- Invasiveness of surgical procedures
-
"Invasive (medical)" redirects here. For "invasive" as related to abnormal tissue growth, see Cancer.
There are three main categories which describe the invasiveness of surgical procedures. These are: non-invasive procedures, minimally invasive procedures, and invasive procedures (the latter of which may also be called open surgery).
Contents
Non-invasive procedure
A medical procedure is strictly defined as non-invasive when no break in the skin is created and there is no contact with the mucosa, or skin break, or internal body cavity beyond a natural or artificial body orifice. For example deep palpation and percussion is non-invasive but a rectal examination is invasive. Similarly, examination of the ear-drum or inside the nose or a wound dressing change all fall outside the strict definition of non-invasive procedure. There are many non-invasive procedures, ranging from simple observation, to specialised forms of surgery, such as radiosurgery.
For centuries, physicians have employed many simple non-invasive methods based on physical parameters in order to assess body function in health and disease (physical examination and inspection), such as pulse-taking, the auscultation of heart sounds and lung sounds (using the stethoscope), temperature examination (using thermometers), respiratory examination, peripheral vascular examination, oral examination[disambiguation needed
 ], abdominal examination, external percussion and palpation, blood pressure measurement (using the sphygmomanometer), change in body volumes (using plethysmograph), audiometry, eye examination and many others.
], abdominal examination, external percussion and palpation, blood pressure measurement (using the sphygmomanometer), change in body volumes (using plethysmograph), audiometry, eye examination and many others.The discovery of the first modern non-invasive techniques based on physical methods, electrocardiography and X-rays, dates back to the end of the 19th century. Since then, non-invasive methods – which penetrate the body nonetheless, but by electromagnetic or particle radiation rather than a scalpel – have continuously enlarged the scope of medical technology. Non-invasive techniques commonly used for diagnosis and therapy include the following:
Diagnostic images
- Bioluminescence imaging
- Dermatoscopy
- Diffuse optical tomography
- Gamma camera and other scintillographical methods, such as Positron Emission Tomography (PET) and Single-Photon Emission Tomography (SPECT), using radioactive tracers in the body
- Computed Tomography
- Gene expression imaging
- Infrared imaging of the body
- Magnetic resonance elastography
- Magnetic resonance imaging, using external magnetic fields
- Magnetic resonance spectroscopy
- Optical coherence tomography
- Posturography
- Radiography, fluoroscopy and computed tomography, using X-rays
- Ultrasonography and echocardiography using ultrasound waves for imaging
A recent advance is the substitution of invasive medical tests, such as colonoscopy by computer-based 3D reconstructions, such as virtual colonoscopy.
Diagnostic signals
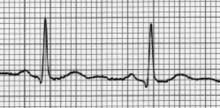
- Electrocardiography (EKG)
- Electroencephalography (EEG)
- Electromyography (EMG)
- Photoplethysmograph(PPG)
- Electrical impedance tomography (EIT)
- Electroneuronography (ENoG)
- Electroretinography (ERG)
- Electronystagmography (ENG)
- Magnetoencephalography (MEG)
- Evoked potentials, such as the visual evoked potentials (VEP) and the brain evoked response audiometry (BERA) tests
- Body impedanciometry
- Impedance phlebography
- Nuclear magnetic resonance spectroscopy
- Percutaneous light spectroscopy (such as in pulse oximetry and capnography)
- Actigraphy
- Breath tests, such as the urea breath test
- Intelligent biomedical clothing
- Non-invasive biomedical sensors
- Endoluminal capsule monitoring
Therapy
- Radiation therapy and radiosurgery, procedures that use external atomic particles (protons, neutrons, photons, alpha particles, etc.) or teletherapy x-rays to destroy pathological tissue within the body (brachytherapy can be non-invasive, minimally invasive, or invasive)
- Lithotripsy, a procedure that uses ultrasound shock waves to break urinary calculus
- Defibrillation, a procedure to block heart fibrillation and start normal rhythm
- Mechanical ventilation, such as the iron lung.
- Transdermal patches, used to deliver drugs applied to the skin.
- Biofeedback
- CPAP (Continuous Positive Airway Pressure) used to treat sleep apnea
- VPAP
- BIPAP
- Neurally Adjusted Ventilatory Assist
- Biphasic Cuirass Ventilation (BCV, e.g. Hayek RTX)
- Photodynamic therapy
- Therapeutic ultrasound
- Extracorporeal thermal ablation
- Extracorporeal magnetic innervation[1]
- Photo-infrared pulsed bio-modulation[2]
- Transcranial magnetic stimulation
In some cases, non-invasive methods will not work for the intended purpose, so medical technology has developed minimally-invasive methods, such as hypodermic injection (using the syringe), endoscopy, percutaneous surgery, laparoscopic surgery, coronary catheterization, angioplasty, stereotactic surgery and many others. The benefits for the patient are self-evident.
Minimally invasive procedure
A minimally invasive procedure is any procedure (surgical or otherwise) that is less invasive than open surgery used for the same purpose. A minimally invasive procedure typically involves use of laparoscopic devices and remote-control manipulation of instruments with indirect observation of the surgical field through an endoscope or similar device, and is carried out through the skin or through a body cavity or anatomical opening. This may result in shorter hospital stays, or allow outpatient treatment.[3] However, the safety and effectiveness of each procedure must be demonstrated with randomized controlled trials. The term was coined by John EA Wickham in 1984, who wrote of it in British Medical Journal in 1987 [4]. A minimally invasive procedure is distinct from a non-invasive procedure, such as external imaging instead of exploratory surgery. When there is minimal damage of biological tissues at the point of entrance of instrument(s), the procedure is called minimally invasive.
Minimal incision technique
Main article: Surgical IncisionsThe minimal incision technique is a specialized surgical technique practiced by some physicians to remove masses or growths with minimal scarring and less recovery time. Most surgeons usually cut along 3/4 to the full length of the mass to access it or remove it. With the minimal incision technique the incision is usually about 1/10 the size of the underlying mass and the surgeon carefully dissects the mass out through this very small incision. A smaller incision forms a much smaller scar and results in less recovery time for the patient. This technique is useful for cysts or lipomas. Patients with such lesions on cosmetically or functionally important areas such as the face can gain great benefit from such techniques.
Specific procedures
Many medical procedures are called minimally invasive, such as hypodermic injection, air-pressure injection, subdermal implants, endoscopy, percutaneous surgery, laparoscopic surgery, arthroscopic surgery, cryosurgery, microsurgery, keyhole surgery, endovascular surgery (such as angioplasty), coronary catheterization, permanent spinal and brain electrodes, stereotactic surgery, The Nuss Procedure, radioactivity-based medical imaging methods, such as gamma camera, Positron emission tomography and SPECT (single photon emission tomography). Related procedures are image-guided surgery, robotic surgery[5] and interventional radiology.
Benefits
Minimally invasive surgery should have less operative trauma for the patient than an equivalent invasive procedure. It may be more or less expensive. Operative time is longer, but hospitalization time is shorter. It causes less pain and scarring, speeds recovery, and reduces the incidence of post-surgical complications, such as adhesions. Some studies have compared heart surgery.[6] However, minimally invasive surgery is not necessarily minor surgery that only regional anesthesia is required. In fact, most of these procedures still requires general anesthesia to be administered beforehand.
Risks
Minimally invasive procedures are not completely safe, and some have complications ranging from infection to death. Risks and complications include the following:
- Anesthesia or medication reactions
- Bleeding
- Infection
- Internal organ injury
- Blood vessel injury
- Vein or lung blood clotting
- Breathing problems
- Death[7]
All of these risks are present also in open, more invasive surgery.
There may be an increased risk of hypothermia and peritoneal trauma due to increased exposure to cold, dry gases during insufflation. The use of heated and humidified CO2 may reduce this risk.[8]
Prevalence
Due to these advantages, surgeons are attempting to perform more procedures as minimally invasive procedures. Some procedures, such as gall bladder removal, can be done very effectively as minimally invasive surgery.[citation needed] Other procedures, such as endarterectomy, have a higher incidence of strokes in some studies.[citation needed] The first successful minimally invasive aortic aneurysm surgery was performed by Dr. Michael L. Marin at Mount Sinai Hospital, New York.[9]
"Lapraroscopic surgery has been around for a long time. We've been using laparoscopy for appendectomies, for taking out gall bladders and for removing cysts on the ovaries. But it's been in very limited use for hysterectomies."[10] Laparoscopic hysterectomy, with incisions measuring less than 10 mm, is used for less than 10% of the roughly 800,000 hysterectomies annually performed in the United States, according to the American Association of Gynecological Laparoscopists (AAGL).
Equipment
Special medical equipment may be used, such as fiber optic cables, miniature video cameras and special surgical instruments handled via tubes inserted into the body through small openings in its surface. The images of the interior of the body are transmitted to an external video monitor and the surgeon has the possibility of making a diagnosis, visually identifying internal features and acting surgically on them.
Open surgery
An invasive procedure is one which penetrates or breaks the skin or enters a body cavity. Examples of invasive procedures include those that involve perforation, an incision, a catheterization, or other entry into the body. Surgery is a typical medical invasive procedure. An open surgery means cutting skin and tissues so the surgeon has a direct access to the structures or organs involved. The structures and tissues involved can be seen and touched, and they are directly exposed to the air of the operating room. Examples of open surgery include the removal of organs, such as the gallbladder (though cholecsytectomy is now mostly done laproscopically) or kidney, and most types of cardiac surgery and neurosurgery. Open surgery involves large incisions, in which the tissues are exposed to the air.
See also
- Anesthesia
- ASA physical status classification system or pre-operative physical fitness
- Endoscopy
- Interventional Radiology
- Laparoscopic surgery
- Medicine
- Natural Orifice Transluminal Endoscopic Surgery
- Surgery
- Traumatology
- Medical imaging
- Biomedical engineering
- Molecular Imaging
- Surgical Incisions
References
- ^ Yokoyama T, Fujita O, Nishiguchi J, et al. (August 2004). "Extracorporeal magnetic innervation treatment for urinary incontinence". International Journal of Urology 11 (8): 602–6. doi:10.1111/j.1442-2042.2004.00857.x. PMID 15285749.
- ^ Santana-Blank LA, Rodríguez-Santana E, Santana-Rodríguez KE (August 2005). "Photo-infrared pulsed bio-modulation (PIPBM): a novel mechanism for the enhancement of physiologically reparative responses". Photomedicine and Laser Surgery 23 (4): 416–24. doi:10.1089/pho.2005.23.416. PMID 16144487.
- ^ NCBI, National Center for Biotechnology Information, NCBI, MeSH, Medical SubHeadings, NLM, National Library of Medicine
- ^ Wickham JE' (December 1987). "The new surgery". Br Med J 295: 1581–1582.
- ^ Ahmed K, Khan MS, Vats A, et al. (October 2009). "Current status of robotic assisted pelvic surgery and future developments". International Journal of Surgery 7 (5): 431–40. doi:10.1016/j.ijsu.2009.08.008. PMID 19735746.
- ^ Kilger E, Weis FC, Goetz AE, et al. (March 2001). "Intensive care after minimally invasive and conventional coronary surgery: a prospective comparison". Intensive Care Medicine 27 (3): 534–9. doi:10.1007/s001340000788. PMID 11355122.
- ^ “Risks and Complications"
- ^ Peng Y, Zheng M, Ye Q, Chen X, Yu B, Liu B (January 2009). "Heated and humidified CO2 prevents hypothermia, peritoneal injury, and intra-abdominal adhesions during prolonged laparoscopic insufflations". The Journal of Surgical Research 151 (1): 40–7. doi:10.1016/j.jss.2008.03.039. PMID 18639246.
- ^ Mount Sinai Hospital In the News
- ^ Warren Volker, OB/GYN MD Minimally Invasive Procedures
Sources
Minimally invasive procedure
- Wickham JEA. The new surgery. Br Med J 1987;29:1581–1582.
- Minimally invasive heart surgery. Medical Encyclopedia, MedlinePlus.
- Minimally invasive aortic valve surgery. CTSNet article.
- Minimally invasive surgery yields benefits. The American Academy of Orthopedic Surgeons. Febr. 2003.
- Minimally invasive cancer treatments highlighted. Science Daily. Nov. 2005.
- Minimal Parathyroid Surgery. The minimally invasive technique utilizing intraoperative nuclear mapping, slso called Minimally Invasive Radioguided Parathyroidectomy, or "MIRP". EndocrineWeb. June 20, 2005.
- Kilger E, Weis FC, Goetz AE, et al. (March 2001). "Intensive care after minimally invasive and conventional coronary surgery: a prospective comparison". Intensive Care Medicine 27 (3): 534–9. doi:10.1007/s001340000788. PMID 11355122.
Non-invasive procedure
- Tachibana K (March 2004). "Emerging technologies in therapeutic ultrasound: thermal ablation to gene delivery". Human Cell 17 (1): 7–15. PMID 15369132.
- Kim PE, Singh M (July 2003). "Functional magnetic resonance imaging for brain mapping in neurosurgery". Neurosurgical Focus 15 (1): E1. doi:10.3171/foc.2003.15.1.1. PMID 15355003.
- Richie RC (2002). "Non-invasive assessment of the risk of coronary heart disease". Journal of Insurance Medicine 34 (1): 31–42. PMID 15303592.
- Golder W (June 2004). "Magnetic resonance spectroscopy in clinical oncology". Onkologie 27 (3): 304–9. doi:10.1159/000077983. PMID 15249722.
- Cherry SR (February 2004). "In vivo molecular and genomic imaging: new challenges for imaging physics". Physics in Medicine and Biology 49 (3): R13–48. doi:10.1088/0031-9155/49/3/R01. PMID 15012005. http://stacks.iop.org/0031-9155/49/R13.
- Lymberis A, Olsson S (2003). "Intelligent biomedical clothing for personal health and disease management: state of the art and future vision". Telemedicine Journal and E-health 9 (4): 379–86. doi:10.1089/153056203772744716. PMID 14980096.
- Söling A, Rainov NG (October 2003). "Bioluminescence imaging in vivo - application to cancer research". Expert Opinion on Biological Therapy 3 (7): 1163–72. doi:10.1517/14712598.3.7.1163. PMID 14519079.
- Rohrscheib M, Robinson R, Eaton RP (September 2003). "Non-invasive glucose sensors and improved informatics--the future of diabetes management". Diabetes, Obesity & Metabolism 5 (5): 280–4. doi:10.1046/j.1463-1326.2003.00275.x. PMID 12940864.
- Jacobs AH, Winkeler A, Dittmar C, Hilker R, Heiss WD (2002). "Prospects of molecular imaging in neurology". Journal of Cellular Biochemistry. Supplement 39: 98–109. doi:10.1002/jcb.10414. PMID 12552609.
- Malhi GS, Valenzuela M, Wen W, Sachdev P (February 2002). "Magnetic resonance spectroscopy and its applications in psychiatry". The Australian and New Zealand Journal of Psychiatry 36 (1): 31–43. doi:10.1046/j.1440-1614.2002.00992.x. PMID 11929436.
- Jacobs A, Heiss WD (April 2002). "Towards non-invasive imaging of HSV-1 vector-mediated gene expression by positron emission tomography". Veterinary Microbiology 86 (1-2): 27–36. doi:10.1016/S0378-1135(01)00488-6. PMID 11888687.
- Leman JA, Morton CA (January 2002). "Photodynamic therapy: applications in dermatology". Expert Opinion on Biological Therapy 2 (1): 45–53. doi:10.1517/14712598.2.1.45. PMID 11772339.
- Richter JE (November 1997). "Ambulatory esophageal pH monitoring". The American Journal of Medicine 103 (5A): 130S–134S. doi:10.1016/S0002-9343(97)00338-0. PMID 9422638.
- Yokoyama T, Fujita O, Nishiguchi J, et al. (August 2004). "Extracorporeal magnetic innervation treatment for urinary incontinence". International Journal of Urology 11 (8): 602–6. doi:10.1111/j.1442-2042.2004.00857.x. PMID 15285749.
Categories:- Medical terms
- Surgery
Wikimedia Foundation. 2010.