- Pathogenic fungi
-
Pathogenic fungi are fungi that cause disease in humans or other organisms. The study of pathogenic fungi is referred to as medical mycology. Although fungi are eukaryotic organisms many pathogenic fungi are also microorganisms.[1]
Contents
Candida
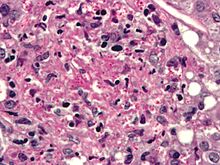
 Candida. Pap test specimen. Pap stain.
Candida. Pap test specimen. Pap stain.
Candida species are important human pathogens that are best known for causing opportunist infections in immunocompromised hosts (e.g. transplant patients, AIDS sufferers, cancer patients). Infections are difficult to treat and can be very serious: 30-40% of systemic infections result in death.[citation needed] The sequencing of the genome of C. albicans and those of several other medically-relevant Candida species has provided a major impetus for Candida comparative and functional genomic analyses. These studies are aiding the development of sensitive diagnostic strategies and novel antifungal therapies.[2]
Aspergillus
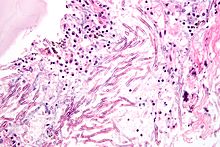 Aspergillosis. H&E stain.
Aspergillosis. H&E stain.
Aerosolized Aspergillus spores are found nearly everywhere so we are routinely and almost constantly exposed to them. Such exposure is a normal part of the human condition and generally poses no adverse health effects. Nevertheless, Aspergillus can and does cause disease in three major ways: through the production of mycotoxins; through induction of allergenic responses; and through localized or systemic infections. With the latter two categories, the immune status of the host is pivotal. Allergies and asthma are thought to be caused by an active host immune response against the presence of fungal spores or hyphae. In contrast, with invasive aspergillosis, the immune system has collapsed and little or no defence can be mounted.[3]
The most common pathogenic species are Aspergillus fumigatus and Aspergillus flavus. Aspergillus flavus produces aflatoxin which is both a toxin and a carcinogen and which can potentially contaminate foods such as nuts. Aspergillus fumigatus and Aspergillus clavatus can cause allergic disease. Some Aspergillus species cause disease on grain crops, especially maize, and synthesize mycotoxins including aflatoxin. Aspergillosis is the group of diseases caused by Aspergillus. The symptoms include fever, cough, chest pain or breathlessness. Usually, only patients with weakened immune systems or with other lung conditions are susceptible.[1][3]:)
Cryptococcus
Cryptococcus neoformans can cause a severe form of meningitis and meningo-encephalitis in patients with HIV infection and AIDS. The majority of Cryptococcus species live in the soil and do not cause disease in humans. Cryptococcus neoformans is the major human and animal pathogen. Cryptococcus laurentii and Cryptococcus albidus have been known to occasionally cause moderate-to-severe disease in human patients with compromised immunity. Cryptococcus gattii is endemic to tropical parts of the continent of Africa and Australia and can cause disease in non-immunocompromised people.[1]
Histoplasma
Histoplasma capsulatum can cause histoplasmosis in humans, dogs and cats. The fungus is most prevalent in the Americas, India and southeastern Asia. It is endemic in certain areas of the United States. Infection is usually due to inhaling contaminated air.
Pneumocystis
Pneumocystis jirovecii (or Pneumocystis carinii) can cause a form of pneumonia in people with weakened immune systems, such as premature children, the elderly, and AIDS patients.[4]
Stachybotrys
Stachybotrys chartarum or "black mold" can cause respiratory damage and severe headaches. It frequently occurs in houses in regions that are chronically damp.
Drug resistance
Treatment with antifungal drugs often results in the appearance of resistant strains of fungi. Various mechanisms leading to resistance have been described. For example, a number of resistant clinical isolates overexpress genes encoding drug efflux pumps. Recent advances in molecular biology have allowed the study of the phenomenon of multi-drug resistance on a genome-wide scale. DNA microarrays are being used to study the expression profiling of pathogenic fungi and proteomics is aiding research in the development of resistance to various antifungal drugs. [5]
Endothermy
Mammalian endothermy and homeothermy are potent nonspecific defenses against most fungi.[6]
See also
External Links
References
- ^ a b c San-Blas G; Calderone RA (editors). (2008). Pathogenic Fungi: Insights in Molecular Biology. Caister Academic Press. ISBN 978-1-904455-32-5. [1]. http://www.horizonpress.com/pat2.
- ^ dEnfert C; Hube B (editors). (2007). Candida: Comparative and Functional Genomics. Caister Academic Press. ISBN 978-1-904455-13-4. [2]. http://www.horizonpress.com/can.
- ^ a b Machida, M; Gomi, K (editors) (2010). Aspergillus: Molecular Biology and Genomics. Caister Academic Press. ISBN 978-1-904455-53-0.
- ^ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 0838585299.
- ^ Waldin et al. (2008). "Genome-wide Approaches to Understand Multi-drug Resistance in Pathogenic Fungi". Pathogenic Fungi: Insights in Molecular Biology. Caister Academic Press. doi:[http://www.horizonpress.com/pat2 ISBN 978-1-904455-32-5]. http://www.horizonpress.com/pat2.
- ^
Infectious diseases · Mycoses and Mesomycetozoea (B35–B49, 110–118) Superficial and
cutaneous
(dermatomycosis):
Tinea=skin;
Piedra (exothrix/
endothrix)=hairBy locationTinea barbae/Tinea capitis (Kerion) · Tinea corporis (Ringworm, Dermatophytid) · Tinea cruris · Tinea manuum · Tinea pedis (Athlete's foot) · Tinea unguium/Onychomycosis (White superficial onychomycosis · Distal subungual onychomycosis · Proximal subungual onychomycosis)
Tinea corporis gladiatorum · Tinea faciei · Tinea imbricata · Tinea incognito · FavusBy organismEpidermophyton floccosum · Microsporum canis · Microsporum audouinii · Trichophyton interdigitale/mentagrophytes · Trichophyton tonsurans · Trichophyton schoenleini · Trichophyton rubrumOtherHortaea werneckii (Tinea nigra) · Piedraia hortae (Black piedra)Subcutaneous,
systemic,
and opportunisticDimorphic
(yeast+mold)Coccidioides immitis/Coccidioides posadasii (Coccidioidomycosis, Disseminated coccidioidomycosis, Primary cutaneous coccidioidomycosis. Primary pulmonary coccidioidomycosis) · Histoplasma capsulatum (Histoplasmosis, Primary cutaneous histoplasmosis, Primary pulmonary histoplasmosis, Progressive disseminated histoplasmosis) · Histoplasma duboisii (African histoplasmosis) · Lacazia loboi (Lobomycosis) · Paracoccidioides brasiliensis (Paracoccidioidomycosis)OtherBlastomyces dermatitidis (Blastomycosis, North American blastomycosis, South American blastomycosis) · Sporothrix schenckii (Sporotrichosis) · Penicillium marneffei (Penicilliosis)Yeast-likeCandida albicans (Candidiasis, Oral, Esophageal, Vulvovaginal, Chronic mucocutaneous, Antibiotic candidiasis, Candidal intertrigo, Candidal onychomycosis, Candidal paronychia, Candidid, Diaper candidiasis, Congenital cutaneous candidiasis, Perianal candidiasis, Systemic candidiasis, Erosio interdigitalis blastomycetica) · C. glabrata · C. tropicalis · C. lusitaniae · Pneumocystis jirovecii (Pneumocystosis, Pneumocystis pneumonia)Mold-likeAspergillus (Aspergillosis, Aspergilloma, Allergic bronchopulmonary aspergillosis, Primary cutaneous aspergillosis) · Exophiala jeanselmei (Eumycetoma) · Fonsecaea pedrosoi/Fonsecaea compacta/Phialophora verrucosa (Chromoblastomycosis) · Geotrichum candidum (Geotrichosis) · Pseudallescheria boydii (Allescheriasis)Entomophthorales
(Entomophthoramycosis)Basidiobolus ranarum (Basidiobolomycosis) · Conidiobolus coronatus/Conidiobolus incongruus (Conidiobolomycosis)Enterocytozoon bieneusi/Encephalitozoon intestinalisMesomycetozoea Ungrouped Alternariosis · Fungal folliculitis · Fusarium (Fusariosis) · Granuloma gluteale infantum · Hyalohyphomycosis · Otomycosis · PhaeohyphomycosisCategories:- Microbiology
- Mycology
- Fungal diseases
Wikimedia Foundation. 2010.