- Endoscopic retrograde cholangiopancreatography
-
Endoscopic retrograde cholangiopancreatography Intervention 
Duodenoscopic image of two pigment stones extracted from common bile duct after sphincterotomy.ICD-9-CM 51.10 MeSH D002760 OPS-301 code: 1-642 Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject dyes into the ducts in the biliary tree and pancreas so they can be seen on X-rays.
ERCP is used primarily to diagnose and treat conditions of the bile ducts, including gallstones, inflammatory strictures (scars), leaks (from trauma and surgery), and cancer. ERCP can be performed for diagnostic and therapeutic reasons, although the development of safer and relatively non-invasive investigations such as magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound has meant that ERCP is now rarely performed without therapeutic intent.
Contents
Diagnostic
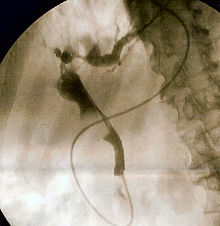 Fluoroscopic image of common bile duct stone seen at the time of ERCP. The stone is impacted in the distal common bile duct. A nasobiliary tube has been inserted.
Fluoroscopic image of common bile duct stone seen at the time of ERCP. The stone is impacted in the distal common bile duct. A nasobiliary tube has been inserted.
- Obstructive jaundice - This may be due to several causes
- Chronic pancreatitis - a now controversial indication due to widespread availability of safer diagnostic modalities including endoscopic ultrasound, high-resolution CT, and MRI/MRCP
- Gallstones with dilated bile ducts on ultrasonography
- Bile duct tumors
- Suspected injury to bile ducts either as a result of trauma or iatrogenic
- Sphincter of Oddi dysfunction
- Pancreatic tumors no longer represent a valid diagnostic indication for ERCP unless they cause bile duct obstruction and jaundice. Endoscopic ultrasound represents a safer and more accurate diagnostic alternative
Therapeutic
- Any of the above when the following may become necessary
- Endoscopic sphincterotomy (both of the biliary and the pancreatic sphincters)
- Removal of stones
- Insertion of stent(s)
- Dilation of strictures (e.g. primary sclerosing cholangitis, anastomotic strictures after liver transplantation)
Contraindications
- Recent myocardial infarction.
- Inadequate surgical back-up
- History of contrast dye anaphylaxis
- Poor health condition for surgery.
- Severe cardiopulmonary disease.
Procedure
The patient is sedated or anaesthetized. Then a flexible camera (endoscope) is inserted through the mouth, down the esophagus, into the stomach, through the pylorus into the duodenum where the ampulla of Vater (the opening of the common bile duct and pancreatic duct) exists. The sphincter of Oddi is a muscular valve that controls the opening of the ampulla. The region can be directly visualized with the endoscopic camera while various procedures are performed. A plastic catheter or cannula is inserted through the ampulla, and radiocontrast is injected into the bile ducts, and/or, pancreatic duct. Fluoroscopy is used to look for blockages, or other lesions such as stones.
When needed, the opening of the ampulla can be enlarged with an electrified wire (sphincterotomy) and access into the bile duct obtained so that gallstones may be removed or other therapy performed.
Other procedures associated with ERCP include the trawling of the common bile duct with a basket or balloon to remove gallstones and the insertion of a plastic stent to assist the drainage of bile. Also, the pancreatic duct can be cannulated and stents be inserted. The pancreatic duct requires visualisation in cases of pancreatitis.
In specific cases, a second camera can be inserted through the channel of the first endoscope. This is termed duodenoscope-assisted cholangiopancreatoscopy (DACP) or mother-daughter ERCP. The daughter scope can be used to administer direct electrohydraulic lithotripsy to break up stones, or to help in diagnosis by directly visualizing the duct (as opposed to obtaining X-ray images).[1]
The gallbladder should be surgically removed (cholecystectomy) following successful removal of gallstones from the bile ducts.[2]
Risks
The major risk of an ERCP is the development of pancreatitis, which can occur in up to 5% of all procedures. This may be self limited and mild, but may require hospitalization, and rarely, may be life-threatening. Patients at additional risk for pancreatitis are younger patients, patients with previous post-ERCP pancreatitis, females, procedures that involve cannulation or injection of the pancreatic duct, and patients with sphincter of Oddi dysfunction.[3]
Gut perforation is a risk of any endoscopic procedure, and is an additional risk if a sphincterotomy is performed. As the second part of the duodenum is anatomically in a retroperitoneal location (that is, behind the peritoneal structures of the abdomen), perforations due to sphincterotomies are also retroperitoneal. Sphincterotomy is also associated with a risk of bleeding.[3]
Oversedation can result in dangerously low blood pressure, respiratory depression, nausea, and vomiting.
There is also a risk associated with the contrast dye in patients who are allergic to compounds containing iodine.
See also
References
- ^ Farrell JJ, Bounds BC, Al-Shalabi S, Jacobson BC, Brugge WR, Schapiro RH, Kelsey PB (2005). "Single-operator duodenoscope-assisted cholangioscopy is an effective alternative in the management of choledocholithiasis not removed by conventional methods, including mechanical lithotripsy". Endoscopy 37 (6): 542–7. doi:10.1055/s-2005-861306. PMID 15933927.
- ^ McAlister VC, Davenport E, Renouf E (2007). McAlister, Vivian. ed. "Cholecystectomy deferral in patients with endoscopic sphincterotomy". Cochrane Database Syst Rev (4): CD006233. doi:10.1002/14651858.CD006233.pub2. PMID 17943900. http://onlinelibrary.wiley.com/o/cochrane/clsysrev/articles/CD006233/frame.html.
- ^ a b Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R (2007). "Incidence rates of post-ERCP complications: a systematic survey of prospective studies". Am. J. Gastroenterol. 102 (8): 1781–8. doi:10.1111/j.1572-0241.2007.01279.x. PMID 17509029.
External links
Categories:- Endoscopy
- Digestive system procedures
Wikimedia Foundation. 2010.

