- Monocyte
-
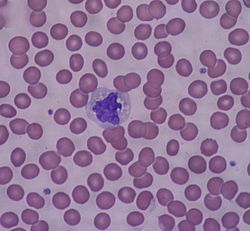
Monocyte Monocyte under a light microscope (40x) from a peripheral blood smear surrounded by red blood cells. Latin monocytus Code TH H2.00.04.1.02010 Monocytes are a type of white blood cell and are part of the innate immune system of vertebrates including all mammals (including humans), birds, reptiles, and fish. Monocytes play multiple roles in immune function. Such roles include: (1) replenish resident macrophages and dendritic cells under normal states, and (2) in response to inflammation signals, monocytes can move quickly (approx. 8-12 hours) to sites of infection in the tissues and divide/differentiate into macrophages and dendritic cells to elicit an immune response. Half of them are stored in the spleen.[1] Monocytes are usually identified in stained smears by their large kidney shaped or notched nucleus.
Contents
Physiology
 Monocyte
Monocyte
Monocytes are produced by the bone marrow from haematopoietic stem cell precursors called monoblasts. Monocytes circulate in the bloodstream for about one to three days and then typically move into tissues throughout the body. They constitute between three to eight percent of the leukocytes in the blood. Half of them are stored as a reserve in the spleen in clusters in the red pulp's Cords of Billroth.[1] In the tissues monocytes mature into different types of macrophages at different anatomical locations. Monocyte is the largest corpuscle in the blood.
Monocytes which migrate from the bloodstream to other tissues will then differentiate into tissue resident macrophages or dendritic cells. Macrophages are responsible for protecting tissues from foreign substances but are also suspected to be important in the formation of important organs like the heart, brain. They are cells that possess a large smooth nucleus, a large area of cytoplasm and many internal vesicles for processing foreign material.
Monocytes and their macrophage and dendritic-cell progeny serve three main functions in the immune system. These are phagocytosis, antigen presentation and cytokine production. Phagocytosis is the process of uptake of microbes and particles followed by digestion and destruction of this material. Monocytes can perform phagocytosis using intermediary (opsonising) proteins such as antibodies or complement that coat the pathogen, as well as by binding to the microbe directly via pattern-recognition receptors that recognize pathogens. Monocytes are also capable of killing infected host cells via antibody, termed antibody-mediated cellular cytotoxicity. Vacuolization may be present in a cell that has recently phagocytized foreign matter.
Microbial fragments that remain after such digestion can serve as antigen. The fragments can be incorporated into MHC molecules and then traffic to the cell surface of monocytes (and macrophages and dendritic cells). This process is called antigen presentation and it leads to activation of T lymphocytes, which then mount a specific immune response against the antigen.
Other microbial products can directly activate monocytes and this leads to production of pro-inflammatory and with some delay of anti-inflammatory cytokines. Typical cytokines produced by monocytes are TNF tumor necrosis factor, IL-1 interleukin-1 and IL-12 interleukin-12.
Monocyte subpopulations
There are at least three types of monocytes in human blood [2]:
a) the classical monocyte is characterized by high level expression of the CD14 cell surface receptor (CD14++ CD16- monocyte)
b) the non-classical monocyte shows low level expression of CD14 and with additional co-expression of the CD16 receptor (CD14+CD16++ monocyte).[3]
c) the intermediate monocyte with high level expression of CD14 and low level expression of CD16 (CD14++CD16+ monocytes).
There appears to be a developmental relationship in that the classical monocytes develop into the intermediate monocytes to then become the non-classical monocytes CD14+CD16+ monocytes. Hence the non-classical monocytes may represent a more mature version. After stimulation with microbial products the CD14+CD16++ monocytes produce high amounts of pro-inflammatory cytokines like tumor necrosis factor and interleukin-12. Said et al. showed that activated monocytes express high levels of PD-1 which might explain the higher expression of PD-1 in CD14+CD16+ monocytes as compared to CD14+CD16- monocytes. Triggering monocytes-expressed PD-1 by its ligand PD-L1 induces IL-10 production which inhibits CD4 T-cell function.[4]
Diagnostic use
 A scanning electron microscope (SEM) image of normal circulating human blood. One can see red blood cells, several knobby white blood cells including lymphocytes, a monocyte, a neutrophil, and many small disc-shaped platelets.
A scanning electron microscope (SEM) image of normal circulating human blood. One can see red blood cells, several knobby white blood cells including lymphocytes, a monocyte, a neutrophil, and many small disc-shaped platelets.
A monocyte count is part of a complete blood count and is expressed either as a ratio of monocytes to the total number of white blood cells counted, or by absolute numbers. Both may be useful in determining or refuting a possible diagnosis.
Monocytosis
Monocytosis is the state of excess monocytes in the peripheral blood. It may be indicative of various disease states. Examples of processes that can increase a monocyte count include:
- chronic inflammation
- stress response
- hyperadrenocorticism
- immune-mediated disease
- pyogranulomatous disease
- necrosis
- red cell regeneration
- Viral Fever
- sarcoidosis
A high count of CD14+CD16+ monocytes is found in severe infection (sepsis)[5] and a very low count of these cells is found after therapy with immuno-suppressive glucocorticoids[6]
Monocytopenia
Monocytopenia is a form of leukopenia associated with a deficiency of monocytes.
Dendritic cells
Monocytes can be used to generate dendritic cells in vitro by adding cytokines like Granulocyte Monocyte Colony Stimulating Factor (GMCSF) and IL-4. [7]
Blood content
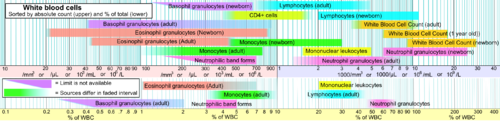 Reference ranges for blood tests of white blood cells, comparing monocyte amount (shown in green) with other cells.
Reference ranges for blood tests of white blood cells, comparing monocyte amount (shown in green) with other cells.
See also
References
- ^ a b Swirski FK, Nahrendorf M, Etzrodt M, Wildgruber M, Cortez-Retamozo V, Panizzi P, Figueiredo J-L, Kohler RH, Chudnovskiy A, Waterman P, Aikawa E, Mempel TR, Libby P, Weissleder R, Pittet MJ. (2009). Identification of Splenic Reservoir Monocytes and Their Deployment to Inflammatory Sites. Science, 325: 612-616. doi:10.1126/science.1175202 PMID 19644120
- ^ Ziegler-Heitbrock, L et al: Nomenclature of monocytes and dendritic cells. Blood, Epub ahead of print
- ^ Ziegler-Heitbrock, L: The CD14+ CD16+ Blood Monocytes: their Role in Infection and Inflammation, Review. J Leukocyte Biology, 81:584, 2007
- ^ Elias A. Said et al. 2009, PD-1 Induced IL10 Production by Monocytes Impairs T-cell Activation in a Reversible Fashion. Nature Medicine. 2010; 452-9.
- ^ Fingerle, G., Pforte, A., Passlick, B., Blumenstein, M., Ströbel, M., Ziegler-Heitbrock, H.W.L.: The novel subset of CD14+ CD16+ blood monocytes is expanded in sepsis patients. Blood, 82: 3170-3176, 1993
- ^ Fingerle-Rowson, G., Angstwurm, M., Andreesen, R., Ziegler-Heitbrock, H.W.L.:Selective depletion of CD14+ CD16+ monocytes by glucocorticoid therapy.Clin. Exp. Immunol., 112: 501-506, 1998
- ^ Sallusto F, Cella M, Danieli C, Lanzavecchia A (1995). "Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: downregulation by cytokines and bacterial products". J. Exp. Med. 182 (2): 389–400. doi:10.1084/jem.182.2.389. PMC 2192110. PMID 7629501. http://www.jem.org/cgi/reprint/182/2/389.pdf.
External links
Myeloid lineage - Blood (WBC and RBC) Cellular/
HSCsCFU-GMHistiocytes · Kupffer cells · Alveolar macrophage · Microglia · Osteoclasts · Epithelioid cells · giant cells (Langhans giant cells, Foreign-body giant cell, Touton giant cells)CFU-DLCommonCFU-BasoCFU-EosCFU-MegCFU-ECFU-MastNoncellular Immunology: Lymphocytic adaptive immune system and complement Lymphoid AntigensAntibodiesImmunity vs.
toleranceaction: Immunity · Autoimmunity · Alloimmunity · Allergy · Hypersensitivity · Inflammation · Cross-reactivity
inaction: Tolerance (Central, Peripheral, Clonal anergy, Clonal deletion, Tolerance in pregnancy) · ImmunodeficiencyLymphocytes Substances Complement Categories:- Mononuclear phagocytes
- Cell biology
- Human cells
Wikimedia Foundation. 2010.