- Public health-care in China
-
- This article is about public health in Mainland China only.
China is undertaking reform of its health-care system. The New Rural Co-operative Medical Care System (NRCMCS) is a 2005 initiative to overhaul the healthcare system, particularly intended to make it more affordable for the rural poor . Under the NRCMCS, the annual cost of medical coverage is 50 yuan (US$7) per person. Of that, 20 yuan is paid in by the central government, 20 yuan by the provincial government and a contribution of 10 yuan is made by the patient. As of September 2007, around 80% of the rural population of China had signed up (about 685 million people). The system is tiered, depending on the location. If patients go to a small hospital or clinic in their local town, the system will cover roughly 70-80% of their bill. If the patient visits a county clinic, the percentage of the cost being covered falls to about 60%. If the patient requires a specialist in a modern city hospital, the plan would cover about 30% of the bill.[1]
Contents
Health indicators
Indicators of the status of China’s health sector can be found in the nation’s fertility rate of 1.8 children per woman (a 2005 estimate) and the infant mortality rate per 1,000 live births was 25.3 (a 2004 estimate).
In 2005 China had about 1,938,000 physicians (1.5 per 1,000 persons) and about 3,074,000 hospital beds (2.4 per 1,000 persons). Health expenditures on a purchasing power parity (PPP) basis were US$224 per capita in 2001, or 5.5 percent of gross domestic product (GDP). Some 37.2 percent of public expenditures were devoted to health care in China in 2001 . However, about 80 percent of the health and medical care services are concentrated in cities, and timely medical care is not available to more than 100 million people in rural areas. To offset this imbalance, in 2005 China set out a five-year plan to invest 20 billion renminbi (RMB; US$2.4 billion) to rebuild the rural medical service system composed of village clinics and township- and county-level hospitals.
Traditional and modern Chinese medicine
See also: Medicine in China, Traditional Chinese medicine, Medical missions in China, Pharmacy in China, and Pharmaceutical industry in ChinaChina has one of the longest recorded history of medicine records of any existing civilization. The methods and theories of traditional Chinese medicine have developed for over two thousand years. Western medical theory and practice came to China in the nineteenth and twentieth centuries, notably through the efforts of missionaries[2] and the Rockefeller Foundation, which together founded Peking Union Medical College. Today Chinese traditional medicine continues alongside western medicine and traditional physicians, who also receive some western medical training, are sometimes primary care givers in the clinics and pharmacies of rural China.
Although the practice of traditional Chinese medicine was strongly promoted by the Chinese leadership and remained a major component of health care, Western medicine gained increasing acceptance in the 1970s and 1980s. For example, the number of physicians and pharmacists trained in Western medicine reportedly increased by 225,000 from 1976 to 1981, and the number of physicians' assistants trained in Western medicine increased by about 50,000. In 1981 there were reportedly 516,000 senior physicians trained in Western medicine and 290,000 senior physicians trained in traditional Chinese medicine. The goal of China's medical professionals is to synthesize the best elements of traditional and Western approaches.
In practice, however, this combination has not always worked smoothly. In many respects, physicians trained in traditional medicine and those trained in Western medicine constitute separate groups with different interests. For instance, physicians trained in Western medicine have been somewhat reluctant to accept unscientific traditional practices, and traditional practitioners have sought to preserve authority in their own sphere. Although Chinese medical schools that provided training in Western medicine also provided some instruction in traditional medicine, relatively few physicians were regarded as competent in both areas in the mid-1980s.
The extent to which traditional and Western treatment methods were combined and integrated in the major hospitals varied greatly. Some hospitals and medical schools of purely traditional medicine were established. In most urban hospitals, the pattern seemed to be to establish separate departments for traditional and Western treatment. In the county hospitals, however, traditional medicine received greater emphasis.
Traditional medicine depends on herbal treatments, acupuncture, acupressure, moxibustion (the burning of herbs over acupuncture points), and "cupping" of skin with heated bamboo. Such approaches are believed to be most effective in treating minor and chronic diseases, in part because of milder side effects. Traditional treatments may be used for more serious conditions as well, particularly for such acute abdominal conditions as appendicitis, pancreatitis, and gallstones; sometimes traditional treatments are used in combination with Western treatments. A traditional method of orthopedic treatment, involving less immobilization than Western methods, continued to be widely used in the 1980s.
Primary care
After 1949 the Ministry of Public Health was responsible for all health-care activities and established and supervised all facets of health policy. Along with a system of national, provincial, and local facilities, the ministry regulated a network of industrial and state enterprise hospitals and other facilities covering the health needs of workers of those enterprises. In 1981 this additional network provided approximately 25 percent of the country's total health services.
Health care was provided in both rural and urban areas through a three-tiered system. In rural areas the first tier was made up of barefoot doctors working out of village medical centers. They provided preventive and primary-care services, with an average of two doctors per 1,000 people. At the next level were the township health centers, which functioned primarily as out-patient clinics for about 10,000 to 30,000 people each. These centers had about ten to thirty beds each, and the most qualified members of the staff were assistant doctors. The two lower-level tiers made up the "rural collective health system" that provided most of the country's medical care. Only the most seriously ill patients were referred to the third and final tier, the county hospitals, which served 200,000 to 600,000 people each and were staffed by senior doctors who held degrees from 5-year medical schools. Health care in urban areas was provided by paramedical personnel assigned to factories and neighborhood health stations. If more professional care was necessary the patient was sent to a district hospital, and the most serious cases were handled by municipal hospitals. To ensure a higher level of care, a number of state enterprises and government agencies sent their employees directly to district or municipal hospitals, circumventing the paramedical, or barefoot doctor, stage.
Post-1949 history
An emphasis on public health and preventive treatment characterized health policy from the beginning of the 1950s. At that time the party began to mobilize the population to engage in mass "patriotic health campaigns" aimed at improving the low level of environmental sanitation and hygiene and attacking certain diseases. One of the best examples of this approach was the mass assaults on the "four pests"—rats, sparrows, flies, and mosquitoes—and on schistosoma-carrying snails. Particular efforts were devoted in the health campaigns to improving water quality through such measures as deep-well construction and human-waste treatment. Only in the larger cities had human waste been centrally disposed. In the countryside, where "night soil" has always been collected and applied to the fields as fertilizer, it was a major source of disease. Since the 1950s, rudimentary treatments such as storage in pits, composting, and mixture with chemicals have been implemented. As a result of preventive efforts, such epidemic diseases as cholera, bubonic plague, typhoid fever, and scarlet fever have almost been eradicated. The mass mobilization approach proved particularly successful in the fight against syphilis, which was reportedly eliminated by the 1960s. The incidence of other infectious and parasitic diseases was reduced and controlled.
Political turmoil and famine following the failure of the Great Leap Forward led to starvation of 20 million people in China. With recovery beginning in 1961, more moderate policies inaugurated by President Liu Shaoqi ended starvation and improved nutrition. The coming of the Cultural Revolution weakened epidemic control, a rebound in epidemic disease and malnutrition in some areas.
The barefoot doctor system was based in the people's communes. With the disappearance of the people's communes, the barefoot doctor system lost its base and funding. The decollectivization of agriculture resulted in a decreased desire on the part of the rural populations to support the collective welfare system, of which health care was a part. In 1984 surveys showed that only 40 to 45 percent of the rural population was covered by an organized cooperative medical system, as compared with 80 to 90 percent in 1979.
This shift entailed a number of important consequences for rural health care. The lack of financial resources for the cooperatives resulted in a decrease in the number of barefoot doctors, which meant that health education and primary and home care suffered and that in some villages sanitation and water supplies were checked less frequently. Also, the failure of the cooperative health-care system limited the funds available for continuing education for barefoot doctors, thereby hindering their ability to provide adequate preventive and curative services. The costs of medical treatment increased, deterring some patients from obtaining necessary medical attention. If the patients could not pay for services received, then the financial responsibility fell on the hospitals and commune health centers, in some cases creating large debts.
Consequently, in the post-Mao era of modernization, the rural areas were forced to adapt to a changing health-care environment. Many barefoot doctors went into private practice, operating on a fee-for-service basis and charging for medication. But soon farmers demanded better medical services as their incomes increased, bypassing the barefoot doctors and going straight to the commune health centers or county hospitals. A number of barefoot doctors left the medical profession after discovering that they could earn a better living from farming, and their services were not replaced. The leaders of brigades, through which local health care was administered, also found farming to be more lucrative than their salaried positions, and many of them left their jobs. Many of the cooperative medical programs collapsed. Farmers in some brigades established voluntary health-insurance programs but had difficulty organizing and administering them.
Their income for many basic medical services limited by regulations, Chinese grassroots health care providers supported themselves by charging for giving injections and selling medicines. This has led to a serious problem of disease spread through health care as patients received too many injections and injections by unsterilized needles. Corruption and disregard for the rights of patients have become serious problems in the Chinese health care system.
The Chinese economist Yang Fan wrote in 2001 that lip service being given to the old socialist health care system and deliberately ignoring and failing to regulate the actual private health care system is a serious failing of the Chinese health care system. "The old argument that "health is a kind of welfare to save lives and assist the injured" is so far removed from reality that things are really more like its opposite. The welfare health system supported by public funds essentially exists in name only. People have to pay for most medical services on their own. Considering health to be still a "welfare activity" has for some time been a major obstacle to the development of proper physician - patient relationship and to the law applicable to that relationship."[3]
Despite the decline of the public health care system during the first decade of the reform era, Chinese health improved sharply as a result of greatly improved nutrition, especially in rural areas, and the recovery of the epidemic control system, which had been neglected during the Cultural Revolution.
Post-1990 history
Further information: Healthcare system reform in the People's Republic of ChinaWestern style medical facilities with international staff are available in Beijing, Shanghai, Guangzhou and a few other large cities. Many other hospitals in major Chinese cities have so-called V.I.P. wards or gaogan bingfang. These feature reasonably up-to-date medical technology and physicians who are both knowledgeable and skilled. Most V.I.P. wards also provide medical services to foreigners and have English-speaking doctors and nurses. Physicians and hospitals have sometimes refused to supply American patients with complete copies of their Chinese hospital medical records, including laboratory test results, scans, and x-rays.[citation needed]
Despite the introduction of western style medical facilities, the PRC has several emerging public health problems, which include problems as a result of pollution, a progressing HIV-AIDS epidemic, hundreds of millions of cigarette smokers,[4][5] and the increase in obesity among the population.[6][7] The HIV epidemic, in addition to the usual routes of infection, was exacerbated in the past by unsanitary practices used in the collection of blood in rural areas.[8] The problem with tobacco is complicated by the concentration of most cigarette sales in a government controlled monopoly.[5] The government, dependent on tobacco revenue, seems hesitant in its response and may even encourage it as seen from government websites.[9] Hepatitis B is endemic in mainland China, with about 10% of the population contracting the disease.[10] Some hepatitis researchers link hepatitis infections to a lower ratio of female births. If this link is confirmed, this would partially explain China's gender imbalance.[11] A program initiated in 2002 will attempt over the next 5 years to vaccinate all newborns in mainland China.[12]
Strains of avian flu outbreaks in recent years among local poultry and birds, along with a number of its citizens, have caused great concern for China and other countries. While the virus is currently mainly animal-human transmissible (with only two well documented cases of human-human have been to the present known of to scientists), experts expect an avian flu pandemic that would affect the region should the virus morph to be human-human transmissible.[13]
A more recent outbreak is the pig-human transmission of the Streptococcus suis bacteria in 2005, which has led to 38 deaths in and around Sichuan province, an unusually high number. Although the bacteria exists in other pig rearing countries, the pig-human transmission has only been reported in China.[14]
As of 2004, in more undeveloped areas it is advised to only drink bottled water as cholera, among other diseases, is spread through the water supply.
Medical Issues in China
Sex education, contraception, and women's health
Main article: Women's healthcare in the People's Republic of ChinaSex education lags in China due to cultural conservatism. Many Chinese feel that sex education should be limited to biological science. Combined with migration of young unmarried women to the cities, lack of knowledge of contraception has resulted in increasing numbers of abortions by young women.[15]
SARS
Further information: Progress of the SARS outbreakAlthough not identified until later, China’s first case of a new, highly contagious disease, severe acute respiratory syndrome (SARS), occurred in Guangdong in November 2002, and within three months the Ministry of Health reported 300 SARS cases and five deaths in the province. By May 2003, some 8,000 cases of SARS had been reported worldwide; about 66 percent of the cases and 349 deaths occurred in China alone. By early summer 2003, the SARS epidemic had ceased. A vaccine was developed and first-round testing on human volunteers completed in 2004.
The 2002 SARS in China demonstrated at once the decline of the PRC epidemic reporting system, the deadly consequences of secrecy on health matters and, on the positive side, the ability of the Chinese central government to command a massive mobilization of resources once its attention is focused on one particular issue. In 2002, the pneumonia-like SARS surfaced in Guangdong province, resulting in 348 deaths. Despite the suppression of news regarding the outbreak during the early stages of the epidemic, the outbreak was soon contained and cases of SARS failed to emerge.[16] Obsessive secrecy seriously delayed the isolation of SARS by Chinese scientists.[17] On 18 May 2004, the World Health Organization announced the PRC free of further cases of SARS.[18]
Hepatitis B
Main article: Hepatitis B in ChinaHIV and AIDS
Main article: HIV/AIDS in the People's Republic of ChinaChina, similar to other nations with migrant and socially mobile populations, has experienced increased incidences of human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS). By the mid-1980s, some Chinese physicians recognized HIV and AIDS as a serious health threat but considered it to be a "foreign problem". As of mid-1987 only two Chinese citizens had died from AIDS and monitoring of foreigners had begun. Following a 1987 regional World Health Organization meeting, the Chinese government announced it would join the global fight against AIDS, which would involve quarantine inspection of people entering China from abroad, medical supervision of people vulnerable to AIDS, and establishment of AIDS laboratories in coastal cities. Within China, the rapid increase in venereal disease, prostitution and drug addiction, internal migration since the 1980s and poorly supervised plasma collection practices, especially by the Henan provincial authorities, created conditions for a serious outbreak of HIV in the early 1990s.[19][20][21]
As of 2005 about 1 million Chinese have been infected with HIV, leading to about 150,000 AIDS deaths. Projections are for about 10 million cases by 2010 if nothing is done. Effective preventive measures have become a priority at the highest levels of the government, but progress is slow. A promising pilot program exists in Gejiu partially funded by international donors.
Tuberculosis
Main article: Tuberculosis in China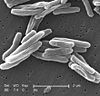 Scanning electron micrograph of Mycobacterium tuberculosis
Scanning electron micrograph of Mycobacterium tuberculosis
Tuberculosis is a major public health problem in China, which has the world's second largest tuberculosis epidemic (after India). Progress in tuberculosis control was slow during the 1990s. Detection of tuberculosis had stagnated at around 30% of the estimated total of new cases, and multidrug-resistant tuberculosis was a major problem. These signs of inadequate tuberculosis control can be linked to a malfunctioning health system. Prevalent smoking aggravates its spread.
Leprosy
Main article: Leprosy in ChinaMental health
Main article: Mental health in ChinaNutrition
In the 2000–2002 period, China had one of the highest per capita caloric intakes in Asia, second only to South Korea and higher than countries such as Japan, Malaysia, and Indonesia. In 2003, daily per capita caloric intake was 2,940 (vegetable products 78%, animal products 22%); 125% of FAO recommended minimum requirement.
Malnutrition among rural children
See also: Zhejiang Xinhua Compassion Education FoundationChina has been developing rapidly for the past 30 years. Though it has uplifted a huge number of people out of poverty, many social issues still remain unsolved. One of them is malnutrition among rural children in China. The problem has diminished but still remains a pertinent national issue. In a survey done in 1998, the stunting rate among children in China was 22 percent and was as high as 46 percent in poor provinces.[22][23] This shows the huge disparity between urban and rural areas. In 2002, Svedberg found that stunting rate in rural areas of China was 15 percent, reflecting that a substantial number of children still suffer from malnutrition.[24] Another study by Chen shows that malnutrition has dropped from 1990 to 1995 but regional differences are still huge, particularly in rural areas.[25]
In a recent report by The Rural Education Action Project on children in rural China, many were found to be suffering from basic health problems. 34 percent have iron deficiency anaemia and 40 percent are infected with intestinal worms.[26] Many of these children do not have proper or sufficient nutrition. Often, this causes them not being able to fully reap the benefits of education, which can be a ticket out of poverty.
One possible reason for poor nutrition in rural areas is that agricultural produce can fetch a decent price, and thus is often sold rather than kept for personal consumption. Rural families would not consume eggs that their hen lay but will sell it in the market for about 20 yuan per kilogram.[27] The money will then be spent on books or food like instant noodles which lack nutrition value compared to an egg. A girl named Wang Jing in China has a bowl of pork only once every five to six weeks, compared to urban children who have a vast array of food chains to choose from.
A survey conducted by China’s Ministry of Health showed the kind of food consumed by rural households. 30 percent consume meat less than once a month. 23 percent consume rice or egg less than once a month. Up to 81 percent consume less than one cup of dairy products a week. Dairy products and eggs provide essential nutrients that are important for a child’s physical development.
In a 2008 Report on Chinese Children Nutrition and Health Conditions, West China still has 7.6 million poor children who were shorter and weigh lesser than urban children. These rural children were also shorter by 4 centimetres and 0.6 kilograms lighter than World Health Organisation standards.[28] It can be concluded that children in West China still lack quality nutrition.
For China to progress even further, these social issues must be tackled. By uplifting more people out of poverty, more children will also be uplifted out of malnutrition.
Epidemiological studies
The most comprehensive epidemiological study of nutrition ever conducted was the [[China-Oxford-Cornell Study on Dietary, Lifestyle and Disease Mortality Chara
Iodine deficiency
Main article: Iodine deficiency in ChinaChina has problems in certain western provinces in iodine deficiency.[29]
Hygiene and sanitation
Further information: Water supply and sanitation in the People's Republic of ChinaBy 2002, 92 percent of the urban population and 8 percent of the rural population had access to an improved water supply, and 69 percent of the urban population and 32 percent of the rural population had access to improved sanitation facilities.
The Patriotic Health Campaign, first started in the 1950s, are campaigns aimed to improve sanitation and hygiene in China.
WHO in China
The World Health Organization (WHO) Constitution came into force on April 7, 1948, and China has been a Member since the beginning.
The WHO China office has increased its scope of activities significantly in recent years, especially following the major SARS outbreak of 2003. The role of WHO China is to provide support for the government's health programs, working closely with the Ministry of Health and other partners within the government, as well as with UN agencies and other organizations.
China's government with WHO assistance and support has strengthened public health in the nation. The current Five Year Plan incorporates public health in a significant way. The government has acknowledged that even as millions upon millions of citizens are prospering amid the country's economic boom, millions of others are lagging behind, with healthcare many cannot afford. The challenge for China is to strengthen its health care system across the spectrum, to reduce the disparities and create a more equitable situation regarding access to health care services for the population at large.
At the same time, in an ever-interconnected world, China has embraced its responsibility to global public health, including the strengthening of surveillance systems aimed at swiftly identifying and tackling the threat of infectious diseases such as SARS and avian influenza. Another major challenge is the epidemic of HIV/AIDS, a key priority for China.
The staff of the WHO Office in China are working with their national counterparts in the following areas:
- Healthcare systems development
- Immunization
- Tuberculosis control
- HIV/AIDS control
- Maternal health and child health
- Injury prevention
- Avian influenza control
- Food safety
- Tobacco control
- Non-communicable diseases control
- Environment and health
- Communicable diseases surveillance and response
In addition, WHO technical experts in specialty areas can be made available on a short-term basis, when requested by the Chinese government. China is an active, contributing member of WHO, and has made valuable contributions to global and regional health policy. Technical experts from China have contributed to WHO through their membership on various WHO technical expert advisory committees and groups.
References
- ^ The reform of the rural cooperative medical system in the People's Republic of China: interim experience in 14 pilot counties. Authors: Carrin G.1; Ron A.; Hui Y.; Hong W.; Tuohong Z.; Licheng Z.; Shuo Z.; Yide Y.; Jiaying C.; Qicheng J.; Zhaoyang Z.; Jun Y.; Xuesheng L. Source: Social Science and Medicine, Volume 48, Number 7, April 1999, pp.961-972(12) (950 people are allowed per person in china. [1]
- ^ Gulick, Edward V. (1975). Peter Parker and the Opening of China. Journal of the American Oriental Society, Vol. 95, No. 3 (Jul. - Sep., 1975). pp. 561–562.
- ^ "What Limits to Corruption in Health Care?" in April 2001 Viewpoint Voice of China translated on the U.S. Embassy Beijing website. Accessed February 7, 2007
- ^ "Smoking 'will kill one third of young Chinese men'". 16 August 2001. Honolulu Community College. Accessed 17 April 2006.
- ^ a b "China's Tobacco Industry Wields Huge Power" article by Didi Kirsten Tatlow in The New York Times June 10, 2010
- ^ "Serving the people?". 1999. Bruce Kennedy. CNN. Accessed 17 April 2006.
- ^ "Obesity Sickening China's Young Hearts" 4 August 2000. People's Daily. Accessed 17 April 2006.
- ^ "HIV and AIDS in China". 29 March 2006. AVERT. Accessed 17 April 2006.
- ^ "The Little Red Pack". 12 October 2005. Harper's Magazine. Accessed 17 April 2006.
- ^ "Prevention and control of hepatitis B in China" 2002. NCBI. Accessed 17 April 2006.
- ^ "Hepatitis B and the Case of the Missing Women". 13 August 2005. Emily Oster. Harvard University. Accessed 17 April 2006
- ^ "China launches battle against hepatitis". 1 June 2002. James Jones. BBC News. Accessed 17 April 2006.
- ^ [2] 2006. FIC. Accessed 17 April 2006.
- ^ "Streptococcus suis Outbreak, Swine and Human, China" August 2005. Veterinary Service. Accessed 17 April 2006.
- ^ "Face of Abortion in China: A Young, Single Woman" article by Jim Yardley in the New York Times April 13, 2007
- ^ "After Its Epidemic Arrival, SARS Vanishes". 15 May 2005. Jim Yardley. Accessed 17 April 2006.
- ^ "Chinese Scientists Say SARS Efforts Stymied by Organizational Obstacles China Youth Daily interview with Chinese geneticist Yang Huanming and Chinese Academy of Sciences science policy researcher Chen Hao
- ^ "China’s latest SARS outbreak has been contained, but biosafety concerns remain". 18 May 2004. World Health Organization. Accessed 17 April 2006.
- ^ July 2001 compendium, U.S. Embassy Beijing website Recent Chinese Reports on HIV/AIDS and Sexually Transmitted Diseases. Accessed May 23, 2010 via Internet Archive of U.S. Embassy Beijing website.
- ^ "Revealing the "Blood Wound" of the Spread of HIV AIDS in Henan Province --- Written on the eve of the first AIDS Day of the New Millennium" translation of email circulated history of the HIV epidemic in Henan Province.
- ^ China Health News And the Henan Province Health Scandal Cover-up translation of a report by the PRC NGO Aizhi
- ^ Park, A. and Wang, S., 2001. “China’s Poverty Statistics.” China Economic Review 12:384–98
- ^ Park, A. and Zhang, L., 2000. “Mother’s Education and Child Health in China’s Poor Areas.” Mimeo, University of Michigan Department of Economics
- ^ Svedberg, P. (2006) “Declining child malnutrition: a reassessment”, International Journal of Epidemiology, Vol. 35, No. 5, pp. 1336-46
- ^ Chen, C. 2000. “Fat Intake and Nutritional Status of Children in China.” American Journal of Clinical Nutrition 72(Supplement):1368S–72S
- ^ The Rural Education Action Project - REAP, http://reap.stanford.edu/ - a group of researchers from the Freeman Spogli Institute and the Chinese Academy of Sciences, 2008 – retrieved from www.ccap.org.cn/uploadfile/2011/0111/20110111054129822.doc on February 11, 2011
- ^ China Daily. (2008, 12 07). Retrieved February 11, 2011, from http://www.chinadaily.com.cn/china/2008-12/07/content_7279010.htm
- ^ China Daily. (2008, 12 07). Retrieved February 11, 2011, from http://www.chinadaily.com.cn/china/2008-12/07/content_7279010.htm
- ^ Google search for "iodine deficiency in China"
External links
- China Health Care Association
- Chinese Preventive Medicine Association
- China Profile by World Health Organization (WHO Office in China)
- Chinese Ministry of Health
Resources
- "Critical health literacy: a case study from China in schistosomiasis control"
- Children's Healthcare in China
- Health Information for Travelers to China U.S. Centers for Disease Control and Prevention (CDC).
- China's Healthcare System: Improving Quality of Insurance, Service, and Personnel Reforming China’s Healthcare System Roundtable series held by the Brookings-Tsinghua Center at Tsinghua University
- The Current State of Public Health in China Annual Review of Public Health Vol. 25: 327-339 (Volume publication date April 2004)
- A Critical Review of Public Health in China August 2004 paper
 People's Republic of China topics
People's Republic of China topicsHistory China (timeline) · Republic of China (1912–1949) · People's Republic of China · 1949-1976 · 1976-1989 · 1989-2002 · since 2002 · Years in the People's Republic of ChinaGeography · Natural environment Overviews Regions Terrain Bays · Canyons · Caves · Deserts · Grasslands · Hills · Islands · Mountains (ranges · passes) · Peninsulas · Northeast / North / Central Plains · Valleys · VolcanoesWater Seas Reserves Wildlife Fauna · FloraGovernment · Politics · Economy Government
and politicsConstitution · National People's Congress · President · Vice President
State Council (Premier · Vice Premier) · Civil service · Military (People's Liberation Army) · Political parties (Communist Party) · Elections · Education (universities) · National security · Foreign relations · Public health · Food safety (incidents) · Social welfare · Water supply and sanitationAdministrative
divisionsProvince level subdivisions · Cities · Baseline islands ·
Border crossingsLaw Economy History · Historical GDP · Reform · Finance · Banking (Central bank) · Currency · Agriculture · Energy · Technological and industrial history · Science and technology · Transport · Ports and harbors · Communications · Special Economic Zones (SEZs) · Foreign aid · Standard of living · PovertyPeople · Culture People Society Culture Art · Cinema · Cuisine · Literature · Media · Newspapers · Music · Philosophy · Tourism · Sports · Martial arts · Variety arts · Tea culture · Smoking · Television · Public holidays · World Heritage Sites · Archaeology · Parks · Gardens · Libraries · ArchivesOther topics Healthcare in Asia Sovereign
states- Afghanistan
- Armenia
- Azerbaijan
- Bahrain
- Bangladesh
- Bhutan
- Brunei
- Burma (Myanmar)
- Cambodia
- People's Republic of China
- Cyprus
- East Timor (Timor-Leste)
- Egypt
- Georgia
- India
- Indonesia
- Iran
- Iraq
- Israel
- Japan
- Jordan
- Kazakhstan
- North Korea
- South Korea
- Kuwait
- Kyrgyzstan
- Laos
- Lebanon
- Malaysia
- Maldives
- Mongolia
- Nepal
- Oman
- Pakistan
- Philippines
- Qatar
- Russia
- Saudi Arabia
- Singapore
- Sri Lanka
- Syria
- Tajikistan
- Thailand
- Turkey
- Turkmenistan
- United Arab Emirates
- Uzbekistan
- Vietnam
- Yemen
States with limited
recognition- Abkhazia
- Nagorno-Karabakh
- Northern Cyprus
- Palestine
- Republic of China (Taiwan)
- South Ossetia
Dependencies and
other territories- Christmas Island
- Cocos (Keeling) Islands
- Hong Kong
- Macau
Public health General Auxology • Biological hazard • Chief Medical Officer • Environmental health • Globalization and disease • Health economics • Sociology of health and illness • Medical sociology • Social psychology • Deviance (sociology) • Sociology of health and illness • Medical anthropology • Health literacy • Health policy (Health care system • Healthcare reform • Public health law) • Maternal health • Mental health • Pharmaceutical policy • Public health genomics • Public health laboratory • Reproductive health • Tropical diseasePreventive
medicineHealth promotion • Family planning • Human nutrition • Hygiene (Hand washing • Food safety • Infection control • Oral hygiene) • Occupational safety and health (Occupational hygiene • Ergonomics • Injury prevention) • Patient safety (organization) • Pharmacovigilance • Safe sex • Sanitation (Community-led total sanitation • Sanitary sewer • Waterborne diseases • Water management) • Smoking cessation • Vaccination • Vector controlPopulation
healthCommunity health • Global health • Biostatistics • Epidemiology • Health impact assessment • Health system • Public health informatics • Health software (Epi Info • OpenEpi) • Social medicine • Social determinants of health (Health equity • Race and health)Organizations, Education and History Health impact assessment • Agencies and
organizationsWorld Health Organization • European (European Centre for Disease Prevention and Control • Committee on the Environment, Public Health and Food Safety) • India (Ministry of Health and Family Welfare) • U.S. (U.S. Public Health Service (Centers for Disease Control and Prevention) • Public Health - Center for Public Health Practice • Center for Minority Health • Council on Education for Public Health • Public Health – Seattle & King County) • World Toilet Organization • Globalization and HealthEducation Health education • Bachelor of Science in Public Health • Master of Public Health • Doctor of Public Health • European Programme for Intervention Epidemiology Training (EPIET) • Professional Further Education in Clinical Pharmacy and Public HealthHistory Categories:- Public health
- Health in the People's Republic of China
Wikimedia Foundation. 2010.
