- Pituitary adenoma
-
Pituitary adenoma Classification and external resources ICD-10 D35.2 ICD-9 237.0 ICD-O: M8140/0 MedlinePlus 000704 eMedicine neuro/312 MeSH D010911 Pituitary adenomas are tumors that occur in the pituitary gland, and account for about 15% of intracranial neoplasms. They often remain undiagnosed, and small pituitary tumors have an estimated prevalence of 16.7% (14.4% in autopsy studies and 22.5% in radiologic studies).[1][2]
Contents
Types
Pituitary tumors were, historically, classed as basophilic, acidophilic, or chromophobic on the basis of whether or not they took up the stains hematoxylin and eosin. This classification has fallen into disuse, in favor of a classification based on what type of hormone is secreted by the tumor (though tumors which do not secrete any active hormone ("non-functioning tumors") are still sometimes called "chromophobic").
At present, classification of pituitary tumors is based on plasma hormone levels or immunohistochemical staining, as given in table below. The "Percentage of hormone production cases" values are the fractions of adenomas producing each related hormone of each tumor type as compared to all cases of pituitary tumors, and does not directly correlate to the percentages of each tumor type because of smaller or greater incidences of absence of secretion of the expected hormone. Thus, nonsecretive adenomas may be either null cell adenomas or a more specific adenoma that, however, remains nonsecretive.
Type of adenoma Secretion Staining Pathology Percentage of hormone production cases lactotrophic adenomas or prolactinomas (most common) secrete prolactin acidophilic galactorrhea, hypogonadism, amenorrhea, infertility, and impotence 30%[3] somatotrophic adenomas secrete growth hormone (GH) acidophilic acromegaly (gigantism) 15%[3] corticotrophic adenomas secrete adenocorticotropic hormone (ACTH) basophilic Cushing's disease gonadotrophic adenomas secrete luteinizing hormone (LH), follicle-stimulating hormone (FSH) and their subunits basophilic usually doesn't cause symptoms 10%[3] thyrotrophic adenomas (rare) secrete thyroid-stimulating hormone (TSH) basophilic to chromophobic occasionally hyperthyroidism,[4] usually doesn't cause symptoms Less than 1%[3] null cell adenomas do not secrete hormones may stain positive for synaptophysin 25% of pituitary adenomas are nonsecretive[3] Pituitary incidentalomas
Pituitary incidentalomas are pituitary tumors that are characterized as an incidental finding. They are often discovered by computed tomography (CT) or MRI performed in the evaluation of unrelated medical conditions such as suspected head trauma, cancer staging or in the evaluation of nonspecific symptoms such as dizziness and headache. It is not uncommon for them to be discovered at autopsy. In a meta-analysis, adenomas were found in an average of 16.7% in postmortem studies, with most being microadenomas (<10mm); macrodenomas accounted for only 0.16% to 0.2% of the decedents.[5]While pituitary microadenomas are generally considered benign the presence of a microadenoma has been positively identified as a risk factor for suicide in a postmortem study of suicide victims.[6][7]
Symptoms
Hormone secreting pituitary adenomas cause one of several forms of hyperpituitarism. The specifics depend on the type of hormone. Some tumors secrete more than one hormone, the most common combination being GH and prolactin.
In addition, a pituitary adenoma may present with visual field defects, classically bitemporal hemianopia. It arises from the compression of the optic nerve by the tumor. The specific area of the visual pathway at which compression by these tumours occurs is at the optic chiasma.
The anatomy of this structure causes pressure on it to produce a defect in the temporal visual field on both sides, a condition called bitemporal hemianopia. If originating superior to the optic chiasm, more commonly in a craniopharyngioma of the pituitary stalk, the visual field defect will first appear as bitemporal inferior quadrantanopia, if originating inferior to the optic chiasm the visual field defect will first appear as bitemporal superior quadrantanopia. Lateral expansion of a pituitary adenoma can also compress the abducens nerve, causing a lateral rectus palsy.
Also, a pituitary adenoma can cause symptoms of increased intracranial pressure.
Prolactinomas often start to give symptoms especially during pregnancy, when the hormone progesterone increases the tumor's growth rate.
Headaches may be present.
Diagnosis and workup
Diagnosis of pituitary adenoma can be made, or at least suspected, by a constellation of related symptoms presented above.
Tumors which cause visual difficulty are likely to be macroadenoma greater than 10 mm in diameter; tumors less than 10 mm are microadenoma.
The differential diagnosis includes pituitary tuberculoma, especially in developing countries and in immumocompromised patients. [8] The diagnosis is confirmed by testing hormone levels, and by radiographic imaging of the pituitary (for example, by CT scan or MRI).
Treatment
Treatment options depend on the type of tumor and on its size:
- Prolactinomas are most often treated with bromocriptine or more recently, cabergoline or quinagolide which decrease tumor size as well as alleviates symptoms, both dopamine agonists, and followed by serial imaging to detect any increase in size. Treatment where the tumor is large can be with radiation therapy or surgery, and patients generally respond well. Efforts have been made to use a progesterone antagonist for the treatment of prolactinomas, but so far have not proved successful.
- Somatotrophic adenomas respond to octreotide, a long-acting somatostatin analog, in many but not all cases according to a review of the medical literature. Unlike prolactinomas, thyrotrophic adenomas characteristically respond poorly to dopamine agonist treatment.[4]
- Surgery is a common treatment for pituitary tumors. Trans-sphenoidal adenectomy surgery can often remove the tumor without affecting other parts of the brain. Endoscopic surgery has become common recently.[9]
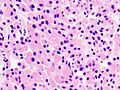
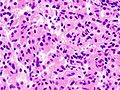
Additional images
References
- ^ Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML, McCutcheon IE. (August 2004). "The prevalence of pituitary adenomas: a systematic review". Cancer 101 (3): 613–9. doi:10.1002/cncr.20412. PMID 15274075.
- ^ Asa SL (August 2008). "Practical pituitary pathology: what does the pathologist need to know?". Arch. Pathol. Lab. Med. 132 (8): 1231–40. doi:10.1043/1543-2165(2008)132[1231:PPPWDT]2.0.CO;2. PMID 18684022. http://journals.allenpress.com/jrnlserv/?request=get-abstract&issn=0003-9985&volume=132&page=1231. Retrieved 2008-09-03.[dead link]
- ^ a b c d e page 526 in: Mandell, Brian F.; Stoller, James K.; Michota, Franklin A. (2009). The Cleveland Clinic Foundation intensive review of internal medicine. Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-9079-4.
- ^ a b Chanson P, Weintraub BD, Harris AG (August 1993). "Octreotide therapy for thyroid-stimulating hormone-secreting pituitary adenomas. A follow-up of 52 patients". Ann. Intern. Med. 119 (3): 236–40. PMID 8323093. http://www.annals.org/cgi/pmidlookup?view=long&pmid=8323093. Retrieved 2008-09-03.
- ^ Ezzat S, Asa SL, Couldwell WT, et al. (August 2004). "The prevalence of pituitary adenomas". Cancer 101 (3): 613–9. doi:10.1002/cncr.20412. PMID 15274075.
- ^ Alicja Furgal-Borzycha et al. (October 2007). "Increased Incidence of Pituitary Microadenomas in Suicide Victims". Neuropsychobiology 54 (3–4): 163–166. doi:10.1159/000106475.
- ^ Forensic Neuropathology p. 137 By Jan E. Leestma
- ^ Saini KS, Patel AL, Shaikh WA, Magar LN, Pungaonkar SA (2007). "Magnetic resonance spectroscopy in pituitary tuberculoma". Singapore Med J 48 (8): 783–6. PMID 17657390.
- ^ [1] American Cancer Society. "Detailed guide: Pituitary tumor. Surgery." Retrieved January 10, 2008
External links
- Cancer.gov: pituitary tumors
- Cleveland Clinic: Evaluation and management of pituitary incidentalomas[2]
- Case report of Bilateral Hemianopsia Due to Pituitary Adenoma. Clinical Cases and Images.
- Medical Illustration of Pituitary Adenomas by Frank H. Netter
- The Pituitary Foundation
- www.AcromegalyCommunity.com Emotional and communal support for those touched by Acromegaly
- - hipofizis.hu Hungarian Pituitary Tumors site
Tumors: endocrine gland neoplasia (C73–C75/D34–D35, 193–194/226–227) Pancreas/
islets of LangerhansHypothalamic/
pituitary axes
+parathyroidPituitaryThyroidThyroid cancer (malignant): epithelial cell /carcinoma (Papillary, Follicular/Hurthle cell) · parafollicular cell (Medullary) · AnaplasticParathyroidGonadssee genital neoplasiaPinealoma MEN Categories:- Endocrine neoplasia
Wikimedia Foundation. 2010.