- Neurodevelopmental disorder
-
A neurodevelopmental disorder,[1] or disorder of neural development, is an impairment of the growth and development of the brain or central nervous system. A narrower use of the term refers to a disorder of brain function that affects emotion, learning ability and memory and that unfolds as the individual grows. The term is sometimes erroneously used as an exclusive synonym for autism and autism spectrum disorders.
Disorders considered to be neurodevelopmental in origin or to have neurodevelopmental consequences when they occur in infancy and childhood include autism and autism spectrum disorders such as Asperger syndrome, traumatic brain injury (including congenital injuries such as those that cause cerebral palsy[2]), communication, speech and language disorders, genetic disorders such as fragile-X syndrome, and Down syndrome.[3] Neurodevelopmental disorders are associated with widely varying degrees of mental, emotional, physical and economic burden to individuals, families and society in general.
Contents
Causes
There are many causes of neurodevelopmental disorder, which can range from deprivation, genetic and metabolic diseases, immune disorders, infectious diseases, nutritional factors, physical trauma, and toxic and environmental factors.
Some neurodevelopmental disorders such as autism,Nampoothiri Syndrome and other pervasive developmental disorders are considered to be multifactorial syndromes (with many causes but more specific neurodevelopmental manifestation).[4] However other multifactorial syndromes such as Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections (PANDAS) are presently thought to have a more specific primary causation as well as a specific neurodevelopmental manifestation.
Deprivation
Infants and children require loving emotional nurture from caregivers—there is a spectrum of problems arising from the lack of it. The most severe deprivation disorder, hospitalism, was described in 1897 as a wasting away to the point of death.[5] A sublethal form, anaclitic depression was first described by René Spitz in the 1940s. It occurred in infants over the age of six months who suffered the loss of their mothers, who then became depressed and showed behavioral retardation (delay in reaching developmental milestones, especially as related to social behaviors).[6] Behavioral retardation, as in the reactive attachment disorders, has been observed in emotionally deprived children living with their families.[7][8] However, prominent modern thought attributes other causative mechanisms to autism and autistic spectrum disorders. (see Autism)
However, nurture is not the only cause of deprivation that leads to neurodevelopmental sequellae. A common example of sensory deprivation due to biologic factors is blindness. Blind infants have risk of poor developmental outcomes which, left untreated, may lead to severe, autistic-like behaviors.[9] Despite its biologic basis, caregivers can ameliorate blindness-related sensory deprivation.[10] This can lead to positive neurodevelopmental outcome, as in the cases of author Helen Keller,[11] who was trained in the use of tactile sign language, and musicians such as Arthel "Doc" Watson[12] and Ray Charles who remained emotionally connected to others via their sense of hearing.
Genetic disorders
A prominent example of a genetically determined neurodevelopmental disorder is Trisomy 21, also known as Down syndrome. This disorder usually results from an extra chromosome 21, although in uncommon instances it is related to other chromosomal abnormalities such as translocation of the genetic material. It is characterized by short stature, epicanthal (eyelid) folds, abnormal fingerprints and palm prints, heart defects, poor muscle tone (delay of neurological development) and mental retardation (delay of intellectual development).[3]
Less commonly known genetically determined neurodevelopmental disorders include Fragile X syndrome, Rett syndrome and Williams syndrome. Fragile X syndrome was first described in 1943 by J.P. Martin and J. Bell, studying persons with family history of sex-linked "mental defects".[13] Rett syndrome, another X-linked disorder, produces severe functional limitations.[14] Williams syndrome is caused by small deletions of genetic material from chromosome 7.[15]
Immune dysfunction
Immune reactions during pregnancy, both maternal and of the developing child can produce neurodevelopmental disorders. One typical immune reaction in infants and children is PANDAS,[16] or Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection produce abnormal movements of the body, emotional disturbance and obsessive compulsive disorder symptoms.[17] Another disorder is Sydenham's chorea, which results in more abnormal movements of the body and fewer psychological sequellae. Both are immune reactions against brain tissue that follow infection by Streptococcus bacteria. (Susceptibility to these immune diseases may be genetically determined,[18] so sometimes several family members may suffer from one or both of them following an epidemic of Strep infection.)
Infectious diseases
A number of infectious diseases can be transmitted either congenitally or in early childhood, and can cause serious neurodevelopmental disorders, such as schizophrenia.[19] Congenital toxoplasmosis may result in formation of cysts in the brain and other organs, causing a variety of neurological deficits. Congenital syphilis may progress to neurosyphilis if it remains untreated. Measles can progress to subacute sclerosing panencephalitis. Congenital rubella syndrome can produce schizophrenia in addition to multiple other symptoms.
Metabolic disorders
Metabolic disorders, present in either the mother or the child, can cause neurodevelopmental disorders. Two examples are diabetes mellitus (a multifactorial disorder) and phenylketonuria (an inborn error of metabolism). Many such inherited diseases may directly affect the child's metabolism and neural development[20] but less commonly they can indirectly affect the child during gestation. (See also teratology).
In the child, type 1 diabetes can produce neurodevelopmental damage by the effects of excessive or insufficient glucose. The problems continue and may worsen throughout childhood if the diabetes is not well controlled.[21] Type 2 diabetes may be preceded in its onset by impaired cognitive functioning.[22]
However a non-diabetic fetus can also be subjected to glucose effects if its mother has undetected gestational diabetes. Maternal diabetes causes excessive birth size, making it harder for the infant to pass through the birth canal without injury or it can directly produce early neurodevelopmental deficits. However usually the neurodevelopmental symptoms decrease in later childhood.[23]
Phenylketonuria, also known as PKU is an inborn error of metabolism that can induce neurodevelopmental disorders in children. Children with PKU require a strict diet to prevent mental retardation and other disorders. In the maternal form of PKU, excessive maternal phenylalanine can be absorbed by the fetus even if the fetus has not inherited the disease. This can produce mental retardation and other disorders.[24][25]
Nutrition
Nutritional deficits may cause neurodevelopmental disorders, such as spina bifida, which is common, and anencephaly, which is rare. Both disorders are neural tube defects with malformation and dysfunction of the nervous system and its supporting structures, leading to serious physical disability as well as its emotional sequellae. The most common nutritional cause of neural tube defects is maternal deficiency of folic acid, a B vitamin usually found in fruits, vegetables, whole grains and milk products.[26][27] (Neural tube defects are also caused by medications and other environmental causes, many of which interfere with folate metabolism, thus they are considered to have multifactorial causes.)[28][29] Another deficiency, iodine deficiency, produces a spectrum of neurodevelopmental disorders from mild emotional disturbance to severe mental retardation. (see also cretinism)
Excesses in both maternal and infant diets may cause disorders as well, with foods or food supplements proving toxic in large amounts. For instance in 1973 K.L. Jones and D.W. Smith of the University of Washington Medical School in Seattle found a pattern of "craniofacial, limb, and cardiovascular defects associated with prenatal onset growth deficiency and developmental delay" in children of alcoholic mothers. This disorder, now called fetal alcohol syndrome, has significant symptom overlap with several other entirely unrelated neurodevelopmental disorders.[30] It has been discovered that iron supplementation in baby formula is linked to lowered I.Q. and other neurodevelopmental delays.[31]
Trauma
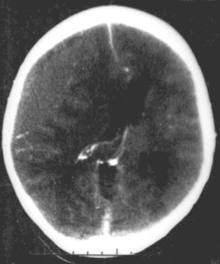
Brain trauma in the developing human is a common cause (over 400,000 injuries per year in the US alone, without clear information as to how many produce developmental sequellae)[32] of neurodevelopmental syndromes. It may be subdivided into two major categories, congenital injury (including injury resulting from otherwise uncomplicated premature birth)[2] and injury occurring in infancy or childhood. Common causes of congenital injury are asphyxia (obstruction of the trachea), hypoxia (lack of oxygen to the brain) and the mechanical trauma of the birth process itself.
Overwhelmingly, in industrial nations the most common causes of childhood brain trauma are falls and transportation-related incidents.[33][34] Child maltreatment such as shaken baby syndrome can produce neurodevelopmental consequences including blindness, neuromotor deficits and cognitive impairment.[35] According to information published by the American Association of Neurological Surgeons, sports injuries account for 21% of the US incidence, however their site includes transportation-related sports injuries. They assert that cycling produced 64,993 head injuries requiring emergency room visits in 2007 while the second most common cause, football, only produced 36,412.[36]
Toxic and environmental factors
One well known environmental toxic cause of neurodevelopmental disorders is heavy metal poisoning, with a prominent 20th century example being Minamata disease. Developmental mercury poisoning can cause a spectrum of problems from mild impairment of emotional development to the full blown syndrome of peripheral nerve damage, visual impairment, impaired coordination and ambulation, hallucinations, mental retardation, depression and death. However other metals such as lead, manganese, arsenic, cadmium and iron, as well as prenatal exposure to pesticides, tobacco and other environmental toxins are also implicated as causative factors.[37]
See also
Bibliography
- Tager-Flusberg, Helen (1999). Neurodevelopmental disorders. Cambridge, Mass: MIT Press. ISBN 0-262-20116-X.
- Brooks, David R.; Walter Wolfgang Fleischhacker (2006). Neurodevelopmental Disorders. Berlin: Springer. ISBN 3-211-26291-1.
Notes
- ^ Reynolds, Cecil R.; Goldstein, Sam (1999). Handbook of neurodevelopmental and genetic disorders in children. New York: The Guilford Press. pp. 3–8. ISBN 1-57230-448-0.
- ^ a b Murray RM, Lewis SW (September 1987). "Is schizophrenia a neurodevelopmental disorder?". Br Med J (Clin Res Ed) 295 (6600): 681–2. doi:10.1136/bmj.295.6600.681. PMC 1247717. PMID 3117295. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1247717.
- ^ a b http://www.nads.org/pages_new/facts.html Facts about down syndrome
- ^ Samaco RC, Hogart A, LaSalle JM (February 2005). "Epigenetic overlap in autism-spectrum neurodevelopmental disorders: MECP2 deficiency causes reduced expression of UBE3A and GABRB3". Hum. Mol. Genet. 14 (4): 483–92. doi:10.1093/hmg/ddi045. PMC 1224722. PMID 15615769. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1224722.>
- ^ Crandall, Floyd M. (June 1897). "Hospitalism". Archives of Pediatrics 14 (6): 448–54. http://www.neonatology.org/classics/crandall.html. Retrieved 2008-08-02.
- ^ definition of Anaclitic depression
- ^ Coleman RW, Provence S (1 February 1957). "Environmental retardation (hospitalism) in infants living in families". Pediatrics 19 (2): 285–92. PMID 13400604. http://pediatrics.aappublications.org/cgi/content/abstract/19/2/285.
- ^ Newman L, Mares S (July 2007). "Recent advances in the theories of and interventions with attachment disorders". Curr Opin Psychiatry 20 (4): 343–8. doi:10.1097/YCO.0b013e3281bc0d08. PMID 17551348. http://www.medscape.com/viewarticle/559998_print.
- ^ Sonksen PM, Dale N (November 2002). "Visual impairment in infancy: impact on neurodevelopmental and neurobiological processes". Dev Med Child Neurol 44 (11): 782–91. doi:10.1017/S0012162201002936. PMID 12418621. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0012-1622&date=2002&volume=44&issue=11&spage=782.
- ^ Warren, David H. (1994). Blindness and children: an individual differences approach. Cambridge, UK: Cambridge University Press. pp. 323–30. ISBN 0-521-45719-X.
- ^ Keller, Helen (2002). The story of my life (100th Anniversary Edition) (Signet Classics (Paperback)). Signet Classics. ISBN 0-451-52825-5.
- ^ Miller, Dan (October 2-8, 2000). "Doc Watson: flatpicking legend". Featured Artist. Flatpicking Guitar Magazine. http://www.flatpick.com/Pages/Featured_Artist/Doc.html. Retrieved 2008-08-17.
- ^ Martin JP, Bell J (1943). "A pedigree of mental defect showing sex-linkage". J. Neurol. Psychiat. 6 (3–4): 154–7. doi:10.1136/jnnp.6.3-4.154. http://jnnp.bmj.com/cgi/reprint/jnnp;6/3-4/154?.
- ^ Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY (October 1999). "Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2". Nat. Genet. 23 (2): 185–8. doi:10.1038/13810. PMID 10508514. http://www.nature.com/ng/journal/v23/n2/full/ng1099_185.html.
- ^ Merla G, Howald C, Henrichsen CN et al. (August 2006). "Submicroscopic Deletion in Patients with Williams-Beuren Syndrome Influences Expression Levels of the Nonhemizygous Flanking Genes". Am. J. Hum. Genet. 79 (2): 332–41. doi:10.1086/506371. PMC 1559497. PMID 16826523. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1559497.
- ^ Pavone, P. et al. (2004). "Anti-brain antibodies in PANDAS versus uncomplicated streptococcal infection". Pediatr Neurol 30 (2): 107–110. doi:10.1016/S0887-8994(03)00413-2. PMID 14984902.
- ^ Dale, RC. et al. (2005). "Incidence of anti-brain antibodies in children with obsessive–compulsive disorder". Brit J Psychiatry 187 (4): 314–319. doi:10.1192/bjp.187.4.314. PMID 16199788. http://bjp.rcpsych.org/cgi/content/full/187/4/314. Retrieved 2008-08-17.
- ^ Swedo, Susan E (December 2001). "Genetics of childhood disorders: XXXIII autoimmunity part 6: poststreptoccoal autoimmunity". Reprinted from J Am Acad Child Adolesc Psychiatry, 40:12,1479-1482. http://www.med.yale.edu/chldstdy/plomdevelop/genetics/01decgen.htm. Retrieved 2008-08-17.
- ^ "Prenatal infection as a risk factor for schizophrenia – Brown 32 (2): 200 – Schizophrenia Bulletin". http://schizophreniabulletin.oxfordjournals.org/cgi/content/full/32/2/200. Retrieved 2008-08-10.
- ^ Richardson, A.J.; Ross, M.A. (July 2000). "Fatty acid metabolism in neurodevelopmental disorder: a new perspective on associations between attention-deficit/hyperactivity disorder, dyslexia, dyspraxia and the autistic spectrum". Prostaglandins, Leukotrienes and Essential Fatty Acids 63 (1–2): 1–9. doi:10.1054/plef.2000.0184. PMID 10970706. http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6WPH-45BCP10-1&_user=10&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=4a168193b6c6acc3a36be28198f9bc00.
- ^ Nordham, Elizabeth A; et al., PJ; Jacobs, R; Hughes, M; Warne, GL; Werther, GA (2001). "Neuropsychological Profiles of Children With Type 1 Diabetes 6 Years After Disease Onset". Diabetes Care 24 (9): 1541–1546. doi:10.2337/diacare.24.9.1541. PMID 11522696. http://care.diabetesjournals.org/cgi/content/full/24/9/1541.
- ^ Olsson, Gunilla M.; et al., AL; Montgomery, SM (2008). "Cognitive Function in Children and Subsequent Type 2 Diabetes: Response to Batty, Gale, and Deary". Diabetes Care 31 (3): 514–516. doi:10.2337/dc07-1399. PMC 2453642. PMID 18083794. http://mail.turkiye-klinikleri.com/cgi/content/full/31/3/514.
- ^ Ornoy A, Wolf A, Ratzon N, Greenbaum C, Dulitzky M (July 1999). "Neurodevelopmental outcome at early school age of children born to mothers with gestational diabetes". Arch. Dis. Child. Fetal Neonatal Ed. 81 (1): F10–4. doi:10.1136/fn.81.1.F10. PMC 1720965. PMID 10375355. http://fn.bmj.com/cgi/pmidlookup?view=long&pmid=10375355.
- ^ Lee PJ, Ridout D, Walter JH, Cockburn F (February 2005). "Maternal phenylketonuria: report from the United Kingdom Registry 1978–97". Arch. Dis. Child. 90 (2): 143–6. doi:10.1136/adc.2003.037762. PMC 1720245. PMID 15665165. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1720245.
- ^ Rouse B, Azen C, Koch R et al. (March 1997). "Maternal Phenylketonuria Collaborative Study (MPKUCS) offspring: facial anomalies, malformations, and early neurological sequelae". Am. J. Med. Genet. 69 (1): 89–95. doi:10.1002/(SICI)1096-8628(19970303)69:1<89::AID-AJMG17>3.0.CO;2-K. PMID 9066890.
- ^ "Folic Acid - March of Dimes". http://www.marchofdimes.com/professionals/14332_1151.asp.
- ^ "Folate (Folacin, Folic Acid)". http://ohioline.osu.edu/hyg-fact/5000/5553.html.
- ^ "Folic scid: topic home". Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. http://www.cdc.gov/ncbddd/folicacid/. Retrieved 2008-08-02.
- ^ "The basics about spina bifida". Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. http://www.cdc.gov/ncbddd/folicacid/. Retrieved 2008-08-02.
- ^ Fetal alcohol syndrome: guidelines for referral and diagnosis (PDF). CDC (July 2004). Retrieved on 2007-04-11
- ^ Kerr, Martha; Désirée Lie (2008). "Neurodevelopmental delays associated with iron-fortified formula for healthy infants". Medscape Psychiatry and Mental Health. http://www.medscape.com/viewarticle/574363. Retrieved 2008-08-04.
- ^ "Facts About TBI" (PDF). http://www.cdc.gov/ncipc/tbi/FactSheets/Facts_About_TBI.pdf. Retrieved 2008-08-06.
- ^ Centers for Disease Control and Prevention (CDC) (March 2006). "Incidence rates of hospitalization related to traumatic brain injury—12 states, 2002". MMWR Morb. Mortal. Wkly. Rep. 55 (8): 201–4. PMID 16511440. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5508a2.htm.
- ^ "TBI in the US". http://www.cdc.gov/ncipc/pub-res/TBI_in_US_04/TBI_ED.htm.
- ^ "Child maltreatment prevention scientific information: consequences". http://www.cdc.gov/ncipc/dvp/CMP/CMP-conque.htm.
- ^ "NeurosurgeryToday.org |What is Neurosurgery |Patient Education Materials |sports-related head injury". http://www.neurosurgerytoday.org/what/patient_e/sports.asp?link_id=5792. Retrieved 2008-08-17.
- ^ "Autism and neurodevelopmental disorders". Children's Environmental Health Centers (CEHCs). U.S. Environmental Health Agency. http://epa.gov/ncer/childrenscenters/autism.html. Retrieved 2011-04-26.
External links
- A Classification of "Neurodevelopmental Disorders" - The Hunterdon Developmental Center
- A Review of Neurodevelopmental Disorders - Medscape review
- Developmental Fx (The Developmental and Fragile X Resource site)
- Neurodevelopmental Disorders at the Open Directory Project
- Mary Ann Knight Institute (portal for Miami Hospital children's services)
- Medical Information on Neurodevelopmental Disorders (M.I.N.D.) - The Hunterdon Developmental Center
- Neurogenetic and neurodevelopmental disorders - listing of neurodevelopmental disorders of interest to the Stanford University School of Medicine CoGENT project. (see also http://cogent.stanford.edu/ CoGENT home page)
- UC Davis M.I.N.D. Institute (portal for the UC Davis site)
Categories:- Childhood psychiatric disorders
- Developmental neuroscience
- Disability
- Neurological disorders
Wikimedia Foundation. 2010.