- Chronic venous insufficiency
-
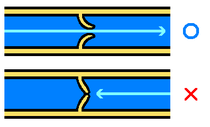
Chronic venous insufficiency Classification and external resources ICD-10 I87.2 ICD-9 459.81 DiseasesDB 13734 eMedicine article/461449 MeSH D014689 Chronic venous insufficiency or CVI is a medical condition where the veins cannot pump enough oxygen-poor blood back to the heart.[1] It is sometimes referred to as an "impaired musculovenous pump", this is due to damaged or "incompetent" valves as may occur after deep vein thrombosis (when the disease is called postthrombotic syndrome) or phlebitis. Paratroopers, utility pole linemen, and men with leg injuries can suffer from damaged leg vein valves and develop this condition. Ordinarily, women make up the largest demographic for this problem.
Contents
Venous insufficiency in the legs
As functional venous valves are required to provide for efficient blood return from the lower extremities, CVI often occurs in the veins of the legs. Itching (pruritis) is sometimes a symptom, along with hyperpigmentation of the legs. Symptoms of CVI include phlebetic lymphedema and chronic swelling of the legs and ankles. The skin may react with varicose eczema, local inflammation, discoloration, thickening, and an increased risk of ulcers and cellulitis. The condition has been known since ancient times and Hippocrates used bandaging to treat it. It is better described as chronic peripheral venous insufficiency.
Venous valve incompetence is treated conservatively with manual compression lymphatic massage therapy, skin lubrication, sequential compression pump, ankle pump, compression stockings, blood pressure medicine, frequent periods of rest elevating the legs above the heart level and using a 20 cm (7-inch) bed wedge during sleep. Surgical treatments include the old Linton procedures and the newer subfascial endoscopic perforator vein surgery. Some experimental valve repair or valve transposition procedures as well as some hemodynamic surgeries are being pursued. This whole field of medicine while ancient is still filled with complications e.g. Sometimes an artery can strangulate a vein or sometimes an arteriovenous fistula (an abnormal connection or passageway between an artery and a vein) may be causing the apparent poor venous return.
Patients are often encouraged to walk while wearing the prescribed medical stockings and to sleep in a 6 degree Trendelenburg position.[citation needed] Obese or pregnant patients might be advised by their physicians to forgo the tilted bed.
Surprisingly, leech therapy long ago abandoned by medicine, can actually be beneficial treatment.[citation needed] The leeches draw out the excess venous blood that has CO2 and metabolic wastes in a measured amount with little danger of dropping the blood volume.[citation needed]
May-Thurner syndrome
In medicine, May-Thurner syndrome is a rare condition in which blood clots, called deep venous thrombosis (DVT), occur in the iliofemoral vein due to compression of the blood vessels in the leg. The specific problem is compression of the left common iliac vein by the overlying right common iliac artery.[citation needed] This leads to pooling or stasis of blood, predisposing the individual to the formation of blood clots.
Venous insufficiency in the central nervous system
CVI has been reported in the CNS of several persons.[2] When it appears into the CNS is called Chronic cerebrospinal venous insufficiency (CCSVI). It can be seen using Transcranial doppler sonography or MRV (magnetic resonance venography)
This disease was only recently described (2006) and the first international symposium took place on September 8, 2009 in Bologna, Italy. The causes of venous insufficiencies were discussed, and it was mostly shown that it is due to venous stenosis which is subsequently due to genetics or embryonic problems.[3]
The known consequences of the disease are hypoxia, delayed perfusion and iron deposits in the blood vessels, with unknown final effects for the health of the patients. A connection with MS has been proposed (all cases of CCSVI were found in MS patients[2]) but the possible relationship is still under study.
It can be treated currently in two ways: Balloons to open the veins, in the hope they will remain open, and venous stents, to keep them open permanently.
Other research groups have found jugular veins reflux in other neurological diseases. In particular in Transient Global Amnesia,[4][5] Leukoaraiosis,[6] and general myelopathies.[7] All of them have been linked to venous reflux with different names like Cerebral Venous Outflow Impairment. At this moment is unknown if these conditions can be considered related to CCSVI.
Venous insufficiency in the liver
Budd–Chiari syndrome is the condition caused by occlusion of the hepatic veins. It presents with the classical triad of abdominal pain, ascites and hepatomegaly. Examples of occlusion include thrombosis of hepatic veins. The syndrome can be fulminant, acute, chronic, or asymptomatic. It occurs in 1 out of a million individuals[8] and is more common in females. Some 10–20% also have obstruction of the portal vein.
Any obstruction of the venous vasculature of the liver is referred to as Budd-Chiari syndrome, from the venules to the right atrium. This leads to increased portal vein and hepatic sinusoid pressures as the blood flow stagnates. The increased portal pressure causes: 1) increased filtration of vascular fluid with the formation of protein-rich ascites in the abdomen; and 2) collateral venous flow through alternative veins leading to gastric varices and hemorrhoids. Obstruction also causes centrilobular necrosis and peripheral lobule fatty change due to ischemia. If this condition persists chronically what is known as Nutmeg liver will develop. Renal failure may occur, perhaps due to the body sensing an "underfill" state and subsequent activation of the renin-angiotensin pathways and excess sodium retention.
See also
- Atrophie blanche
- Chronic cerebrospinal venous insufficiency
- Compression stockings
- Heavy legs
- Linton flap
- Lipodermatosclerosis
- May-Thurner syndrome
- Musculovenous pump
- Thoracic outlet syndrome
- Varicose veins
- Vascular myelopathy
- Venography
- Venous stasis ulceration
- Venous stasis
- Venous ulcer
- Superior vena cava syndrome
- Chronic venous congestion
References
- ^ "Chronic Venous Insufficiency". Society for Vascular Surgery. December 1, 2009. http://www.vascularweb.org/vascularhealth/Pages/chronic-venous-insufficiency.aspx.
- ^ a b Zamboni, P; Galeotti, R; Menegatti, E; Malagoni, A M; Tacconi, G; Dall'ara, S; Bartolomei, I; Salvi, F (2008). "Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis". Journal of Neurology, Neurosurgery & Psychiatry 80 (4): 392–9. doi:10.1136/jnnp.2008.157164. PMC 2647682. PMID 19060024. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2647682.
- ^ Bologna conference notes [1][unreliable medical source?]
- ^ Chung, C; Hsu, H; Chao, A; Sheng, W; Soong, B; Hu, H (2007). "Transient Global Amnesia: Cerebral Venous Outflow Impairment—Insight from the Abnormal Flow Patterns of the Internal Jugular Vein". Ultrasound in Medicine & Biology 33 (11): 1727–35. doi:10.1016/j.ultrasmedbio.2007.05.018.
- ^ Chung, C; Hsu, H; Chao, A; Wong, W; Sheng, W; Hu, H (2007). "Flow Volume in the Jugular Vein and Related Hemodynamics in the Branches of the Jugular Vein". Ultrasound in Medicine & Biology 33 (4): 500–5. doi:10.1016/j.ultrasmedbio.2006.10.009.
- ^ Chung, Chih-Ping; Hu, Han-Hwa (2010). "Pathogenesis of leukoaraiosis: Role of jugular venous reflux". Medical Hypotheses 75 (1): 85–90. doi:10.1016/j.mehy.2010.01.042. PMID 20172657.
- ^ Leriche, H; Aubin, ML; Aboulker, J (1976). "Cavo-spinal phlebography in myelopathies. Stenoses of internal jugular and azygos veins, venous compressions and thromboses". Acta radiologica. Supplementum 347: 415–7. PMID 207127.
- ^ Rajani, Rupesh; Melin, Tor; Björnsson, Einar; Broomé, Ulrika; Sangfelt, Per; Danielsson, Åke; Gustavsson, Anders; Grip, Olof et al. (2009). "Budd-Chiari syndrome in Sweden: epidemiology, clinical characteristics and survival – an 18-year experience". Liver International 29 (2): 253–9. doi:10.1111/j.1478-3231.2008.01838.x. PMID 18694401.
Further reading
- Anning, Stephen Towers (1954). Leg ulcers: their causes and treatment. London: Churchill. OCLC 14661804.
- Scott, HJ; McMullin, GM; Coleridge Smith, PD; Scurr, JH (1990). "Venous disease: investigation and treatment, fact or fiction?". Annals of the Royal College of Surgeons of England 72 (3): 188–92. PMC 2499160. PMID 2192676. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2499160.
Categories:- Vascular diseases
Wikimedia Foundation. 2010.