- Membranoproliferative glomerulonephritis
-
Membranoproliferative glomerulonephritis Classification and external resources 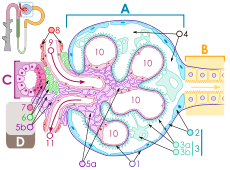
Renal corpuscle. Membranoproliferative glomerulonephritis involves deposits at the intraglomerular mesangium (#5a) which leads to "splitting" of the glomerular basement membrane (#1).ICD-10 N00-N08 with .5 and .6 suffix ICD-9 581.2, 582.2, 583.2 OMIM 609814 305800 DiseasesDB 34457 eMedicine med/887 MeSH D015432 Membranoproliferative glomerulonephritis ("MPGN"), also known as mesangiocapillary glomerulonephritis,[1] is a type of glomerulonephritis caused by deposits in the kidney glomerular mesangium and basement membrane (GBM) thickening,[2] activating complement and damaging the glomeruli.
MPGN accounts for approximately 4% of primary renal causes of nephrotic syndrome in children and 7% in adults.[3]
It should not be confused with membranous glomerulonephritis, a condition in where the basement membrane is thickened, but the mesangium is not.
Contents
Appearance
The GBM is rebuilt on top of the deposits, causing a "tram tracking" appearance under the microscope.[4] Mesangial cellularity is increased.[5]
Type
There are three types of MPGN.
Type I
Type I the most common by far, is caused by immune complexes depositing in the kidney. It is characterised by subendothelial and mesangial immune deposits.
It is believed to be associated with the classical complement pathway.[6]
Type II
Type II (sometimes also called "dense deposit disease"[7]) is similar to type I. However, it is believed to be associated with the alternative complement pathway.[8][9]
Spontaneous remissions of MPGN II are rare, approximately half of those affected with MPGN II will progress to end stage renal disease within 10 years.[10]
In many cases, people with MPGN II can develop drusen which is caused by same deposits within the Bruch's membrane beneath the retinal pigment epithelium (RPE) layer of the eye. Over time vision can deteriorate and subretinal neovascular membranes, macular detachment, and central serous retinopathy develop.[11]
Recent research suggests that dense deposit disease may not be a membranoproliferative glomerulonephritis subtype.[12]
Type III
Type III is very rare, it is characterized by a mixture of subepithelial deposits and the typical pathological findings of Type I disease.
A candidate gene has been identified on chromosome 1.[13]
Complement component 3 is seen under immunofluorescence.[14]
References
- ^ Colville D, Guymer R, Sinclair RA, Savige J (August 2003). "Visual impairment caused by retinal abnormalities in mesangiocapillary (membranoproliferative) glomerulonephritis type II ("dense deposit disease")". Am. J. Kidney Dis. 42 (2): E2–5. doi:10.1016/S0272-6386(03)00665-6. PMID 12900843. http://linkinghub.elsevier.com/retrieve/pii/S0272638603006656.
- ^ "membranoproliferative glomerulonephritis" at Dorland's Medical Dictionary
- ^ Habib R, Gubler MC, Loirat C, Mäiz HB, Levy M (1975). "Dense deposit disease: a variant of membranoproliferative glomerulonephritis". Kidney Int. 7 (4): 204–15. doi:10.1038/ki.1975.32. PMID 1095806.
- ^ "Membranoproliferative_glomerulonephritis_type_I of the Kidney". http://pathweb.uchc.edu/eAtlas/Code/1510.HTM. Retrieved 2008-11-25.
- ^ "Renal Pathology". http://library.med.utah.edu/WebPath/RENAHTML/RENAL097.html. Retrieved 2008-11-25.
- ^ West CD, McAdams AJ (March 1998). "Glomerular paramesangial deposits: association with hypocomplementemia in membranoproliferative glomerulonephritis types I and III". Am. J. Kidney Dis. 31 (3): 427–34. doi:10.1053/ajkd.1998.v31.pm9506679. PMID 9506679. http://linkinghub.elsevier.com/retrieve/pii/S0272638698000651.
- ^ "Final Diagnosis -- Case 148". http://path.upmc.edu/cases/case148/dx.html. Retrieved 2008-11-25.
- ^ Rose KL, Paixao-Cavalcante D, Fish J, et al. (February 2008). "Factor I is required for the development of membranoproliferative glomerulonephritis in factor H-deficient mice". J. Clin. Invest. 118 (2): 608–18. doi:10.1172/JCI32525. PMC 2200299. PMID 18202746. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2200299.
- ^ Licht C, Schlötzer-Schrehardt U, Kirschfink M, Zipfel PF, Hoppe B (January 2007). "MPGN II--genetically determined by defective complement regulation?". Pediatr. Nephrol. 22 (1): 2–9. doi:10.1007/s00467-006-0299-8. PMID 17024390.
- ^ Swainson CP, Robson JS, Thomson D, MacDonald MK (1983). "Mesangiocapillary glomerulonephritis: a long-term study of 40 cases". J. Pathol. 141 (4): 449–68. doi:10.1002/path.1711410404. PMID 6363655.
- ^ Colville D, Guymer R, Sinclair RA, Savige J (2003). "Visual impairment caused by retinal abnormalities in mesangiocapillary (membranoproliferative) glomerulonephritis type II ("dense deposit disease")". Am. J. Kidney Dis. 42 (2): E2–5. doi:10.1016/S0272-6386(03)00665-6. PMID 12900843. http://linkinghub.elsevier.com/retrieve/pii/S0272638603006656.
- ^ Patrick D Walker, Franco Ferrario, Kensuke Joh, Stephen M Bonsib (2007). "Dense deposit disease is not a membranoproliferative glomerulonephritis". Modern Pathology. 20 (6): 605–616. doi:10.1038/modpathol.3800773. PMID 17396142. http://www.nature.com/modpathol/journal/v20/
- ^ Neary JJ, Conlon PJ, Croke D, et al. (August 2002). "Linkage of a gene causing familial membranoproliferative glomerulonephritis type III to chromosome 1". J. Am. Soc. Nephrol. 13 (8): 2052–7. doi:10.1097/01.ASN.0000022006.49966.F8. PMID 12138136. http://jasn.asnjournals.org/cgi/pmidlookup?view=long&pmid=12138136.
- ^ name="pmid12087587">Neary J, Dorman A, Campbell E, Keogan M, Conlon P (July 2002). "Familial membranoproliferative glomerulonephritis type III". Am. J. Kidney Dis. 40 (1): E1. doi:10.1053/ajkd.2002.33932. PMID 12087587. http://linkinghub.elsevier.com/retrieve/pii/S0272638602000306.
External links
- Glomerulonephritis, Membranoproliferative Types I,II,III - overview, workup, treatment
- GeneReviews/NCBI/NIH/UW entry on Dense Deposit Disease / Membranoproliferative Glomerulonephritis Type II
Urinary system · Pathology · Urologic disease / Uropathy (N00–N39, 580–599) Abdominal Primarily
nephrotic.3 Mesangial proliferative · .4 Endocapillary proliferative .5/.6 Membranoproliferative/mesangiocapillaryBy conditionType III RPG/Pauci-immuneTubulopathy/
tubulitisAny/allAny/allGeneral syndromesOtherUreterPelvic UrethraUrethritis (Non-gonococcal urethritis) · Urethral syndrome · Urethral stricture/Meatal stenosis · Urethral caruncleAny/all Obstructive uropathy · Urinary tract infection · Retroperitoneal fibrosis · Urolithiasis (Bladder stone, Kidney stone, Renal colic) · Malacoplakia · Urinary incontinence (Stress, Urge, Overflow)Categories:- Nephrology
- Disease stubs
Wikimedia Foundation. 2010.
