- Dopamine beta hydroxylase deficiency
-
Dopamine beta hydroxylase deficiency Classification and external resources 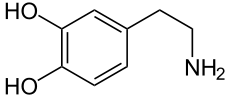
Dopamine beta hydroxylase is the enzyme responsible for converting dopamine (pictured) to norepinephrine.OMIM 223360 DiseasesDB 33227 Dopamine beta hydroxylase deficiency is a condition involving inadequate Dopamine beta hydroxylase.
Contents
Symptoms
A deficiency of norepinephrine and epinephrine that causes orthostatic hypotension, nasal stuffiness, and droopy eyelids (ptosis) among other symptoms. Some people refer to this as norepinephrine deficiency. It's caused by largely increased amounts of serum dopamine and release of dopamine in place of norepinephrine. It is difficult for people with this to stand still for longer than one minute. Another symptom is hypoglycemia which is thought to be caused by adrenomedullary failure and the T-wave abnormalities from failure of noradrenergic control. Also, prolactin is frequently suppressed by excessive dopamine. This can also have an impact on digestion. "Dopamine has an emetic effect and inhibitis digestive motricity"[1]. People with dopamine beta hydroxylase deficiency may have a paradoxical response to NRI antidepressant medication such as Edronax -- they may experience more depression, less energy, and become more sleepy. This is a form of dysautonomia but differentiated from familial dysautonomia by lack of familial dysautonomic symptoms such as loss of sense of pain and smell.
Medications
Most people can be treated using L-Threo-DOPS. Some other OTC medications can be beneficial as well. Researchers of disorders such as depression, schizophrenia, and migraines are very interested in studying this disorder, as the persons generally have triple fold amounts of dopamine in their system and yet are generally normal.
Other medications that can bring relief include:[2]
- phenylpropanolamine- due to pressor response to vascular α-adrenoceptors.[3]
- indomethacin[citation needed]
Circumstances to Avoid
Untreated individuals with DBH deficiency should avoid hot environments, strenuous exercise, standing still, and dehydration. [4][5]
References
- ^ "Dopamine receptor antagonists". Pharmacorama. 2005-06-19. http://www.pharmacorama.com/en/Sections/Catecholamines_7_4.php. Retrieved 2010-04-29.
- ^ Roberta A Pagon, Thomas C Bird, Cynthia R Dolan, Karen Stephens, David Robertson, Emily M Garland. "Dopamine Beta-Hydroxylase Deficiency". GeneReviews - NCBI Bookshelf. http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=dbh#dbh.REF.robertson.1990.1. Retrieved 2010-04-29.
- ^ Robertson D, Hollister AS, Biaggioni I (1990). "Dopamine-b-hydroxylase deficiency and cardiovascular control". In Laragh JH, Brenner BM. Hypertension Pathophysiology, Diagnosis and Management. New York: Raven Press Ltd. pp. 749–59.
- ^ Senard JM, Rouet P (2006). "Dopamine beta-hydroxylase deficiency". Orphanet Journal of Rare Diseases 1: 7. doi:10.1186/1750-1172-1-7. PMC 1459119. PMID 16722595. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1459119.
- ^ Roberta A Pagon, Thomas C Bird, Cynthia R Dolan, Karen Stephens, David Robertson, Emily M Garland. "Dopamine Beta-Hydroxylase Deficiency". GeneReviews - NCBI Bookshelf. http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=dbh. Retrieved 2010-04-29.
External links
- GeneReviews/NCBI/NIH/UW entry on Dopamine Beta-Hydroxylase Deficiency
- Fu W, Shen J, Luo X, et al. (September 2007). "Dopamine D1 receptor agonist and D2 receptor antagonist effects of the natural product (-)-stepholidine: molecular modeling and dynamics simulations". Biophysical Journal 93 (5): 1431–41. doi:10.1529/biophysj.106.088500. PMC 1948031. PMID 17468175. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1948031.
- National Dysautonomia Research Foundation
- Alaniz RC, Thomas SA, Perez-Melgosa M, et al. (March 1999). "Dopamine beta-hydroxylase deficiency impairs cellular immunity". Proceedings of the National Academy of Sciences of the United States of America 96 (5): 2274–8. doi:10.1073/pnas.96.5.2274. PMC 26773. PMID 10051631. http://www.pnas.org/cgi/pmidlookup?view=long&pmid=10051631.
Inborn error of amino acid metabolism (E70–E72, 270) K→acetyl-CoA Lysine/straight chainHypertryptophanemiaG G→pyruvate→citrateG→glutamate→
α-ketoglutarateGlutamate/glutamineG→fumarateType II tyrosinemia · Type III tyrosinemia/Hawkinsinuria · Alkaptonuria/Ochronosis · Type I tyrosinemiaDopamine beta hydroxylase deficiency · reverse: Brunner syndromeTransport/
IE of RTTOther Categories:- Amino acid metabolism disorders
Wikimedia Foundation. 2010.
