- Testicular cancer
-
Testicular Cancer Classification and external resources 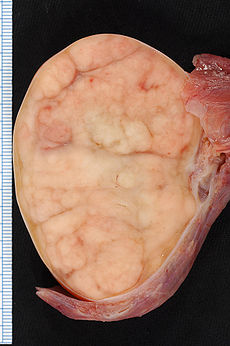
7.4 × 5.5-cm seminoma in a radical orchiectomy specimen.ICD-10 C62 ICD-9 186.9 OMIM 273300 DiseasesDB 12966 eMedicine med/2250 med/863 MeSH D013736 Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system.
In the United States, between 7,500 and 8,000 diagnoses of testicular cancer are made each year.[1][2] In the UK, approximately 2,000 men are diagnosed each year.[3] Over his lifetime, a man's risk of testicular cancer is roughly 1 in 250 (0.4%). It is the most common cancer in males aged 20–39 years, the period of peak incidence, and is rarely seen before the age of 15 years.[4] Testicular cancer has one of the highest cure rates of all cancers: in excess of 90 percent; essentially 100 percent if it has not spread (metastasized).[5] Even for the relatively few cases in which malignant cancer has spread widely, modern chemotherapy offers a cure rate of at least 80%.[6] Not all lumps on the testicles are tumors, and not all tumors are malignant; there are many other conditions such as testicular microlithiasis, epididymal cysts, appendix testis (hydatid of Morgagni), and so on which may be painful but are non-cancerous.
Contents
Classification
Although testicular cancer can be derived from any cell type found in the testicles, more than 95% of testicular cancers are germ cell tumors. Most of the remaining 5% are sex cord-gonadal stromal tumours derived from Leydig cells or Sertoli cells. Correct diagnosis is necessary to ensure the most effective and appropriate treatment. To some extent, this can be done via blood tests for tumor markers, but definitive diagnosis requires examination of the histology of a specimen by a pathologist.
Most pathologists use the World Health Organization Classification system for testicular tumours:[7][8]
- Germ cell tumours
-
- Precursor lesions
-
-
- Unclassified type (carcinoma in situ)
- Specifed types
-
- Tumours of one histologic type (pure forms)
-
-
- Variant - Seminoma with syncytiotrophoblastic cells
-
- Variant - spermatocytic seminoma with sarcoma
- Embryonal carcinoma
- Yolk sac tumour
- Trophoblastic tumours
-
-
- Variant - monophasic choriocarcinoma
- Placental site trophoblastic tumour
- Cystic trophoblastic tumour
-
-
- Variant - Dermoid cyst
- Variant - Epidermoid cyst
- Variant - Monodermal teratoma (Carcinoid, Primitive neuroectodermal tumour (PNET), Nephroblastoma-like tumor, others.
- Variant - Teratomic with somatic-type malignancy
-
- Tumours of more than one histologic type (mixed forms)
-
- Embryonal carcinoma and teratoma
- Teratoma and seminoma
- Choriocarcinoma and teratoma.embryonal carcinoma
- Others
- Sex cord/Gonadal stromal tumours
-
- Leydig cell tumour
- Sertoli cell tumour
-
- Lipid rich variant
- Scleriosing variant
- Large cell calcifying variant
- Intratubular sertoli cell neoplasia in Peutz-Jeghers syndrome
-
- Adult type
- Juvenile type
- Thecoma Fibroma Group
- Sex cord/gonadal stromal tunour - incompletely differentiated
- Sex cord/gonadal stromal tumour - mixed types
- Mixed Germ Cell and Sex Cord/Gonadal Stromal Tumours
-
- Gonadoblastoma
- Germ cell-sex cord/gonadal stromal tumour, unclassified
- Miscellaneous tumours of the testis
-
- Carcinoid
- Tumours of ovarian epithelial types
-
- Serous tumour of borderline malignancy
- Serous carcinoma
- Well differentiated endometrioid tumour
- Mucinous cystadenoma
- Mucinous cystadenocarcinoma
- Brenner tumour
- Nephroblastoma
- Paraganglioma
- Haematopoietic tumours
- Tumours of collecting ducts and rete
- Tumours of the paratesticular structures
-
- Adenomatoid tumour
- Malignant and Benign Mesothelioma
- Adenocarcinoma of the epididymis
- Papillary cystadenoma of the epididymis
- Melanotic neuroectodermal tumour
- Desmoplastic small round cell tumour
- Mesenchymal tumours of the spermatic cord and testicular adnexae
-
- Lipoma
- Liposarcoma
- Rhabdomyosarcoma
- Aggressive angiomyxoma
- Angiomyofibroblastoma-like tumour (see Myxoma)
- Fibromatosis
- Fibroma
- Solitary fibrous tumour
- Others
- Secondary tumours of the testis
Signs and symptoms
One of the first signs of testicular cancer is often a lump or swelling in the testes. The U.S. Preventive Services Task Force (USPSTF) recommends against routine screening for testicular cancer in asymptomatic adolescent and adults, which means that men should not perform routine testicular self-exams.[9] This practice was encouraged in the past, but current scientific evidence suggests that screening for testicular cancer does not lead to decreased morbidity and mortality.[10] However, the American Cancer Society suggests that some men should examine their testicles monthly, especially if they have a family history of cancer.[11]
Symptoms may also include one or more of the following:
- a lump in one testis which may or may not be painful [12][13]
- sharp pain or a dull ache in the lower abdomen or scrotum[13]
- a feeling often described as "heaviness" in the scrotum[13]
- breast enlargement (gynecomastia) from hormonal effects of β-hCG[12][13]
- low back pain (lumbago) tumor spread to the lymph nodes along the back[12][13]
It is not very common for testicular cancer to spread to other organs, apart from the lungs. However, if it has, the following symptoms may be present:
- shortness of breath (dyspnea), cough or coughing up blood (hemoptysis) from metastatic spread to the lungs[12][13]
- a lump in the neck due to metastases to the lymph nodes[12][13]
Genetic defects
Most testicular germ cell tumors have too many chromosomes, and most often they are triploid to tetraploid. An isochromosome 12p (the short arm of chromosome 12 on both sides of the same centromere) is present in about 80% of the testicular cancers, and also the other cancers usually have extra material from this chromosome arm through other mechanisms of genomic amplification.[14]
Diagnosis
The main way testicular cancer is diagnosed is via a lump or mass inside the testis. More generally, if a young adult or adolescent has a single enlarged testicle, which may or may not be painful, this should give doctors reason to suspect testicular cancer.
Other conditions may also have symptoms similar to testicular cancer:
Incorrect or mistaken diagnosis can delay access to appropriate treatment; this is thought to occur in up to 25% of cases[citation needed]
The nature of any palpated lump in the scrotum is often evaluated by scrotal ultrasound, which can determine exact location, size, and some characteristics of the lump, such as cystic vs solid, uniform vs heterogeneous, sharply circumscribed or poorly defined. The extent of the disease is evaluated by CT scans, which are used to locate metastases.
The differential diagnosis of testicular cancer requires examining the histology of tissue obtained from an inguinal orchiectomy - that is, surgical excision of the entire testis along with attached structures (epididymis and spermatic cord). A biopsy should not be performed, as it raises the risk of spreading cancer cells into the scrotum.
Inguinal orchiectomy is the preferred method because it lowers the risk of cancer cells escaping. This is because the lymphatic system of the scrotum, through which white blood cells (and, potentially, cancer cells) flow in and out, links to the lower extremities, while that of the testicle links to the back of the abdominal cavity (the retroperitoneum). A transscrotal biopsy or orchiectomy will potentially leave cancer cells in the scrotum and create two routes for cancer cells to spread, while in an inguinal orchiectomy only the retroperitoneal route exists.
Blood tests are also used to identify and measure tumor markers (usually proteins present in the bloodstream) that are specific to testicular cancer. AFP alpha1 feto protein, Beta-HCG, and LDH are the typical markers used to identify testicular cancer.
Staging
After removal, the testicle is fixed with Bouin's solution[15][16] because it better conserves some morphological details such as nuclear conformation. Then the testicular tumor is staged by a pathologist according to the TNM Classification of Malignant Tumors as published in the AJCC Cancer Staging Manual. Testicular cancer is categorized as being in one of three stages (which have subclassifications). The size of the tumor in the testis is irrelevant to staging.[17] In broad terms, testicular cancer is staged as follows:
- Stage I: the cancer remains localized to the testis.
- Stage II: the cancer involves the testis and metastasis to retroperitoneal and/or Paraaortic lymph nodes (lymph nodes below the diaphragm).
- Stage III: the cancer involves the testis and metastasis beyond the retroperitoneal and Paraaortic lymph nodes. Stage 3 is further subdivided into non-bulky stage 3 and bulky stage 3.[18]
Further information on the detailed staging system is available on the website of the American Cancer Society.[19]
Treatment
Since testicular cancers can spread, patients are usually offered adjuvant treatment - in the form of chemotherapy or radiotherapy - after surgery to remove the affected testicle (orchiectomy). The type of adjuvant therapy depends largely on the histology of the tumor (i.e. the size and shape of its cells under the microscope) and the stage of progression at the time of surgery (i.e how far cells has 'escaped' from the testicle, invaded the sorrounding tissue, or spread to the rest of the body). If the cancer is not particularly advanced, patients may be offered careful surveillance by frequent CT scans and blood tests, in place of adjuvant treatment.
Before 1970, survival rates from testicular cancer were low. Since the introduction of adjuvant chemotherapy, chiefly platinum-based drugs like cisplatin and carboplatin, the outlook has improved substantially. Although 7000 to 8000 new cases of testicular cancer occur in the United States yearly, only 400 men are expected to die of the disease.
In the UK, a similar trend has emerged: since improvements in treatment, survival rates have risen rapidly to cure rates of over 95%.[20]
The three basic types of treatment are surgery, radiation therapy, and chemotherapy.[21]
Surgery is performed by urologists; radiation therapy is administered by radiation oncologists; and chemotherapy is the work of medical oncologists. In most patients with testicular cancer, the disease is cured readily with minimal long-term morbidity.
Surgery
Orchiectomy
While it may be possible, in some cases, to remove testicular cancer tumors from a testis while leaving the testis functional, this is almost never done, as the affected testicle usually contains pre-cancerous cells spread throughout the entire testicle. Thus removing the tumor alone without additional treatment greatly increases the risk that another cancer will form in that testicle . Since only one testis is typically required to maintain fertility, hormone production, and other male functions, the afflicted testis is almost always removed completely in a procedure called inguinal orchiectomy. (The testicle is almost never removed through the scrotum; an incision is made beneath the belt line in the inguinal area.) In the UK, the procedure is known as a radical orchidectomy.
Retroperitoneal Lymph Node Dissection (RPLND)
In the case of nonseminomas that appear to be stage I, surgery may be done on the retroperitoneal/Paraaortic lymph nodes (in a separate operation) to accurately determine whether the cancer is in stage I or stage II and to reduce the risk that malignant testicular cancer cells that may have metastasized to lymph nodes in the lower abdomen. This surgery is called Retroperitoneal Lymph Node Dissection (RPLND). However, this approach, while standard in many places, especially the United States, is out of favor due to costs and the high level of expertise required to perform the surgery. The urologist may take extra care in the case of males who have not fathered children, to preserve the nerves involved in ejaculation.
Many patients are instead choosing surveillance, where no further surgery is performed unless tests indicate that the cancer has returned. This approach maintains a high cure rate because of the growing accuracy of surveillance techniques.
Lymph node surgery may also be performed after chemotherapy to remove masses left behind, particularly in the cases of advanced initial cancer or large nonseminomas.
Radiation therapy
Radiation may be used to treat stage 2 seminoma cancers, or as adjuvant (preventative) therapy in the case of stage 1 seminomas, to minimize the likelihood that tiny, non-detectable tumors exist and will spread (in the inguinal and para-aortic lymph nodes). Radiation is never used as a primary therapy for nonseminoma.
Chemotherapy
As an adjuvant treatment, use of chemotherapy as an alternative to radiation therapy in the treatment of seminoma is increasing, because radiation therapy appears to have more significant long-term side effects (for example, internal scarring, increased risks of secondary malignancies, etc.). Two doses, or occasionally a single dose of carboplatin, typically delivered three weeks apart, is proving to be a successful adjuvant treatment, with recurrence rates in the same ranges as those of radiotherapy. However, very long term data on the efficacy of adjuvant carboplatin in this setting does not exist. Since seminoma can recur decades after the primary tumor is removed, patients receiving adjuvant chemotherapy should remain vigilant and not assume they are cured 5 years after treatment. The concept of carboplatin as a single-dose therapy was developed by Tim Oliver, Professor of Medical Oncology at Barts and The London School of Medicine and Dentistry.[22]
Chemotherapy is the standard treatment for non-seminoma when the cancer has spread to other parts of the body (that is, stage 2B or 3). The standard chemotherapy protocol is three, or sometimes four, rounds of Bleomycin-Etoposide-Cisplatin (BEP). Bleomycin, etoposide and cisplatin (BEP) as a first-line treatment was first reported by Professor Michael Peckham in 1983.[23] The landmark trial published in 1987 which established BEP as the optimum treatment was conducted by Dr. Lawrence Einhorn at Indiana University.[24] An alternative, equally effective treatment involves the use of four cycles of Etoposide-Cisplatin (EP).
While treatment success depends on the stage, the average survival rate after five years is around 95%, and stage 1 cancers cases (if monitored properly) have essentially a 100% survival rate (which is why prompt action, when testicular cancer is a possibility, is extremely important).
Prognosis
In the New England Journal of Medicine, treatment of testicular cancer has been called one of the success stories of modern medicine, with sustained response to treatment in more than 90% of cases, regardless of stage.[25] Because of advances in chemotherapy, cure rates now approach 85% overall, with better than 95% for localized disease and 80% for metastatic disease—the best response by any solid tumor.[6]
Surveillance
For many patients with stage I cancer, adjuvant (preventative) therapy following surgery may not be appropriate and patients will undergo surveillance instead.[26] The form this surveillance takes, e.g. the type and frequency of investigations and the length time it should continue, will depend on the type of cancer (non-seminoma or seminoma), but the aim is to avoid unnecessary treatments in the many patients who are cured by their surgery, and ensure that any relapses with metastases (secondary cancers) are detected early and cured. This approach ensures that chemotherapy and or radiotherapy is only given to the patients that need it. The number of patients ultimately cured is the same using surveillance as post-operative “adjuvant” treatments, but the patients have to be prepared to follow a prolonged series of visits and tests.
For both non-seminomas and seminomas, surveillance tests generally include physical examination, blood tests for tumour markers, chest x-rays and CT scanning. However, the requirements of a surveillance programme differ according to the type of disease since, for seminoma patients, relapses can occur later and blood tests are not as good at indicating relapse.
CT scans are performed on the abdomen (and sometimes the pelvis) and also the chest in some hospitals. Chest x-rays are increasingly preferred for the lungs as they give sufficient detail combined with a lower false-positive rate and significantly smaller radiation dose than CT.
The frequency of CT scans during surveillance should ensure that relapses are detected at an early stage while minimising the radiation exposure.
For patients treated for stage I non-seminoma, a randomised trial (Medical Research Council TE08[27]) showed that, when combined with the standard surveillance tests described above, 2 CT scans at 3 and 12 months were as good as 5 over 2 years in detecting relapse at an early stage.
For patients treated for stage I seminoma who choose surveillance rather than undergoing adjuvant therapy, there have been no randomised trials to determine the optimum frequency of scans and visits, and the schedules vary very widely across the world, and within individual countries. In the UK there is an ongoing clinical trial called TRISST.[28][29] This is assessing how often scans should take place and whether magnetic resonance imaging (MRI) can be used instead of CT scans. MRI is being investigated because it does not expose the patient to radiation and so, if it is shown to be as good at detecting relapses, it may be preferable to CT. It is possible that one or more centres in Canada may join the trial in the next year or so.
For more advanced stages of testicular cancer, and for those cases in which radiation therapy or chemotherapy was administered, the extent of monitoring (tests) after treatment will vary on the basis of the circumstances, but normally should be done for five years in uncomplicated cases and for longer in those with higher risks of relapse.
Fertility
A man with one remaining testis can lead a normal life, because the remaining testis takes up the burden of testosterone production and will generally have adequate fertility.[30] However, it is worth the (minor) expense of measuring hormone levels before removal of a testicle, and sperm banking may be appropriate for younger men who still plan to have children, since fertility may be lessened by removal of one testicle[citation needed], and can be severely affected if extensive chemotherapy and/or radiotherapy is done.
Less than five percent of those who have testicular cancer will have it again in the remaining testis. A man who loses both testicles will normally have to take hormone supplements (in particular, testosterone, which is created in the testicles), and will be infertile, but can lead an otherwise normal life.
Epidemiology
Testicular cancer is most common among Caucasian men and rare among men of African descent.[31] Testicular cancer is uncommon in Asia and Africa. Worldwide incidence has doubled since the 1960s, with the highest rates of prevalence in Scandinavia, Germany, and New Zealand.
Incidence among African Americans doubled from 1988 to 2001 with a bias towards seminoma. The lack of significant increase in the incidence of early-stage testicular cancer during this timeframe suggests that the overall increase was not due to heightened awareness of the disease.
Although testicular cancer is most common among men aged 15–40 years, it has three peaks: infancy through the age of four as teratomas and yolk sac tumors, ages 25–40 years as post-pubertal seminomas and nonseminomas, and from age 60 as spermatocytic seminomas.[32]
Germ cell tumors of the testis are the most common cancer in young men between the ages of 15 and 35 years.[33]
A major risk factor for the development of testis cancer is cryptorchidism (undescended testicles). It is generally believed that the presence of a tumor contributes to cryptorchidism; when cryptorchidism occurs in conjunction with a tumor then the tumor tends to be large. Other risk factors include inguinal hernia,[34] mumps orchitis. [35] Physical activity is associated with decreased risk and sedentary lifestyle is associated with increased risk. Early onset of male characteristics is associated with increased risk. These may reflect endogenous or environmental hormones.
In other animals
Testicular tumors occur also in animals. In horses, these include interstitial cell tumors and teratomas. Typically, the former are found in older stallions (affected stallions may become extremely vicious, suggesting excessive production of androgen), and the latter are found in young horses and are large.[36]
Notable people who had testicular cancer
- Lance Armstrong, American former professional road racing cyclist
- Niklas Axelsson, Swedish professional road racing cyclist
- Jake Burton Carpenter, founder of Burton Snowboards
- Bob Champion, English jump jockey
- Aaron Cruden, New Zealand Rugby Union player
- Colin Curtis, MLB outfielder for the New York Yankees
- Kevin Curtis, American NFL football wide receiver
- Tyson Edwards, former AFL player for the Adelaide Crows
- Tom Green, Canadian actor, rapper, comedian, and talk show host
- Neil Harris, English footballer
- John Hartson, former Welsh footballer
- Markel Irizar, Spanish professional road bicycle racer
- Sébastien Joly, French professional road racing cyclist
- Phil Kessel, American professional ice hockey forward
- John Kruk, American former major league baseball player
- Mark Latham, former leader of the Federal Parliamentary Australian Labor Party and Leader of the Opposition
- Michael Lowell, former major league baseball third baseman
- Billy Mayfair, American PGA professional golfer
- Robert Schwentke, German film director
- Craig Moore, former Australian footballer
- Gunnar Nilsson, (20 November 1948 – 20 October 1978), Swedish racing driver
- Pete Postlethwaite, English actor
- Chris Reason, Australian television news reporter
- Scott Schoeneweis, American Major League Baseball left-handed relief pitcher
References
- ^ Cancer Facts and Figures 2003. Atlanta, GA: American Cancer Society. 2003. http://www.cancer.org/downloads/STT/CAFF2003PWSecured.pdf. Retrieved 2008-04-24.
- ^ Cancer Facts and Figures 2007. Atlanta, GA: American Cancer Society. 2007. http://www.cancer.org/downloads/STT/CAFF2007PWSecured.pdf. Retrieved 2008-04-24.
- ^ CancerStats, 2007 UK incidence data, Cancer Research UK.
- ^ Hayes-Lattin, Brandon; Nichols, Craig R. (October 2009). "Testicular Cancer: A Prototypic Tumor of Young Adults". Seminars in oncology 36 (5): 432–438. doi:10.1053/j.seminoncol.2009.07.006. PMC 2796329. PMID 19835738. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2796329.
- ^ {{[1]}}
- ^ a b Feldman DR; Bosl GJ, Sheinfeld J, Motzer RJ (February 13, 2008). "Medical treatment of advanced testicular cancer". JAMA 299 (6): 672–684. doi:10.1001/jama.299.6.672. PMID 18270356. http://jama.ama-assn.org/cgi/content/full/299/6/672. Retrieved June 24, 2011.
- ^ Eble J.N., Sauter G., Epstein J.I., Sesterhenn I.A. (Eds.): World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. IARC Press: Lyon 2004. ISBN 92 832 2412 4
- ^ Mills, S (ed.) 2009.Sternberg's Diagnostic Pathology. 5th Edition. ISBN 978-0-7817-7942-5
- ^ http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm
- ^ Screening for testicular cancer: a brief evidence update for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality; February 2004. http://www.ahrq.gov/clinic/3rduspstf/testicular/testiculup.htm
- ^ Testicular Cancer: Early Detection, Diagnosis, and Staging. July 2010. http://www.cancer.org/Cancer/TesticularCancer/DetailedGuide/testicular-cancer-detection
- ^ a b c d e Motzer, Robert J.; Bosl, George J. (2005). "82. Testicular Cancer". In Kasper, Dennis L.; Jameson, J. Larry. Harrison's Principles of Internal Medicine (16th ed.). McGraw-Hill. pp. 550–553. ISBN 0071391401.
- ^ a b c d e f g Shaw, Joel (February 15, 2008). "Diagnosis and Treatment of Testicular Cancer". American Family Physician (American Academy of Family Physicians) 77 (4): 469–474. ISSN 1532-0650. PMID 18326165. http://www.aafp.org/afp/2008/0215/p469.html. Retrieved August 5, 2010.
- ^ Atkin NB, Baker MC (December 1982). "Specific chromosome change, i(12p), in testicular tumours?". Lancet 2 (8311): 1349. PMID 6128640.
- ^ Bonin, S; Petrera, F; Rosai, J; Stanta, G (2011-09-29). "DNA and RNA obtained from Bouin's fixed tissues". Journal of clinical pathology (Journal of Clinical Pathology) 58 (3): 313–6. doi:10.1136/jcp.2004.016477. PMC 1770606. PMID 15735167. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1770606.
- ^ "Lectin-binding sites in normal human testis?". cancer.org. Journal of Clinical Pathology. 2011-09-29. http://www.ncbi.nlm.nih.gov/pubmed/2469362/. Retrieved 29 September 2011.
- ^ http://www.cancerstaging.org/cstage/CSPart1Manual.pdf
- ^ "Testicular Cancer Resource Center's Staging Page". http://tcrc.acor.org/staging.html. Retrieved 2007-12-13.
- ^ "How is testicular cancer staged?". cancer.org. American Cancer Society. 2011-01-19. http://www.cancer.org/Cancer/TesticularCancer/DetailedGuide/testicular-cancer-staging. Retrieved 12 July 2011.
- ^ UK testicular cancer survival statistics - Cancer Research UK websites
- ^ "Testicular Cancer Treatment (PDQ)". National Cancer Institute. 2009-01-15. http://www.cancer.gov/cancertopics/pdq/treatment/testicular/HealthProfessional/page8. Retrieved 2009-02-13.
- ^ http://www.mrc.ac.uk/Newspublications/News/MRC001863
- ^ Peckham, MJ; Barrett, A; Liew, KH; Horwich, A; Robinson, B; Dobbs, HJ; McElwain, TJ; Hendry, WF (1983). "The treatment of metastatic germ-cell testicular tumours with bleomycin, etoposide and cisplatin (BEP).". British Journal of Cancer 47: 613–619. PMC 2011384. PMID 6189504. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2011384.
- ^ "Chemotherapy - BEP and EP". http://www.tc-library.com/chemotherapy-bep-and-ep/. Retrieved 2009-02-16.
- ^ Huang, William C. (June 5, 2008). "Book Review: Urological Oncology". The New England Journal of Medicine (Massachusetts Medical Society) 358 (23): 2527. doi:10.1056/NEJMbkrev59744. ISSN 1533-4406. http://www.nejm.org/doi/full/10.1056/NEJMbkrev59744. Retrieved August 9, 2010.
- ^ Krege, S.; Beyer, J.; Souchon, R.; Albers, P.; Albrecht, W.; Algaba, F.; et al., Michael; Bodrogi, István et al. (2008). "European consensus conference on diagnosis and treatment of germ cell cancer: a report of the second meeting of the European Germ Cell Cancer Consensus group (EGCCCG): part I". European Urology 53 (3): 478–496. doi:10.1016/j.eururo.2007.12.024. PMID 18191324.
- ^ Rustin, G. J.; Mead, G. M.; Stenning, S. P.; Vasey, P. A.; Aass, N.; Huddart, R. A.; et al., M. P.; Joffe, J. K. et al. (2007). "Randomized trial of two or five computed tomography scans in the surveillance of patients with stage I nonseminomatous germ cell tumors of the testis: Medical Research Council Trial TE08; ISRCTN56475197—the National Cancer Research Institute Testis Cancer Clinical Studies Group". JCO 25 (11): 1310–1315. doi:10.1200/JCO.2006.08.4889.
- ^ http://www.cancerhelp.org.uk/trials/a-trial-to-find-the-best-way-of-using-scans-to-monitor-men-after-treatment-for-seminoma-testicular-cancer
- ^ http://www.ctu.mrc.ac.uk/research_areas/study_details.aspx?s=40
- ^ http://www.fda.gov/fdac/features/196_test.html
- ^ "Cancer of the testicle Causes - Health encyclopaedia - NHS Direct". Archived from the original on 2007-12-10. http://web.archive.org/web/20071210081436/http://www.nhsdirect.nhs.uk/articles/article.aspx?articleId=85§ionId=5. Retrieved 2007-12-13.
- ^ Leendert H. J. Looijenga; J. Wolter Oosterhuis (May 1999). "Pathogenesis of testicular germ cell tumours" (PDF). Rev. Reprod. 4 (2): 90–100. doi:10.1530/ror.0.0040090. ISSN 1359-6004. PMID 10357096. http://ror.reproduction-online.org/cgi/reprint/4/2/90.
- ^ Holmes L; Escalante C, Garrison O, Foldi BX, Ogungbade GO, Essien EJ, Ward D (September 2008). "Testicular cancer incidence trends in the United States (1975−2004): Plateau or shifting racial paradigm?". Public Health 122 (9): 862–872. doi:10.1016/j.puhe.2007.10.010. PMC 2551560. PMID 18555499. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2551560.
- ^ Forman, D; M C Pike, G Davey, S Dawson, K Baker, C E D Chilvers, R T D Oliver, C A C Coupland (28 May 1994). "Aetiology of testicular cancer: association with congenital abnormalities, age at puberty, infertility, and exercise. United Kingdom Testicular Cancer Study Group". BMJ 308 (6941): 1393–9. PMC 2540340. PMID 7912596. http://www.bmj.com/cgi/content/full/308/6941/1393.
- ^ Swerdlow, AJ; Huttly SR, Smith PG. (January 1987). "Testicular cancer and antecedent diseases". Br. J. Cancer 55 (1): 97–103. doi:10.1038/bjc.1987.20. PMC 2001571. PMID 2880604. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2001571.
- ^ Jones, T. C., R. D. Hunt, and N. W. King (1997). Veterinary pathology (6th ed.). Wiley-Blackwell. p. 1210. ISBN 0683044818, 9780683044812. http://books.google.com/?id=8fXzJrDfFgUC.
External links
- Testicular Cancer: Survival High with Early Treatment
- National Institute of Health information and links
- Testicular Cancer Resource Center
- Testicular Cancer symptoms
- Understanding Testicular Cancer from The Cancer Council Australia
- Testicular Cancer at UK NHS
- UK testicular cancer statistics from Cancer Research UK
Tumors: male urogenital neoplasia · genital neoplasia (C60–C63/D29, 185–187/222) Internal TesticlesSex cord-gonadal stromalSertoli-Leydig cell tumour (Sertoli cell tumor, Leydig cell tumor)Embryonal carcinoma · Endodermal sinus tumor · Gonadoblastoma · Teratoma · Choriocarcinoma · EmbryomaExternal PenisCarcinoma (Extramammary Paget's disease) · Bowen's disease · Bowenoid papulosis · Erythroplasia of Queyrat · Hirsuties papillaris genitalisCategories:- Testicle disorders
Wikimedia Foundation. 2010.


