- Pelvic floor
-
Pelvic floor 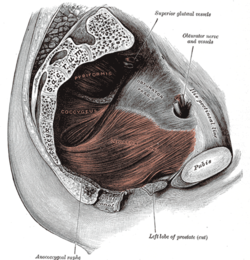
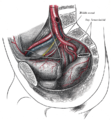
Left Levator ani from within. 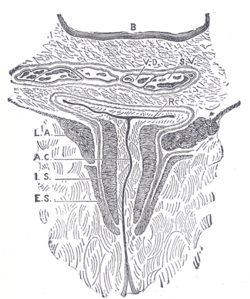
Coronal section through the male anal canal. B. Cavity of urinary bladder V.D. Ductus deferens. S.V. Seminal vesicle. R. Second part of rectum. A.C. Anal canal. L.A. Levator ani. I.S. Sphincter ani internus. E.S. Sphinear ani externus. Latin diaphragma pelvis Gray's subject #119 420 Nerve Sacral nerves 3-4 [1] The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling. Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border). The perineum has the pelvic floor as its superior border.
Some sources do not consider "pelvic floor" and "pelvic diaphragm" to be identical, with the "diaphragm" consisting of only the levator ani and coccygeus, while the "floor" also includes the perineal membrane and deep perineal pouch.[2] However, other sources include the fascia as part of the diaphragm.[3] In practice, the two terms are often used interchangeably.
Posteriorly, the pelvic floor extends into the anal triangle.
Contents
Function
It is important in providing support for pelvic viscera (organs), e.g. the bladder, intestines, the uterus (in females), and in maintenance of continence as part of the urinary and anal sphincters. It facilitates birth by resisting the descent of the presenting part, causing the fetus to rotate forwards to navigate through the pelvic girdle.
Clinical significance
In women, the levator muscles or their supplying nerves can be damaged in pregnancy or childbirth. There is some evidence that these muscles may also be damaged during a hysterectomy. Pelvic surgery using the "perineal approach" (between the anus and coccyx) is an established cause of damage to the pelvic floor. This surgery includes coccygectomy.
In female high-level athletes, perineal trauma is rare and is associated with certain sports (each with a distinct type of trauma): water-skiing, bicycle racing, and equestrian sports.[4]
Damage to the pelvic floor not only contributes to urinary incontinence but can lead to pelvic organ prolapse. Pelvic organ prolapse occurs in women when pelvic organs (e.g. the vagina, bladder, rectum, or uterus) protrude into or outside of the vagina. The causes of pelvic organ prolapse are not unlike those that also contribute to urinary incontinence. These include inappropriate (asymmetrical, excessive, insufficient) muscle tone and asymmetries caused by trauma to the pelvis. Age, pregnancy, family history, and hormonal status all contribute to the development of pelvic organ prolapse. The vagina is suspended by attachments to the perineum, pelvic side wall and sacrum via attachments that include collagen, elastin, and smooth muscle. Surgery can be performed to repair pelvic floor muscles. The pelvic floor muscles can be strengthened with Kegel exercises.
Disorders of the posterior pelvic floor include rectal prolapse, rectocele, perineal hernia, and a number of functional disorders including anismus. Constipation due to any of these disorders is called "functional constipation" and is identifiable by clinical diagnostic criteria.[5]
Pelvic floor exercise (PFE), also known as Kegel exercises, may improve the tone and function of the pelvic floor muscles, which is of particular benefit for women (and less commonly men) who experience stress urinary incontinence.[6][7] However, compliance with PFE programs often is poor,[6] PFE generally is ineffective for urinary incontinence unless performed with biofeedback and trained supervision,[7] and in severe cases it may have no benefit. Pelvic floor muscle tone may be estimated using a perineometer, which measures the pressure within the vagina. Medication may also be used to improve continence. In severe cases, surgery may be used to repair or even to reconstruct the pelvic floor. It has been reported that patients who have overly-toned musculature may suffer from inability to relax the pelvic floor muscles - in effect, Kegel exercises would only exacerbate the problem. http://www.massagetoday.com/mpacms/mt/article.php?id=13515
Perineology or pelviperineology is a speciality dealing with the functional troubles of the three axis (urological, gynaecological and coloproctological) of the pelvic floor.
See also
- Coccyx (Tailbone)
- Pubococcygeus muscle
- Pelvic floor dysfunction
- Perineology
- Perineal hernia
Additional images
References
- ^ Human anatomy at Dartmouth part_6/chapter_37.html#chpt_37_innervation_diaphragm
- ^ Gray's Anatomy For Students. 2005. pp. 391.
- ^ Pelvic+diaphragm at eMedicine Dictionary
- ^ Crepin G, Biserte J, Cosson M, Duchene F (October 2006). "[The female urogenital system and high level sports]" (in French). Bull. Acad. Natl. Med. 190 (7): 1479–91; discussion 1491–3. PMID 17450681.
- ^ Berman L, Aversa J, Abir F, Longo WE (July 2005). "Management of disorders of the posterior pelvic floor". Yale J Biol Med 78 (4): 211–21. PMC 2259151. PMID 16720016. http://openurl.ingenta.com/content/nlm?genre=article&issn=0044-0086&volume=78&issue=4&spage=211&aulast=Berman.
- ^ a b Kielb SJ (2005). "Stress incontinence: alternatives to surgery". Int J Fertil Womens Med 50 (1): 24–9. PMID 15971718.
- ^ a b Harvey MA (June 2003). "Pelvic floor exercises during and after pregnancy: a systematic review of their role in preventing pelvic floor dysfunction". J Obstet Gynaecol Can 25 (6): 487–98. PMID 12806450.
External links
- PC Muscles How to Strengthen
- Overview at nih.gov
- Selection of recent medical literature continuously updated on Pelvic Floor Functional Anatomy
- Pelviperineology The Open Access Journal who consider all the compartments of the pelvis and of the perineum, with the body around and the mind above, as a single unit.
- Pelvic Floor Video Video with overview of pelvic floor muscles and related physical therapy exercises
- Pelvic Floor Exercises blog: how to exercise pelvic floor muscles
- Danger of over-toning muscles
This article was originally based on an entry from a public domain edition of Gray's Anatomy. As such, some of the information contained within it may be outdated.
List of muscles of abdominopelvic cavity (TA A04.5, GA 4.408) Abdomen/
wallAnterior/
lateralMuscleFasciaFascia/abdominal fascia: panniculus adiposus (Fascia of Camper) · stratum membranosum (Fascia of Scarpa) · Transversalis fascia (Interfoveolar ligament)
Linea alba · Linea semilunaris · Inguinal triangle
Inguinal canal (Deep inguinal ring, Superficial inguinal ring, Intercrural fibers, Crura of superficial inguinal ring)
Inguinal ligament (Pectineal ligament, Lacunar ligament, Reflected ligament)PosteriorMuscleFasciaPelvis MuscleFasciafascia/pelvic fascia visceral (Rectovaginal fascia, Rectoprostatic fascia) · parietal (Obturator fascia/Tendinous arch, Piriformis fascia)
floor/diaphragm: Superior fascia of pelvic diaphragm (Pubovesical ligament, Puboprostatic ligament) · Inferior fascia of pelvic diaphragm
Anococcygeal bodyCategories:- Sexual anatomy
- Muscles of the torso
Wikimedia Foundation. 2010.