- Moxonidine
-
Moxonidine 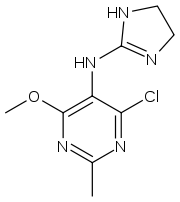
Systematic (IUPAC) name 4-chloro-N-(4,5-dihydro-1H-imidazol-2-yl)-
6-methoxy-2-methylpyrimidin-5-amineClinical data AHFS/Drugs.com International Drug Names Pregnancy cat. B3(AU) Legal status POM (UK) Routes Oral Pharmacokinetic data Bioavailability 88% Half-life 2.2 hours Excretion Renal Identifiers CAS number 75438-57-2 
ATC code C02AC05 PubChem CID 4810 ChemSpider 4645 
UNII CC6X0L40GW 
KEGG D05087 
ChEMBL CHEMBL19236 
Chemical data Formula C9H12ClN5O Mol. mass 241.677 g/mol SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Moxonidine (INN) (
 /mɒkˈsɒnɪdiːn/) is a new generation centrally acting antihypertensive drug licensed for the treatment of mild to moderate essential hypertension. It may have a role when thiazides, beta-blockers, ACE inhibitors and calcium channel blockers are not appropriate or have failed to control blood pressure. In addition, it demonstrates favourable effects on parameters of the insulin resistance syndrome, apparently independent of blood pressure reduction. It is manufactured by Solvay Pharmaceuticals under the brand name Physiotens.
/mɒkˈsɒnɪdiːn/) is a new generation centrally acting antihypertensive drug licensed for the treatment of mild to moderate essential hypertension. It may have a role when thiazides, beta-blockers, ACE inhibitors and calcium channel blockers are not appropriate or have failed to control blood pressure. In addition, it demonstrates favourable effects on parameters of the insulin resistance syndrome, apparently independent of blood pressure reduction. It is manufactured by Solvay Pharmaceuticals under the brand name Physiotens.Contents
Mechanism of actions
Moxonidine is a selective agonist at the imidazoline receptor subtype 1 (I1). This receptor subtype is found in both the rostral ventro-lateral pressor and ventromedial depressor areas of the medulla oblongata. Moxonidine therefore causes a decrease in sympathetic nervous system activity and, therefore, a decrease in blood pressure.
Compared to the older central-acting antihypertensives, moxonidine binds with much greater affinity to the imidazoline I1-receptor than to the α2-receptor. In contrast, clonidine binds to both receptors with equal affinity.
In addition, moxonidine may also promote sodium excretion, improve insulin resistance and glucose tolerance and protect against hypertensive target organ damage, such as kidney disease and cardiac hypertrophy.
Pharmacodynamic properties
Effects on insulin resistance
In all animal models of insulin resistance, moxonidine had striking effects on the development of insulin resistance, hyperinsulinaemia and impaired glucose homeostasis. Given the importance of insulin resistance as a risk factor for cardiovascular disease, it is of considerable relevance that it has been shown to improve insulin sensitivity.
Based on animal models, it has demonstrated that moxonidine is capable of:
- normalising plasma insulin levels
- improving glucose uptake in peripheral cells
- lowering lipid levels
- decreasing food intake and reducing weight gain in obese animals.
Renal function
Evidence is accumulating to show that sympathetic overactivity is substantially involved in the development and progression of chronic renal failure, contributing to a poor overall cardiovascular prognosis. Moxonidine has been shown to reduce structural renal damage in various models of renal failure.
Cardiac structure
In spontaneously hypertensive rats, moxonidine significantly reduced total heart weight, left ventricular weight and the ratio of ventricular weight to body weight compared with an untreated control group.
Safety pharmacology
Routine toxicology studies have provided no evidence that moxonidine has any teratogenic, mutagenic or carcinogenic potential. No evidence has been found of serious adverse effects on organs or organ systems, and the drug has not been shown to have deleterious effects on perinatal or postnatal growth and development.
Cautions
Moxonidine should be avoided in patients with moderate to severe renal impairment. Abrupt discontinuation of the drug should also be avoided. If concomitant treatment with a beta blocker has to be stopped, the beta blocker should be discontinued first, then moxonidine after a few days.
Drug interactions
Concomitant administration of moxonidine and a thiazide diuretic such as hydrochlorothiazide is not indicated, as both drugs' hypotensive effects may be enhanced.
Contra-indications
It is contraindicated if there has been a past history of angioedema; heart conduction disorders (e.g. sick sinus syndrome, second- or third-degree heart block); bradycardia; severe heart failure or coronary artery disease, severe liver or renal impairment. Also: Raynaud's syndrome, intermittent claudication, epilepsy, depression, Parkinson's disease, glaucoma. Use in pregnancy is discouraged. Moxonidine passes into breast milk.
Excess mortality has been seen in patients with symptomatic heart failure.[1]
Side-effects
Noteworthy side effects include dry mouth, headache, fatigue, dizziness, nausea, sleep disturbances (rarely sedation), asthenia, vasodilatation, and rarely, skin reactions.
References
- ^ Cohn J et al. (2003). "Adverse mortality effect of central sympathetic inhibition with sustained-release moxonidine in patients with heart failure (MOXCON)". Eur J Heart Fail 5 (5): 659–67. doi:10.1016/S1388-9842(03)00163-6. PMID 14607206.
Sympatholytic (and closely related) antihypertensives (C02) Sympatholytics
(antagonize α-adrenergic
vasoconstriction)CentralAdrenergic release inhibitorsBethanidine • Bretylium • Debrisoquine • Guanadrel • Guanazodine • Guanethidine • Guanoclor • Guanoxan • Guanazodine • Guanoxabenz • GuanoxanImidazoline receptor agonistMoxonidine • RilmenidineMecamylamine • Pentolinium • TrimethaphanPeripheralIndirectTyrosine hydroxylase inhibitorDirectNon-selective α blockerOther antagonists Endothelin antagonist (for PH)Categories:- Antihypertensive agents
- Imidazolines
- Pyrimidines
- Organochlorides
- Phenol ethers
Wikimedia Foundation. 2010.
