- B-cell lymphoma
-
B-cell lymphoma Classification and external resources 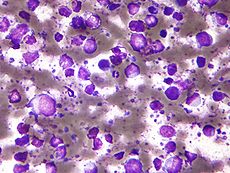
Micrograph showing a large B cell lymphoma. Field stain.ICD-10 C85.1 ICD-O: 9680/0, 9699/3, 9699/3 eMedicine med/1358 MeSH D016393 The B-cell lymphomas are types of lymphoma affecting B cells. Lymphomas are "blood cancers" in the lymph glands. They develop more frequently in older adults and in immunocompromised individuals (such as those with AIDS).
B-cell lymphomas include both Hodgkin's lymphomas and most non-Hodgkins lymphomas. They are often divided into indolent (slow-growing) lymphomas and aggressive lymphomas. Indolent lymphomas respond rapidly to treatment and are kept under control (in remission) with long-term survival of many years, but are not cured. Aggressive lymphomas usually require intensive treatments, but have good prospects for a permanent cure.[1]
Prognosis and treatment depends on the specific type of lymphoma as well as the stage and grade. Treatment includes radiation and chemotherapy. Early-stage indolent B-cell lymphomas can often be treated with radiation alone, with long-term non-reoccurrence. Early-stage aggressive disease is treated with chemotherapy and often radiation, with a 70-90% cure rate.[1] Late-stage indolent lymphomas are sometimes left untreated and monitored until they progress. Late-stage aggressive disease is treated with chemotherapy, with cure rates of over 70%.[1]
Contents
Types
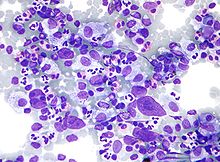 Micrograph showing Hodgkin lymphoma, a type of B cell lymphoma that is usually considered separate from other B cell lymphomas. Field stain.
Micrograph showing Hodgkin lymphoma, a type of B cell lymphoma that is usually considered separate from other B cell lymphomas. Field stain.
There are fourteen kinds of lymphomas involving B cells.
Common
Five account for nearly three out of four patients with non-Hodgkin lymphoma:[2]
- Diffuse large B cell lymphoma[3]
- Follicular lymphoma
- Mucosa-Associated Lymphatic Tissue lymphoma (MALT)
- Small cell lymphocytic lymphoma (overlaps with Chronic lymphocytic leukemia)
- Mantle cell lymphoma (MCL)
Rare
The remaining nine are much less common:[2]
- Burkitt lymphoma
- Mediastinal large B cell lymphoma
- Waldenström macroglobulinemia
- Nodal marginal zone B cell lymphoma (NMZL)
- Splenic marginal zone lymphoma (SMZL)
- Intravascular large B-cell lymphoma
- Primary effusion lymphoma
- Lymphomatoid granulomatosis
Other
Additionally, some researchers separate out lymphomas that appear result from other immune system disorders, such as AIDS-related lymphoma.
Classic Hodgkin's lymphoma and nodular lymphocyte predominant Hodgkin's lymphoma are now considered forms of B-cell lymphoma.[4]
Associated chromosomal translocations
Chromosomal translocations involving the immunoglobulin heavy locus (IGH@) is a classic cytogenetic abnormality for many B-cell lymphomas, including follicular lymphoma, mantle cell lymphoma and Burkitt's lymphoma. In these cases, The immunoglobulin heavy locus forms a fusion protein with another protein that has pro-proliferative or anti-apoptotic abilities. The enhancer element of the immunoglobulin heavy locus, which normally functions to make B cells produce massive production of antibodies, now induces massive transcription of the fusion protein, resulting in excessive pro-proliferative or anti-apoptotic effects on the B cells containing the fusion protein. In Burkitt's lymphoma and mantle cell lymphoma, the other protein in the fusion is c-myc (on chromosome 8) and cyclin D1[5] (on chromosome 11), respectively, which gives the fusion protein pro-proliferative ability. In follicular lymphoma, the fused protein is Bcl-2 (on chromosome 18), which gives the fusion protein anti-apoptotic abilities.
See also
References
- ^ a b c Merck Manual home edition, Non-Hodgkin Lymphomas
- ^ a b "The Lymphomas" (PDF). The Leukemia & Lymphoma Society. May 2006. p. 12. http://www.leukemia-lymphoma.org/attachments/National/br_1161891669.pdf. Retrieved 2008-04-07.
- ^ Mazen Sanoufa, Mohammad Sami Walid, Talat Parveen (2010). "B-Cell Lymphoma of the Thoracic Spine Presenting with Spinal Cord Pressure Syndrome". JOCMR 2 (1): 53–54. doi:10.4021/jocmr2010.02.258w.
- ^ "HMDS: Hodgkin's Lymphoma". http://www.hmds.org.uk/hl.html. Retrieved 2009-02-01.
- ^ Li JY, Gaillard F, Moreau A, et al. (May 1999). "Detection of translocation t(11;14)(q13;q32) in mantle cell lymphoma by fluorescence in situ hybridization". Am. J. Pathol. 154 (5): 1449–52. doi:10.1016/S0002-9440(10)65399-0. PMC 1866594. PMID 10329598. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1866594.
External links
- Overview and video at harvard.edu
- Lymphoma Association – Specialist UK charity providing free information and support to patients, their families, friends and carers
Hematological malignancy/leukemia histology (ICD-O 9590–9989, C81–C96, 200–208)
Lymphoid/Lymphoproliferative, Lymphomas/Lymphoid leukemias (9590–9739, 9800–9839)By development/
markerALL (Precursor B acute lymphoblastic leukemia/lymphoma)CD5+CD22+germinal center/follicular B cell (Follicular, Burkitt's, GCB DLBCL, Primary cutaneous follicular lymphoma)marginal zone/marginal-zone B cell (Splenic marginal zone, MALT, Nodal marginal zone, Primary cutaneous marginal zone lymphoma)see immunoproliferative immunoglobulin disordersBy infectionDiffuse large B-cell lymphoma · Intravascular large B-cell lymphoma · Primary cutaneous marginal zone lymphoma · Primary cutaneous immunocytoma · Plasmacytoma · Plasmacytosis · Primary cutaneous follicular lymphomaBy development/
markerTdT+: ALL (Precursor T acute lymphoblastic leukemia/lymphoma)
prolymphocyte (Prolymphocytic)
CD30+ (Anaplastic large-cell lymphoma, Lymphomatoid papulosis type A)indolent: Mycosis fungoides · Pagetoid reticulosis · Granulomatous slack skin
aggressive: Sézary's disease · Adult T-cell leukemia/lymphomaNon-MFCD30-: Non-mycosis fungoides CD30− cutaneous large T-cell lymphoma · Pleomorphic T-cell lymphoma · Lymphomatoid papulosis type B
CD30+: CD30+ cutaneous T-cell lymphoma · Secondary cutaneous CD30+ large cell lymphoma · Lymphomatoid papulosis type AOther peripheralHepatosplenic · Angioimmunoblastic · Enteropathy-associated T-cell lymphoma · Peripheral T-cell lymphoma-Not-Otherwise-Specified (Lennert lymphoma) · Subcutaneous T-cell lymphomaBy infectionHTLV-1 (Adult T-cell leukemia/lymphoma)NK cell/
(most CD56)Aggressive NK-cell leukemia · Blastic NK cell lymphomaT or NKLymphoid+myeloidCutaneous lymphoid hyperplasia Cutaneous lymphoid hyperplasia with bandlike and perivascular patterns · Cutaneous lymphoid hyperplasia with nodular pattern · Jessner lymphocytic infiltrate of the skinCategories:
Wikimedia Foundation. 2010.
