- Superior vena cava syndrome
-
Superior vena cava syndrome Classification and external resources
Superior vena cava syndrome in a person with bronchogenic carcinoma. Note the swelling of his face first thing in the morning (left) and its resolution after being upright all day (right).ICD-10 I87.1 ICD-9 459.2 DiseasesDB 12711 MedlinePlus 001097 eMedicine emerg/561 MeSH D013479 Superior vena cava syndrome (SVCS), or superior vena cava obstruction (SVCO), is usually the result of the direct obstruction of the superior vena cava by malignancies such as compression of the vessel wall by right upper lobe tumors or thymoma and/or mediastinal lymphadenopathy. The most common malignancies that cause SVCS is bronchogenic carcinoma. Cerebral edema is rare, but if it occurs it may be fatal. [1][2]
Contents
Signs and symptoms
Shortness of breath is the most common symptom, followed by face or arm swelling.[3]
Following are frequent symptoms:
- Dyspnea[1]
- Headache[1]
- Facial edema[1]
- Venous distention in the neck and distended veins in the upper chest and arms[1]
- Upper limb edema[1]
- Lightheadedness[3]
- Cough[3]
- Edema of the neck, called the collar of Stokes[4]
Superior vena cava syndrome usually presents more gradually with an increase in symptoms over time as malignancies increase in size or invasiveness.[3]
Cause
Approximately 90% of cases are associated with a cancerous tumor that is compressing the superior vena cava,[3] such as bronchogenic carcinoma including small cell and non-small cell lung carcinoma, Burkitt lymphoma, lymphoblastic lymphomas, pre-T-cell lineage acute lymphoblastic leukemia (rare), and other acute leukemias.[3] Syphilis and tuberculosis have also been known to cause superior vena cava syndrome.[3] SVCS can be caused by invasion or compression by a pathological process or by thrombosis in the vein itself, although this latter is less common (approximately 35% due to the use of intravascular devices).[3]
Diagnosis
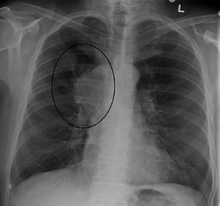
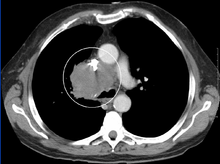
The main techniques of diagnosing SVCS are with chest X-rays (CXR), CT scans, transbronchial needle aspiration at bronchoscopy and mediastinoscopy.[1] CXRs provide the ability to show mediastinal widening and may show the presenting primary cause of SVCS.[1] CT scans should be contrast enhanced and be taken on the neck, chest, lower abdomen and pelvis.[1] They may also show the underlying cause and the extent to which the disease has progressed.[1]
Treatment
Several methods of treatment are available, mainly consisting of careful drug therapy and surgery.[3] Glucocorticoids (such as prednisone or methylprednisolone) decrease the inflammatory response to tumor invasion and edema surrounding the tumor.[3] Glucocorticoids are most helpful if the tumor is steroid-responsive, such as lymphomas. In addition, diuretics (such as furosemide) are used to reduce venous return to the heart which relieves the increased pressure.[3]
Prognosis
Symptoms are usually relieved with radiation therapy within one month of treatment.[3] However, even with treatment, 90% of patients die within two and a half years.[3] This relates to the cancerous causes of SVC that are 90% of the cases. The average age of onset of disease is 54 years of age.[3]
See also
References
- ^ a b c d e f g h i j Parker, Robert; Catherine Thomas, Lesley Bennett (2007). Emergencies in Respiratory Medicine. Oxford. pp. 96–7. ISBN 978-0-19-920244-7.
- ^ Longmore, Murray; Ian Wilkinson, Tom Turmezei, Chee Kay Cheung (2007). Oxford Handbook of Clinical Medicine. Oxford. p. 162. ISBN 0-19-856837-1.
- ^ a b c d e f g h i j k l m n emedicine > Superior Vena Cava Syndrome. Author: Michael S Beeson, MD, MBA, FACEP, Professor of Emergency Medicine, Northeastern Ohio Universities College of Medicine and Pharmacy; Attending Faculty, Summa Health System. Updated: Dec 3, 2009
- ^ define:collar of Stokes at open-resource-project.org. Retrieved Mars 2011
External links
- Superior vena cava syndrome at eMedicine
- Wilson LD, Detterbeck FC, Yahalom J (May 2007). "Clinical practice. Superior vena cava syndrome with malignant causes". N Engl J Med. 356 (18): 1862–9. doi:10.1056/NEJMcp067190. PMID 17476012.
- Randolph HL Wong, Joshua Chai, Calvin SH Ng, et al. Transvenous pacing lead-induced Superior Vena Cava Syndrome: What do we know? (2009). Surgical Practice 13 (4): 125–126. doi:10.1111/j.1744-1633.2009.00462.x.
Categories:- Paraneoplastic syndromes
- Diseases of veins, lymphatic vessels and lymph nodes
Wikimedia Foundation. 2010.