- Visual prosthesis
-
For the non-functional prosthesis or glass eye see Ocular prosthesis and Craniofacial prosthesis.
A visual prosthesis, often referred to as a bionic eye, is an experimental visual device intended to restore functional vision in those suffering from partial or total blindness. Many devices have been developed, usually modeled on the cochlear implant or bionic ear devices, a type of neural prosthesis in use since the mid 1980s.
Biological considerations
The ability to give sight to a blind person via a bionic eye depends on the circumstances surrounding the loss of sight. For retinal prostheses, which are the most prevalent visual prosthetic under development (due to ease of access to the retina among other considerations), vision loss due to degeneration of photoreceptors (retinitis pigmentosa, choroideremia, geographic atrophy macular degeneration) is the best candidate for treatment. Candidates for visual prosthetic implants find the procedure most successful if the optic nerve was developed prior to the onset of blindness. Persons born with blindness may lack a fully developed optical nerve, which typically develops prior to birth.[citation needed]
Technological considerations
Visual prosthetics are being developed as a potentially valuable aid for individuals with visual degradation. The visual prosthetic in humans remains investigational.
Ongoing projects
Argus Retinal Prosthesis
Drs. Mark Humayun and Eugene DeJuan at the Doheny Eye Institute (USC) along with Bio-electronics Engineer Dr Wentai Liu at University of California, Santa Cruz were the original inventors of the active epi-retinal prosthesis [1] and demonstrated proof of principle in acute patient investigations at Johns Hopkins University in the early 1990s along with Dr. Robert Greenberg. In the late 1990s the company Second Sight was formed by Dr. Greenberg along with medical device entrepreneur, Alfred E. Mann, to develop a chronically implantable retinal prosthesis. Their first generation implant had 16 electrodes and was implanted in 6 subjects between 2002 and 2004. Five of these subjects still use the device in their homes today. These subjects, who were all completely blind prior to implantation, can now perform a surprising array of tasks using the device. More recently, the company announced that it has received FDA approval to begin a trial of its second generation, 60 electrode implant, in the US.[2][3] Additionally they have planned clinical trials worldwide, which all got underway in 2007. Second generation Argus II trials are currently ongoing in the U.S. and are still waiting on FDA approval for public sale. Only around ten people in the U.S. currently have this model. It was recently approved in Europe, yet it costs roughly $100,000. The Argus III model is currently in process of improved sight with 240 electrodes.[4] Three major US government funding agencies (National Eye Institute, Department of Energy, and National Science Foundation) have supported the work at Second Sight, USC, UCSC, CalTech, and other research labs .
Microsystem-based Visual Prosthesis (MIVIP)
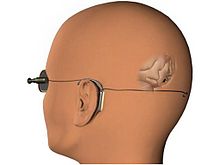
Designed by Claude Veraart at the University of Louvain, this is a spiral cuff electrode around the optic nerve at the back of the eye. It is connected to a stimulator implanted in a small depression in the skull. The stimulator receives signals from an externally-worn camera, which are translated into electrical signals that stimulate the optic nerve directly.[5]
Implantable Miniature Telescope
Although not truly an active prosthesis, an Implantable Miniature Telescope is one type of visual implant that has met with some success in the treatment of end-stage age-related macular degeneration.[6][7][8] This type of device is implanted in the eye's posterior chamber and works by increasing (by about three times) the size of the image projected onto the retina in order to overcome a centrally-located scotoma or blind spot.[7][8]
Created by VisionCare Ophthalmic Technologies in conjunction with the CentraSight Treatment Program, the telescope is about the size of a pea and is implanted behind the iris of one eye. Images are projected onto healthy areas of the central retina, outside the degenerated macula, and is enlarged to reduce the effect the blind spot has on central vision. 2.2x or 2.7x magnification strengths make it possible to see or discern the central vision object of interest while the other eye is used for peripheral vision because the eye that has the implant will have limited peripheral vision as a side effect. The implant doesn’t affect your natural eye movement; you’ll need to wear glasses and may need to sometimes use a hand-held magnifying glass to read or see fine details.[9]
Tübingen MPDA Project Alpha IMS
A Southern German team led by the University Eye Hospital in Tübingen, was formed in 1995 by Eberhart Zrenner to develop a subretinal prosthesis. The chip is located behind the retina and utilizes microphotodiode arrays (MPDA) which collect incident light and transform it into electrical current stimulating the retinal ganglion cells. As natural photoreceptors are far more efficient than photodiodes, visible light is not powerful enough to stimulate the MPDA. Therefore, an external power supply is used to enhance the stimulation current. The German team commenced in vivo experiments in 2000, when evoked cortical potentials were measured from Yucatán micropigs and rabbits. At 14 months post implantation, the implant and retina surrounding it were examined and there were no noticeable changes to anatomical integrity. The implants were successful in producing evoked cortical potentials in half of the animals tested. The thresholds identified in this study were similar to those required in epiretinal stimulation. The latest reports from this group concern the results of a clinical pilot study on 11 participants suffering from RP. Some blind patients were able to read letters, recognize unknown objects, localize a plate, a cup and cutlery. The results were to be presented in detail in 2011 in the Proceeedings of the Royal Society B (doi: 10.1098/rspb.2010.1747). In 2010 a new multicenter Study has been started using a fully implantable device with 1500 Electrodes Alpha IMS (produced by Retina Implant AG, Reutlingen, Germany), 10 patients included so far; first results have been presented at ARVO 2011.
Harvard/MIT Retinal Implant
Joseph Rizzo and John Wyatt at the Massachusetts Eye and Ear Infirmary and MIT began researching the feasibility of a retinal prosthesis in 1989, and performed a number of proof-of-concept epiretinal stimulation trials on blind volunteers between 1998 and 2000. They have since developed a subretinal stimulator, an array of electrodes, that is placed beneath the retina in the subretinal space and receives image signals beamed from a camera mounted on a pair of glasses. The stimulator chip decodes the picture information beamed from the camera and stimulates retinal ganglion cells accordingly. Their second generation prosthesis collects data and sends it to the implant through RF fields from transmitter coils that are mounted on the glasses. A secondary receiver coil is sutured around the iris.[10]
Artificial Silicon Retina (ASR)
The brothers Alan Chow and Vincent Chow have developed a microchip containing 3500 photo diodes, which detect light and convert it into electrical impulses, which stimulate healthy retinal ganglion cells. The ASR requires no externally-worn devices.[5]
The original Optobionics Corp. stopped operations, but Dr. Chow acquired the Optobionics name, the ASR implants and will be reorganizing a new company under the same name. The ASR microchip is a 2mm in diameter silicon chip (same concept as computer chips) containing ~5,000 microscopic solar cells called “microphotodiodes” that each have their own stimulating electrode.[11]
Optoelectronic Retinal Prosthesis
Daniel Palanker and his group at Stanford University have developed an optoelectronic system for visual prosthesis [12] that includes a subretinal photodiode array and an infrared image projection system mounted on video goggles. Information from the video camera is processed in a pocket PC and displayed on pulsed near-infrared (IR, 850-900 nm) video goggles. IR image is projected onto the retina via natural eye optics, and activates photodiodes in the subretinal implant that convert light into pulsed bi-phasic electric current in each pixel. Charge injection can be further increased using a common bias voltage provided by a radiofrequency-driven implantable power supply [13] Proximity between electrodes and neural cells necessary for high resolution stimulation can be achieved utilizing the effect of retinal migration.
Dobelle Eye
Main article: William H. DobelleSimilar in function to the Harvard/MIT device, except the stimulator chip sits in the primary visual cortex, rather than on the retina. Many subjects have been implanted with a high success rate and limited negative effects. Still in the developmental phase, upon the death of Dr. Dobelle, selling the eye for profit was ruled against in favor of donating it to a publicly funded research team.[5][14]
Intracortical Visual Prosthesis
Main article: Intracortical Visual ProsthesisThe Laboratory of Neural Prosthesis at Illinois Institute Of Technology (IIT), Chicago, is developing a visual prosthetic using Intracortical Iridium Oxide (AIROF) electrodes arrays. These arrays will be implanted on the occipital lobe. External hardware will capture images, process them and generate instructions which will then be transmitted to implanted circuitry via a telemetry link. The circuitry will decode the instructions and stimulate the electrodes, in turn stimulating the visual cortex. The group is developing a wearable external image capture and processing system. Studies on animals and psyphophysical studies on humans are being conducted to test the feasibility of a human volunteer implant.[citation needed]
Virtual Retinal Display (VRD)
Main article: Virtual retinal displayLaser-based system for projecting an image directly onto the retina. This could be useful for enhancing normal vision or bypassing an occlusion such as a cataract, or a damaged cornea.[5]
Visual Cortical Implant
Dr. Mohamad Sawan, Professor and Researcher at Polystim neurotechnologies Laboratory at the Ecole Polytechnique de Montreal, has been working on a visual prosthesis to be implanted into the visual cortex. The basic principle of Dr. Sawan’s technology consists of stimulating the visual cortex by implanting a silicon microchip on a network of electrodes, made of biocompatible materials, wherein each electrode injects a stimulating electrical current in order to provoke a series of luminous points to appear (an array of pixels) in the field of vision of the sightless person. This system is composed of two distinct parts: the implant and an external controller. The implant is lodged in the visual cortex and wirelessly receives data and energy from the external controller. It contains all the circuits necessary to generate the electrical stimuli and to monitor the changing microelectrode/biological tissue interface. The battery-operated outer controller consists of a micro-camera, which captures images, as well as a processor and a command generator, which process the imaging data to translate the captured images and generate and manage the electrical stimulation process. The external controller and the implant exchange data in both directions by a transcutaneous radio frequency (RF) link, which also powers the implant.[15]
Other projects
Other note-worthy researchers include Richard Normann (University of Utah) and David Bradley at University of Chicago, Eduardo Fernandez and the European Consortium CORTIVIS (http://cortivis.umh.es), Ed Tehovnik at MIT, Tohru Yagi in Japan Visual Prosthesis Project, and the Bionic Vision Australia multi-institute partnership.
See also
References
- ^ U.S. Department of Energy Office of Science. "How the Artificial Retina Works". http://artificialretina.energy.gov/howartificialretinaworks.shtml.
- ^ Second Sight (January 9, 2007). "Ending the Journey through Darkness: Innovative Technology Offers New Hope for Treating Blindness due to Retinitis Pigmentosa". http://www.2-sight.com/Argus_II_IDE_pr.htm.
- ^ Jonathan Fildes (16 February 2007). "Trials for bionic eye implants". BBC. http://news.bbc.co.uk/1/hi/sci/tech/6368089.stm.
- ^ "Bionic eye gives partial sight to blind". CBS Interactive Inc.. http://www.cbsnews.com/video/watch/?id=7358218n&tag=content;col1. Retrieved 20 March 2011.
- ^ a b c d James Geary (2002). The Body Electric. Phoenix.
- ^ Chun DW, Heier JS, Raizman MB. (2005). "Visual prosthetic device for bilateral end-stage macular degeneration.". Expert Rev Med Devices. 2 (6): 657–65. doi:10.1586/17434440.2.6.657. PMID 16293092.
- ^ a b Lane SS, Kuppermann BD, Fine IH, Hamill MB, Gordon JF, Chuck RS, Hoffman RS, Packer M, Koch DD. (2004). "A prospective multicenter clinical trial to evaluate the safety and effectiveness of the implantable miniature telescope.". Am J Ophthalmol. 137 (6): 993–1001. doi:10.1016/j.ajo.2004.01.030. PMID 15183782.
- ^ a b Lane SS, Kuppermann BD. (2006). "The Implantable Miniature Telescope for macular degeneration.". Curr Opin Ophthalmol. 17 (1): 94–8. doi:10.1097/01.icu.0000193067.86627.a1. PMID 16436930.
- ^ Lipshitz, Dr. Isaac. "Implantable Telescope Technology". VisionCare Ophthalmic Technologies, Inc.. http://www.centrasight.com/centrasight_technology. Retrieved 20 March 2011.
- ^ Wyatt, Jr., J.L.. "The Retinal Implant Project". Research Laboratory of Electronics (RLE) at the Massachusetts Institute of Technology (MIT). http://www.rle.mit.edu/media/pr151/19.pdf. Retrieved 20 March 2011.
- ^ "ASR® Device". Optobionics. http://optobionics.com/asrdevice.shtml. Retrieved 20 March 2011.
- ^ Palanker Group. "Artificial Sight: Optoelectronic Retinal Prosthesis". http://www.stanford.edu/~palanker/lab/retinalpros.html.
- ^ J.D. Loudin, D.M. Simanovskii, K. Vijayraghavan, C.K. Sramek, A.F. Butterwick, P. Huie, G.Y. McLean, and D.V. Palanker (2007). "Optoelectronic retinal prosthesis: system design and performance" (PDF). J Neural Engineering 4 (1): S72–S84. doi:10.1088/1741-2560/4/1/S09. PMID 17325419. http://www.stanford.edu/~palanker/publications/OptoelectronicRetinalProsthesis.pdf.
- ^ Simon Ings (2007). "Chapter 10(3): Making eyes to see". The Eye: a natural history. London: Bloomsbury. pp. 276–283.
- ^ Sawan. "INTRA-CORTICAL VISUAL PROSTHESIS". INTRA-CORTICAL VISUAL PROSTHESIS. Montréal Polytechnical. http://www.polymtl.ca/polystim/en/navigation/Prothesevisuelleintra-corticale.php. Retrieved April 10, 2011.
External links
- List of visual prosthesis companies
- Quantum Leap for Bionic Eye
- ARMD, Retinal Electronic Prosthesis and RPE Transplantation - eMedicine.com
- 'Bionic' eye implants look ahead - BBC
- NewScientist.com: 'Bionic eye' may help reverse blindness
- BBC: 'Artificial eye'
- How does a "bionic eye" allow blind people to see? - HowStuffWorks.com
- Research opens way for bionic eye; BBC, 24 April 2007.
- Visual Prosthesis Links; Japan Visual Prosthesis Group
- Palanker Group Publication List
- Published Papers Related to the DOE Artificial Retina Project CRADA
- The Boston Retinal Implant Project
- 'Bionic eye gives partial sight to the blind' - CBS News Video
- Implantable Telescope Technology - CentraSight
- - The Retinal Implant Project - rle.mit.edu
- - ASR® Device - optobionics.com
- - 'Tiny Technologies Raise Big Ethical Issues' - issues.control.com.au
Categories:- Blindness
- Eye
- Prosthetics
- Neuroprosthetics
- Artificial organs
- Emerging technologies
Wikimedia Foundation. 2010.