- Prader–Willi syndrome
-
Prader-Willi syndrome Classification and external resources ICD-10 Q87.1 ICD-9 759.81 OMIM 176270 DiseasesDB 10481 eMedicine ped/1880 MeSH D011218  A 1680 painting "La monstrua desnuda" by Juan Carreño de Miranda of a girl presumed to have Prader-Willi syndrome[1]
A 1680 painting "La monstrua desnuda" by Juan Carreño de Miranda of a girl presumed to have Prader-Willi syndrome[1]
Prader–Willi syndrome (abbreviated PWS) is a rare genetic disorder in which seven genes (or some subset thereof) on chromosome 15 (q 11–13) are deleted or unexpressed (chromosome 15q partial deletion) on the paternal chromosome. It was first described in 1956 by Andrea Prader (1919–2001), Heinrich Willi (1900–1971), Alexis Labhart (1916), Andrew Ziegler, and Guido Fanconi of Switzerland.[2] The incidence of PWS is between 1 in 25,000 and 1 in 10,000 live births. The paternal origin of the genetic material that is affected in the syndrome is important because the particular region of chromosome 15 involved is subject to parent of origin imprinting, meaning that for a number of genes in this region only one copy of the gene is expressed while the other is silenced through imprinting. For the genes affected in PWS, it is the paternal copy that is usually expressed, while the maternal copy is silenced. This means that while most people have a single working copy of these genes, people with PWS have no working copy. PWS has the sister syndrome Angelman syndrome in which maternally derived genetic material is affected in the same genetic region.
Contents
Signs and symptoms
Clinical features and signs
Holm et al. (1993) describe the following features and signs as pretest indicators of PWS, although not all will be present.
- In utero
- Reduced fetal movement
- Frequent abnormal fetal position
- Occasional polyhydramnios (excessive amniotic fluid)
- At birth
- Often breech or caesarean births
- Lethargy
- Hypotonia
- Feeding difficulties (due to poor muscle tone affecting sucking reflex)
- Difficulties establishing respiration
- Hypogonadism
- Infancy
- Failure to thrive (continued feeding difficulties)
- Delayed milestones/intellectual delay
- Excessive sleeping
- Strabismus ('crossed eyes')
- Scoliosis (often not detected at birth)
- Cyrptorchidism
- Childhood
- Speech delay
- Poor physical coordination
- Hyperphagia (over-eating) from age 2 – 8 years. Note change from feeding difficulties in infancy
- Excessive weight gain
- Sleep disorders
- Scoliosis
- Adolescence
- Delayed puberty
- Short stature
- Obesity
- Extreme flexibility
- Adulthood
- Infertility (males and females)
- Hypogonadism
- Sparse pubic hair
- Obesity
- Hypotonia (low muscle tone)
- Learning disabilities/borderline intellectual functioning (but some cases of average intelligence)
- Prone to diabetes mellitus
- Extreme flexibility
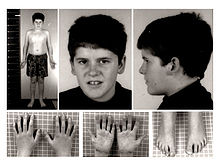
- General physical appearance (adults)
- Prominent nasal bridge
- Small hands and feet with tapering of fingers
- Soft skin, which is easily bruised
- Excess fat, especially in the central portion of the body
- High, narrow forehead
- Almond-shaped eyes with thin, down-turned lids
- Light skin and hair relative to other family members
- Lack of complete sexual development
- Frequent skin picking
- Striae
- Delayed motor development
Neuro-cognitive
Individuals with PWS are at risk of learning and attention difficulties. Curfs and Fryns (1992) conducted research into the varying degrees of learning disability found in Prader Willi Syndrome (PWS).[3] Their results were as follows:
- 5%: IQ above 85 (average to low average intelligence)
- 27%: IQ 70 – 85 (borderline intellectual functioning)
- 39%: IQ 50 – 70 (mild intellectual disability)
- 27%: IQ 35 – 50 (moderate intellectual disability)
- 1%: IQ 20 – 35 (severe intellectual disability)
- <1%: IQ <20 (profound intellectual disability)
Cassidy found that 40% of individuals with PWS have borderline/low average intelligence,[4] a figure higher than that found in Curfs and Fryns' study (32%).[3] However, both studies suggest that most individuals (50–65%) fall within the mild/borderline/low average intelligence range.
Children with PWS show an unusual cognitive profile. They are often strong in visual organization and perception, including reading and vocabulary, but their spoken language (sometimes affected by hypernasality) is generally poorer than their comprehension. A marked skill in completing jigsaw puzzles has been noted,[5][6] although this may be an effect of increased practice.[7]
Auditory information processing and sequential processing are relatively poor, as are arithmetic and writing skills, visual and auditory short term memory and auditory attention span. These sometimes improve with age, but deficits in these areas remain throughout adulthood.[5]
Behavioral
Prader–Willi syndrome is also frequently associated with an extreme and insatiable appetite, often resulting in morbid obesity. There is currently no consensus as to the cause for this particular symptom, although genetic abnormalities in chromosome 15 disrupt the normal functioning of the hypothalamus.[4] Given that the hypothalamus regulates many basic processes, including appetite, there may well be a link. In the hypothalamus of PWS patients, nerve cells that produce oxytocin, a hormone thought to contribute to satiety, have been found to be abnormal.
Prader–Willi syndrome patients have high ghrelin levels, which are thought to directly contribute to the increased appetite, hyperphagia, and obesity seen in this syndrome. Cassidy states the need for a clear delineation of behavioural expectations, the reinforcement of behavioural limits and the establishment of regular routines.[21]
The main mental health difficulties experienced by people with PWS include compulsive behaviour (usually manifested in skin-picking) and anxiety.[5][8] Psychiatric symptoms, for example, hallucinations, paranoia and depression have been described in some cases[5] and affect approximately 5–10% of young adults.[4] Psychiatric and behavioural problems are the most common cause of hospitalization.[9]
Endocrine
There are several aspects of PWS that support the concept of growth hormone deficiency in individuals with PWS. Specifically, individuals with PWS have short stature, are obese with abnormal body composition, have reduced fat free mass (FFM), have reduced LBM and total energy expenditure, and have decreased bone density.
PWS is characterized by hypogonadism. This is manifested as undescended testes in males and benign premature adrenarche in females. Testes may descend with time or can be managed with surgery or testosterone replacement. Adrenarche may be treated with hormone replacement therapy.
Genetics
PWS is caused by the deletion of the paternal copies of the imprinted SNRPN and necdin genes along with clusters of snoRNAs: SNORD64, SNORD107, SNORD108 and two copies of SNORD109, 29 copies of SNORD116 (HBII-85) and 48 copies of SNORD115 (HBII-52). These are on chromosome 15 located in the region 15q11-13.[10][11][12] This so-called PWS/AS region may be lost by one of several genetic mechanisms which, in the majority of instances occurs through chance mutation. Other less common mechanisms include; uniparental disomy, sporadic mutations, chromosome translocations, and gene deletions. Due to imprinting, the maternally inherited copies of these genes are virtually silent, only the paternal copies of the genes are expressed. PWS results from the loss of paternal copies of this region. Deletion of the same region on the maternal chromosome causes Angelman syndrome (AS). PWS and AS represent the first reported instances of imprinting disorders in humans.
The risk to the sibling of an affected child of having PWS depends upon the genetic mechanism which caused the disorder. The risk to siblings is <1% if the affected child has a gene deletion or uniparental disomy, up to 50% if the affected child has a mutation of the imprinting control region, and up to 25% if a parental chromosomal translocation is present. Prenatal testing is possible for any of the known genetic mechanisms.
A microdeletion in one family of the snoRNA HBII-52 has excluded it from playing a major role in the disease.[13]
Studies of human and mouse model systems have shown that deletion of the 29 copies of the C/D box snoRNA SNORD116 (HBII-85) has been shown to be the primary cause of Prader–Willi syndrome.[14][15][16][17] [18]
Diagnosis
PWS affects approximately 1 in 10,000 to 1 in 25,000 newborns.[19] There are more than 400,000 people who live with PWS around the world.[20] It is traditionally characterized by hypotonia, short stature, hyperphagia, obesity, behavioral issues (specifically OCD-like behaviors), small hands and feet, hypogonadism, and mild mental retardation.[19] However, with early diagnosis and early treatment (such as with growth hormone therapy), the prognosis for persons with PWS is beginning to change. Like autism, PWS is a spectrum disorder and so symptoms can range from mild to severe, and may change throughout the person's lifetime. Various organ systems are affected.
Traditionally, Prader-Willi Syndrome was diagnosed by clinical presentation. Currently, the syndrome is diagnosed through genetic testing; testing is recommended for newborns with pronounced hypotonia. Early diagnosis of PWS allows for early intervention as well as the early prescription of growth hormone. Daily recombinant growth hormone (GH) injections are indicated for children with PWS. GH supports linear growth and increased muscle mass, and may lessen food preoccupation and weight gain.
The mainstay of diagnosis is genetic testing, specifically DNA-based methylation testing to detect the absence of the paternally contributed Prader–Willi syndrome/Angelman syndrome (PWS/AS) region on chromosome 15q11-q13. Such testing detects over 97% of patients. Methylation-specific testing is important to confirm the diagnosis of PWS in all individuals, but especially those who are too young to manifest sufficient features to make the diagnosis on clinical grounds or in those individuals who have atypical findings. Because PWS infants have a higher rate of difficulties at birth (including breech delivery and respiratory delay) birth-related injuries and oxygen deprivation may complicate the genetic handicaps, resulting in atypical PWS.[citation needed]
Differential diagnosis
Prader–Willi syndrome is often misdiagnosed as a variety of other syndromes due to many in the medical community's unfamiliarity with PWS. Sometimes it is misdiagnosed as Down syndrome, simply because of the relative frequency of Down syndrome compared to PWS. Also, marked obesity can occur in Down syndrome due to behavioral problems. Adding to the confusion, parents of children who already carry a diagnosis of Prader–Willi syndrome may tell friends, family, and even physicians and nurses that their child has Down syndrome because more people have heard of that condition.[citation needed] It is thought that 75% of those with PWS are undiagnosed.
Treatment
Prader–Willi syndrome has no cure; however, several treatments are in place to lessen the condition's symptoms. During infancy, subjects should undergo therapies to improve muscle tone. Speech and occupational therapy are also indicated. During the school years, children benefit from a highly structured learning environment as well as extra help. The largest problem associated with the syndrome is severe obesity.
Prescription of daily recombinant growth hormone injections are indicated for children with PWS. GH supports linear growth and increased muscle mass, and may lessen food preoccupation and weight gain.[21][22][23]
Because of severe obesity, obstructive sleep apnea is a common sequela, and a positive airway pressure machine is often needed.
Society and culture
Prader–Willi syndrome appeared in the UK media in July 2007 when Channel 4 aired a program Can't Stop Eating, surrounding the everyday lives of two Prader-Willi patients, Joe and Tamara.[24]
An individual with Prader-Willi Syndrome featured in the episode entitled "Dog Eat Dog" of the television series CSI: Crime Scene Investigation (aired on November 24, 2005).[25]
Another individual with Prader–Willi syndrome, Ethan Starkweather, was on Extreme Makeover: Home Edition originally aired on Mothers Day 2010.
On TLC's My Deadly Appetite (aired in December 2010), a patient named Will was treated for the condition (as well as others featured).[1]
In Judas Strain, a book by James Rollins, victims of an unknown plague suffer from Prader-Willi as a side-effect, gorging themselves on human flesh until their stomachs explode.
See also
References
- ^ Mary Jones. "Case Study: Cataplexy and SOREMPs Without Excessive Daytime Sleepiness in Prader Willi Syndrome. Is This the Beginning of Narcolepsy in a Five Year Old?". European Society of Sleep Technologists. http://www.esst.org/newsletter2000.htm. Retrieved April 6, 2009.
- ^ synd/1836 at Who Named It?
- ^ a b Curfs LM, Fryns JP (1992). "Prader-Willi syndrome: a review with special attention to the cognitive and behavioral profile". Birth Defects Orig. Artic. Ser. 28 (1): 99–104. PMID 1340242.
- ^ a b c Cassidy SB (1997). "Prader-Willi syndrome". J. Med. Genet. 34 (11): 917–23. doi:10.1136/jmg.34.11.917. PMC 1051120. PMID 9391886. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1051120.
- ^ a b c d Udwin O (November 1998). "Prader-Willi syndrome: Psychological and behavioural characteristics". Contact a Family. http://www.cafamily.org.uk/medicalinformation/conditions/azlistings/p33_3.html.
- ^ Holm VA, Cassidy SB, Butler MG, et al. (1993). "Prader-Willi syndrome: consensus diagnostic criteria". Pediatrics 91 (2): 398–402. PMID 8424017.
- ^ Whittington J, Holland A, Webb T, Butler J, Clarke D, Boer H (February 2004). "Cognitive abilities and genotype in a population-based sample of people with Prader-Willi syndrome". J Intellect Disabil Res 48 (Pt 2): 172–87. doi:10.1111/j.1365-2788.2004.00556.x. PMID 14723659.
- ^ Clark DJ, Boer H, Webb T (1995). "General and behavioural aspects of PWS: a review". Mental Health Research 8 (195): 38–49.
- ^ Cassidy SB, Devi A, Mukaida C (1994). "Aging in PWS: 232 patients over age 30 years". Proc. Greenwood Genetic Centre 13: 102–3.
- ^ Online 'Mendelian Inheritance in Man' (OMIM) Prader-Willi Syndrome; PWS -17627
- ^ de los Santos T, Schweizer J, Rees CA, Francke U (November 2000). "Small evolutionarily conserved RNA, resembling C/D box small nucleolar RNA, is transcribed from PWCR1, a novel imprinted gene in the Prader-Willi deletion region, which Is highly expressed in brain". Am. J. Hum. Genet. 67 (5): 1067–82. doi:10.1086/303106. PMC 1288549. PMID 11007541. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1288549.
- ^ Cavaillé J, Buiting K, Kiefmann M, et al. (December 2000). "Identification of brain-specific and imprinted small nucleolar RNA genes exhibiting an unusual genomic organization". Proc. Natl. Acad. Sci. U.S.A. 97 (26): 14311–6. doi:10.1073/pnas.250426397. PMC 18915. PMID 11106375. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=18915.
- ^ Runte M, Varon R, Horn D, Horsthemke B, Buiting K (2005). "Exclusion of the C/D box snoRNA gene cluster HBII-52 from a major role in Prader-Willi syndrome.". Hum Genet 116 (3): 228–30. doi:10.1007/s00439-004-1219-2. PMID 15565282.
- ^ Skryabin BV, Gubar LV, Seeger B, et al. (2007). "Deletion of the MBII-85 snoRNA gene cluster in mice results in postnatal growth retardation". PLoS Genet. 3 (12): e235. doi:10.1371/journal.pgen.0030235. PMC 2323313. PMID 18166085. http://www.plosgenetics.org/article/info:doi/10.1371/journal.pgen.0030235.
- ^ Sahoo T, del Gaudio D, German JR, Shinawi M, Peters SU, Person RE, Garnica A, Cheung SW, Beaudet AL (2008). "Prader-Willi phenotype caused by paternal deficiency for the HBII-85 C/D box small nucleolar RNA cluster.". Nat Genet 40 (6): 719–21. doi:10.1038/ng.158. PMC 2705197. PMID 18500341. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2705197.
- ^ Ding F, Li HH, Zhang S, Solomon NM, Camper SA, Cohen P, Francke U (2008). Akbarian, Schahram. ed. "SnoRNA Snord116 (Pwcr1/MBII-85) deletion causes growth deficiency and hyperphagia in mice". PLoS ONE 3 (3): e1709. doi:10.1371/journal.pone.0001709. PMC 2248623. PMID 18320030. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2248623.
- ^ Ding F, Prints Y, Dhar MS, Johnson DK, Garnacho-Montero C, Nicholls RD, Francke U (2005). "Lack of Pwcr1/MBII-85 snoRNA is critical for neonatal lethality in Prader-Willi syndrome mouse models". Mamm Genome 16 (6): 424–31. doi:10.1007/s00335-005-2460-2. PMID 16075369.
- ^ de Smith AJ, Purmann C, Walters RG, et al. (June 2009). "A Deletion of the HBII-85 Class of Small Nucleolar RNAs (snoRNAs) is Associated with Hyperphagia, Obesity and Hypogonadism". Hum. Mol. Genet. 18 (17): 3257–65. doi:10.1093/hmg/ddp263. PMC 2722987. PMID 19498035. http://hmg.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=19498035.
- ^ a b Killeen, Anthony A. (2004). "Genetic Inheritance". Principles of Molecular Pathology. Humana Press. pp. 41. ISBN 9781588290854. http://books.google.com/books?id=oHcDreGaMm0C&pg=PA41.
- ^ [|Tweed, Katherine] (September 2009). "Shawn Cooper Struggles with Prader Willi Syndrome". AOL Health. http://www.aolhealth.com/health/living-with-prader-willi-syndrome. Retrieved September 2009.
- ^ Davies PS, Evans S, Broomhead S, et al. (May 1998). "Effect of growth hormone on height, weight, and body composition in Prader-Willi syndrome". Arch. Dis. Child. 78 (5): 474–6. doi:10.1136/adc.78.5.474. PMC 1717576. PMID 9659098. http://adc.bmj.com/cgi/pmidlookup?view=long&pmid=9659098.
- ^ Carrel AL, Myers SE, Whitman BY, Allen DB (April 2002). "Benefits of long-term GH therapy in Prader-Willi syndrome: a 4-year study". J. Clin. Endocrinol. Metab. 87 (4): 1581–5. doi:10.1210/jc.87.4.1581. PMID 11932286.
- ^ Höybye C, Hilding A, Jacobsson H, Thorén M (May 2003). "Growth hormone treatment improves body composition in adults with Prader-Willi syndrome". Clin. Endocrinol. (Oxf) 58 (5): 653–61. doi:10.1046/j.1365-2265.2003.01769.x. PMID 12699450. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0300-0664&date=2003&volume=58&issue=5&spage=653.
- ^ "Can't Stop Eating". 2006. http://www.channel4.com/health/microsites/F/family/problems/pws.html. Retrieved 2009-06-12.
- ^ "Dog Eat Dog". www.csifiles.com. http://www.csifiles.com/reviews/csi/dog_eat_dog.shtml. Retrieved 2009-06-12.
External links
- PWS research short film
- Prader-Willi syndrome explanation Video
- Prader–Willi syndrome at the Open Directory Project
- Foundation for Prader-Willi Research
- Foundation for Prader-Willi Research Canada
- Prader-Willi Syndrome Association (USA)
- Prader-Willi Syndrome (UK)
- Prader-Willi Syndrome Association (UK)
- Prader-Willi Syndrome Association (South Africa)
- SPINE Foundation (Argentina)
- (GeneReview on Prader-Willi syndrome)
Non-Mendelian inheritance: genomic imprinting Chromosome 15 Chromosome 11 Beckwith–Wiedemann syndrome ♀ / Silver–Russell syndrome ♂
Myoclonic dystoniaChromosome 20 Chromosome 6 Transient neonatal diabetes mellitusCategories:- Disability
- Medical conditions related to obesity
- Syndromes
- Genodermatoses
- Autosomal monosomies and deletions
Wikimedia Foundation. 2010.