- Cystinosis
-
Cystinosis Classification and external resources 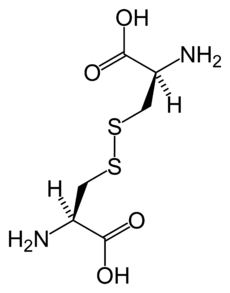
Chemical structure of cystine formed from L-cysteine (under biological conditions)ICD-10 E72.0 ICD-9 270.0 DiseasesDB 3382 eMedicine ped/538 MeSH D003554 Cystinosis is a lysosomal storage disease characterized by the abnormal accumulation of the amino acid cystine.[1] It is a genetic disorder that typically follows an autosomal recessive inheritance pattern. Cystinosis is the most common cause of Fanconi syndrome in the pediatric age group. Fanconi syndrome occurs when the function of cells in renal tubules are impaired, leading to abnormal amounts of carbohydrates and amino acids in the urine, excessive urination, and low blood levels of potassium and phosphates.
Contents
Diagnosis
Cystinosis is a rare genetic disorder[2] that causes an accumulation of the amino acid cystine within cells, forming crystals that can build up and damage the cells. These crystals negatively affect many systems in the body, especially the kidneys and eyes.[1]
The accumulation is caused by abnormal transport of cystine from lysosomes, resulting in a massive intra-lysosomal cystine accumulation in tissues. Via an as yet unknown mechanism, lysosomal cystine appears to amplify and alter apoptosis in such a way that cells die inappropriately, leading to loss of renal epithelial cells. This results in renal Fanconi syndrome,[3] and similar loss in other tissues can account for the short stature, retinopathy, and other features of the disease.
Definitive diagnosis and treatment monitoring are most often performed through measurement of white blood cell cystine level using tandem mass spectrometry.
Symptoms
There are three distinct types of cystinosis each with slightly different symptoms: nephropathic cystinosis, intermediate cystinosis, and non-nephropathic or ocular cystinosis. Infants affected by nephropathic cystinosis initially exhibit poor growth and particular kidney problems (sometimes called renal Fanconi syndrome). The kidney problems lead to the loss of important minerals, salts, fluids, and other nutrients. The loss of nutrients not only impairs growth, but may result in soft, bowed bones (hypophosphatemic rickets), especially in the legs. The nutrient imbalances in the body lead to increased urination, thirst, dehydration, and abnormally acidic blood (acidosis).
By about age two, cystine crystals may also be present in the cornea. The buildup of these crystals in the eye causes an increased sensitivity to light (photophobia). Without treatment, children with cystinosis are likely to experience complete kidney failure by about age ten. Other signs and symptoms that may occur in untreated patients include muscle deterioration, blindness, inability to swallow, diabetes, and thyroid and nervous system problems.
The signs and symptoms of intermediate cystinosis are the same as nephropathic cystinosis, but they occur at a later age. Intermediate cystinosis typically begins to affect individuals around age twelve to fifteen. Malfunctioning kidneys and corneal crystals are the main initial features of this disorder. If intermediate cystinosis is left untreated, complete kidney failure will occur, but usually not until the late teens to mid twenties.
People with non-nephropathic or ocular cystinosis do not usually experience growth impairment or kidney malfunction. The only symptom is photophobia due to cystine crystals in the cornea.
It is currently being researched at UC San Diego, The University of Michigan, Tulane University School of Medicine, and at the National Institutes of Health in Bethesda, Maryland as well as at Robert Gordon University in Aberdeen and in Sunderland, UK as well as the Necker Hospital in Paris.
Genetics
Cystinosis occurs due to a mutation in the gene CTNS, located on chromosome 17, which codes for cystinosin, the lysosomal cystine transporter. Symptoms are first seen at about 3 to 18 months of age with profound polyuria (excessive urination), followed by poor growth, photophobia, and ultimately kidney failure by age 6 years in the nephropathic form.
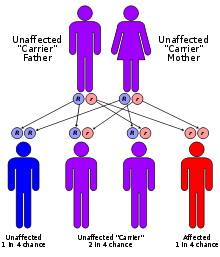
All forms of cystinosis (nephropathic, juvenile and ocular) are autosomal recessive, which means that the trait is located on an autosomal gene, and an individual who inherits two copies of the gene - one from both parents - will have the disorder. There is a 25% risk of having a child with the disorder, when both parents are carriers of an autosomal recessive trait.
Cystinosis affects approximately 1 in 100,000 to 200,000 newborns.[4] and there are only around 2,000 known individuals with cystinosis in the world. The incidence is higher in the province of Brittany, France, where the disorder affects 1 in 26,000 individuals.[5]
Treatment
Cystinosis is normally treated with a drug called cysteamine (brand name Cystagon).[6] The administration of cysteamine can reduce the intracellular cystine content. Cysteamine concentrates inside the lysosomes and reacts with cystine to form both cysteine and a cysteine-cysteamine complex, which are able to leave the lysosomes. When administered regularly, cysteamine decreases the amount of cystine stored in lysosomes and correlates with conservation of renal function and improved growth.[6] Cysteamine eyedrops remove the cystine crystals in the cornea that can cause photophobia if left unchecked. Patients with cystinosis are also often given sodium citrate to treat the blood acidosis, as well as potassium and phosphorus supplements. If the kidneys become significantly impaired or fail, then treatment must be begun to ensure continued survival, up to and including renal transplantation.
Types
- Online 'Mendelian Inheritance in Man' (OMIM) 219800 - Infantile nephropathic
- Online 'Mendelian Inheritance in Man' (OMIM) 219900 - Adolescent nephropathic
- Online 'Mendelian Inheritance in Man' (OMIM) 219750 - Adult nonnephropathic
See also
- Hartnup disease
- Cystinuria
- Fanconi syndrome
- genetic disease
- Cystinosis at NLM Genetics Home Reference
References
- ^ a b A. Gahl, William; Jess G. Thoene and Jerry A. Schneider (2002). "Cystinosis". N Engl J Med 347 (2): 111–121. doi:10.1056/NEJMra020552. PMID 12110740.
- ^ Cystinosis
- ^ Howard G. WORTHEN, N; Robert A. GOOD (1958). "The de Toni-Fanconi Syndrome with Cystinosis". AMA J Dis Child. 95 (6): 653–688. PMID 1353216.
- ^ "Cystinosis on Genetic home reference". http://ghr.nlm.nih.gov/condition=cystinosis.
- ^ Kalatzis, V; Cherqui S, Jean G, Cordier B, Cochat P, Broyer M, Antignac C (October 2001). "Characterization of a putative founder mutation that accounts for the high incidence of cystinosis in Brittany". J Am Soc Nephrol 12 (10): 2170–2174. PMID 11562417. http://jasn.asnjournals.org/content/12/10/2170.long. Retrieved 31 March 2011.
- ^ a b William A. Gahl, William A.; George F. Reed, Ph.D., Jess G. Thoene, M.D., Joseph D. Schulman, M.D., William B. Rizzo, M.D., Adam J. Jonas, M.D., Daniel W. Denman, M.A., James J. Schlesselman, Ph.D., Brian J. Corden, M.D., and Jerry A. Schneider, M.D. (1987). "Cysteamine Therapy for Children with Nephropathic Cystinosis". N Engl J Med 316 (16): 971–977. doi:10.1056/NEJM198704163161602. PMID 3550461.
External links
- Cystinosis Research Network - a non-profit organization advocating research, providing family assistance, and educating the public about cystinosis.
- Cystinosis Patient Registry - contribute to research and be informed of available clinical trials and studies
- GeneReviews/NCBI/NIH/UW entry on Cystinosis
- Cystinosis - Cystinosis Research Foundation- an international research support and education foundation
- BC Health Guide
- Cystinosis Foundation UK - a UK Charity Supporting Families & Research
- Hide and Seek Foundation For Lysosomal Disease Research
Inborn error of amino acid metabolism (E70–E72, 270) K→acetyl-CoA HypertryptophanemiaG Glutamate/glutamineG→fumarateType II tyrosinemia · Type III tyrosinemia/Hawkinsinuria · Alkaptonuria/Ochronosis · Type I tyrosinemiaTransport/
IE of RTTOther Categories:- Autosomal recessive disorders
- Amino acid metabolism disorders
- Lysosomal storage diseases
Wikimedia Foundation. 2010.