- Pelvic pain
-
Pelvic and perineal pain
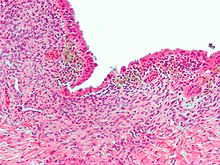
Micrograph showing endometriosis (H&E stain), a common cause of chronic pelvic pain in women.ICD-10 R10..2 ICD-9 625.9, 789.00 MeSH D017699 Pelvic pain is a symptom that can affect both women and men. The pelvic pain that persists for a period of 3 months or more to be considered chronic while less than this duration is considered acute. The pain may indicate the existence of poorly-understood conditions that likely represent abnormal psychoneuromuscular function. Differentiating between acute and chronic pain is important in understanding chronic pelvic pain syndromes. Acute pain is most common, often experienced by patients after surgery or other soft tissue traumas. It tends to be immediate, severe and short lived however, pain that extends beyond a normal recovery period and lasts longer than 3–6 months constitutes chronic pain.[1]
Contents
Female
Most women, at some time in their lives, experience pelvic pain. As girls enter puberty, pelvic or abdominal pain becomes a frequent complaint.
Chronic pelvic pain (CPP) accounts for 10% of all visits to gynecologists. In addition, CPP is the reason for 20—30% of all laparoscopies in adults.[citation needed]
Cause
Many different conditions can cause pelvic pain including:
- exaggerated bladder, bowel, or uterine pain sensitivity (also known as visceral pain)
- pelvic girdle pain (SPD or DSP)
- Gynecologic
- Dysmenorrhea—pain during the menstrual period
- Endometriosis—pain caused by uterine tissue that is outside the uterus
- Müllerian abnormalities
- Pelvic inflammatory disease—pain caused by damage from infections
- Ovarian cysts—the ovary produces a large, painful cyst, which may rupture
- Ovarian torsion—the ovary is twisted in a way that interferes with its blood supply
- Ectopic pregnancy—a pregnancy implanted outside the uterus
- Abdominal
- Loin pain hematuria syndrome
- Proctitis—infection or inflammation of the anus or rectum
- Colitis—infection or inflammation of the colon
- Appendicitis—infection or inflammation of the bowel
Internal hernias are difficult to identify in women, and misdiagnosis with endometriosis or idiopathic chronic pelvic pain is very common. One cause of misdiagnosis that when the woman lies down flat on an examination table, all of the medical signs of the hernia disappear. The hernia can typically only be detected when symptoms are present, so diagnosis requires positioning the woman's body in a way that provokes symptoms.[2]
Workup
The diagnostic workup begins with a careful history and examination, followed by a pregnancy test. Some women may also need bloodwork or additional imaging studies, and a handful may also benefit from having surgical evaluation.
The absence of visible pathology in chronic pain syndromes should not form the basis for either seeking psychological explanations or questioning the reality of the patient’s pain. Instead it is essential to approach the complexity of chronic pain from a psychophysiological perspective which recognises the importance of the mind-body interaction. Some of the mechanisms by which the limbic system impacts on pain, and in particular myofascial pain, have been clarified by research findings in neurology and psychophysiology.[1]
Treatment
Many women will benefit from a consultation with a physical therapist, a trial of anti-inflammatory medications, hormonal therapy, or even neurological agents.
A hysterectomy is sometimes performed.[3]
Male
Chronic pelvic pain in men is referred to as Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) and is also known as chronic nonbacterial prostatitis. Men in this category have no known infection, but do have extensive pelvic pain lasting more than 3 months.[4] There are no standard diagnostic tests; diagnosis is by exclusion of other disease entities. Multimodal therapy is the most successful treatment option,[5] and includes α-blockers,[6] phytotherapy,[7][8] and protocols aimed at quieting the pelvic nerves through myofascial trigger point release with psychological re-training for anxiety control.[9][10] Antibiotics are not recommended.[11][12]
Differential diagnosis
In men, chronic pelvic pain (category IIIB) is often misdiagnosed as chronic bacterial prostatitis and needlessly treated with antibiotics exposing the patient to inappropriate antibiotic use and unnecessarily to adverse effects with little if any benefit in most cases. Within a Bulgarian study, where by definition all patients had negative microbiological results, a 65% adverse drug reaction rate was found for patients treated with ciprofloxacin in comparison to a 9% rate for the placebo patients. This was combined with a higher cure rate (69% v 53%) found within the placebo group.[13]
Epidemiology
Chronic pelvic pain is a common condition with rate of dysmenorrhoea between 16.8—81%, dyspareunia between 8—21.8%, and noncyclical pain between 2.1—24%.[14]
References
- ^ a b Marek Jantos (2007). "Understanding Chronic Pelvic Pain". Pelviperineology 26 (2): 66–69. http://www.pelviperineology.org/practical/chronic_pelvic_pain.html.
- ^ Brody, Jane E. "In women, hernias may be hidden agony" The St. Louis Post-Dispatch. 18 May 2011.
- ^ Kuppermann M, Learman LA, Schembri M, et al. (March 2010). "Predictors of hysterectomy use and satisfaction". Obstet Gynecol 115 (3): 543–51. doi:10.1097/AOG.0b013e3181cf46a0. PMID 20177285.
- ^ Luzzi GA (2002). "Chronic prostatitis and chronic pelvic pain in men: aetiology, diagnosis and management". Journal of the European Academy of Dermatology and Venereology : JEADV 16 (3): 253–6. doi:10.1046/j.1468-3083.2002.00481.x. PMID 12195565.
- ^ Potts JM (2005). "Therapeutic options for chronic prostatitis/chronic pelvic pain syndrome". Current urology reports 6 (4): 313–7. doi:10.1007/s11934-005-0030-5. PMID 15978236.
- ^ Yang G, Wei Q, Li H, Yang Y, Zhang S, Dong Q (2006). "The effect of alpha-adrenergic antagonists in chronic prostatitis/chronic pelvic pain syndrome: a meta-analysis of randomized controlled trials". J. Androl. 27 (6): 847–52. doi:10.2164/jandrol.106.000661. PMID 16870951. "...treatment duration should be long enough (more than 3 months)"
- ^ Shoskes DA, Zeitlin SI, Shahed A, Rajfer J (1999). "Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial". Urology 54 (6): 960–3. doi:10.1016/S0090-4295(99)00358-1. PMID 10604689.
- ^ Elist J (2006). "Effects of pollen extract preparation Prostat/Poltit on lower urinary tract symptoms in patients with chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a randomized, double-blind, placebo-controlled study". Urology 67 (1): 60–3. doi:10.1016/j.urology.2005.07.035. PMID 16413333.
- ^ Anderson RU, Wise D, Sawyer T, Chan C (2005). "Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men". J. Urol. 174 (1): 155–60. doi:10.1097/01.ju.0000161609.31185.d5. PMID 15947608.
- ^ Anderson RU, Wise D, Sawyer T, Chan CA (2006). "Sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome: improvement after trigger point release and paradoxical relaxation training". J. Urol. 176 (4 Pt 1): 1534–8; discussion 1538–9. doi:10.1016/j.juro.2006.06.010. PMID 16952676.
- ^ Alexander RB, Propert KJ, Schaeffer AJ, et al. (2004). "Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial". Ann. Intern. Med. 141 (8): 581–9. PMID 15492337.
- ^ Nickel JC, Downey J, Clark J, et al. (2003). "Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial". Urology 62 (4): 614–7. doi:10.1016/S0090-4295(03)00583-1. PMID 14550427.
- ^ J. Dimitrakov; J. Tchitalov, T. Zlatanov, D. Dikov. "A Prospective, Randomized, Double-Blind, Placebo-Controlled Study Of Antibiotics For The Treatment Of Category Iiib Chronic Pelvic Pain Syndrome In Men". Third International Chronic Prostatitis Network. http://www.prostatitis.org/a92000.html. Retrieved 4 September 2009. "The results of our study show that antibiotics have an unacceptably high rate of adverse side effects as well as a statistically insignificant improvement over placebo..."
- ^ Latthe P, Latthe M, Say L, Gülmezoglu M, Khan KS (2006). "WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity". BMC Public Health 6: 177. doi:10.1186/1471-2458-6-177. PMC 1550236. PMID 16824213. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1550236.
External links
- Pelvic Pain Support Network
- International Pelvic Pain Society
- American Pain Society
- University of Michigan Pelvic Pain Program
- University of North Carolina Pelvic Pain Program
- Tailbone pain (coccyx pain, coccydynia): Free medical article online at eMedicine
- Pelviperineology The multidisciplinary open access pelvic floor journal
Symptoms and signs: digestive system and abdomen (R10–R19, 787,789) GI tract Upper GI tractAccessory Abdominopelvic Abdominal – general Pain and nociception By region/system HEENTCardiovascular systemMusculoskeletalNeurologicCongenital insensitivity to pain · HSAN (Type I, II congenital sensory neuropathy, III familial dysautonomia, IV congenital insensitivity to pain with anhidrosis, V congenital insensitivity to pain with partial anhidrosis) · Neuralgia · Pain asymbolia · Pain disorder · Paroxysmal extreme pain disorder · Allodynia · Chronic pain · Hyperalgesia · Hypoalgesia · Hyperpathia · Phantom pain · Referred painUrogenitalGastrointestinalProctalgiaTests Related concepts Female diseases of the pelvis and genitals (N70–N99, 614–629) Internal AdnexaOophoritis · Ovarian cyst (Follicular cyst of ovary, Corpus luteum cyst, Theca lutein cyst) · Endometriosis of ovary · Ovarian hyperstimulation syndrome · Ovarian torsion · Ovarian apoplexy · Mittelschmerz · Female infertility (Anovulation, Poor ovarian reserve)Cervicitis · Cervical polyp · Nabothian cyst · Cervical incompetence · Female infertility (Cervical stenosis) · Cervical dysplasiaGeneralVaginitis (Bacterial vaginosis, Atrophic vaginitis, Candidal vulvovaginitis) · Leukorrhea/Vaginal discharge · Hematocolpos/HydrocolposOther/generalExternal Categories:- Gynaecology
- Nociception
- Chronic pain syndromes
Wikimedia Foundation. 2010.