small Aneurysm Trial Participants". Lancet 352 (9141): 1649–55. November 1998. doi:10.1016/S0140-6736(98)10137-X. PMID 9853436. http://linkinghub.elsevier.com/retrieve/pii/S014067369810137X.
- ^ Aluffi A, Berti A, Buniva P, Rescigno G, Nazari S (2002). "Improved device for sutureless aortic anastomosis applied in a case of cancer". Tex Heart Inst J. 29 (1): 56–9. PMC 101273. PMID 11995854. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=101273.
- ^ Nazari S, Salvi S, Visconti E, et al. (June 1999). "Descending aorta substitution with expandable ends prosthesis. Case report". J Cardiovasc Surg (Torino) 40 (3): 417–20. PMID 10412932.
- ^ Nazari S (February 2010). "Expandable device type III for easy and reliable approximation of dissection layers in sutureless aortic anastomosis. Ex vivo experimental study". Interact Cardiovasc Thorac Surg 10 (2): 161–4. doi:10.1510/icvts.2009.216291. PMID 19933306. http://icvts.ctsnetjournals.org/cgi/pmidlookup?view=long&pmid=19933306.
- ^ Cinà, C.; Abouzahr, L.; Arena, G.; Laganà, A.; Devereaux, P.; Farrokhyar, F. (2004). "Cerebrospinal fluid drainage to prevent paraplegia during thoracic and thoracoabdominal aortic aneurysm surgery: a systematic review and meta-analysis". Journal of vascular surgery : official publication, the Society for Vascular Surgery [and] International Society for Cardiovascular Surgery, North American Chapter 40 (1): 36–44. doi:10.1016/j.jvs.2004.03.017. PMID 15218460.
- ^ Khan, S. N.; Stansby, G. (2004). "Cerebrospinal fluid drainage for thoracic and thoracoabdominal aortic aneurysm surgery". Cochrane Database of Systematic Reviews (1): CD003635. doi:10.1002/14651858.CD003635.pub2. PMID 14974026.
- ^ Rutherford RB (June 2006). "Randomized EVAR trials and advent of level i evidence: a paradigm shift in management of large abdominal aortic aneurysms?". Semin Vasc Surg. 19 (2): 69–74. doi:10.1053/j.semvascsurg.2006.03.001. PMID 16782510.
- ^ Gopaldas RR, Huh J, Dao TK, et al. (November 2010). "Superior nationwide outcomes of endovascular versus open repair for isolated descending thoracic aortic aneurysm in 11,669 patients". J. Thorac. Cardiovasc. Surg. 140 (5): 1001–10. doi:10.1016/j.jtcvs.2010.08.007. PMID 20951252. http://linkinghub.elsevier.com/retrieve/pii/S0022-5223(10)00883-4.
- ^ Routine screening in the management of AAA, UK Department of Health study Report
- ^ "Abdominal Aortic Aneurysm". Bandolier 27 (3). May 1996. http://www.medicine.ox.ac.uk/bandolier/band27/b27-3.html.
Bibliography
- Saratzis N, Melas N, Lazaridis J, et al. (June 2005). "Endovascular AAA repair with the aortomonoiliac EndoFit stent-graft: two years' experience". J Endovasc Ther. 12 (3): 280–7. doi:10.1583/04-1474.1. PMID 15943502.
External links
- Vascular Medicine — Information for experts and laypersons regarding vascular medicine and related diseases.
- Aortic Aneurysm CT scans MedPix Medical Images
Cardiovascular disease: vascular disease · Circulatory system pathology (I70–I99, 440–456) Arteries, arterioles
and capillariesAtherosclerosis (Foam cell, Fatty streak, Atheroma, Intermittent claudication) · Monckeberg's arteriosclerosis · Arteriolosclerosis (Hyaline, Hyperplastic, oxycholesterol, cholesterol, LDL, trans fat)Othertorso: Aortic aneurysm (Thoracic aortic aneurysm, Abdominal aortic aneurysm) · Aortic dissection · Coronary artery aneurysmhead/neck: Cerebral aneurysm · Intracranial berry aneurysm · Carotid artery dissection · Vertebral artery dissection · Familial aortic dissectionVeins OtherArteries or veins Blood pressure Hypertensive heart disease · Hypertensive nephropathy · Essential hypertension · Secondary hypertension (Renovascular hypertension) · Pulmonary hypertension · Malignant hypertension · Benign hypertension · Systolic hypertension · White coat hypertensionCategories:- Diseases of the aorta
- Vascular surgery
- Diseases of arteries, arterioles and capillaries
- Deaths from aortic aneurysm
Wikimedia Foundation. 2010.