- Paget's disease of bone
-
For other diseases named after Paget, see Paget's disease (disambiguation).
Paget's disease of bone Classification and external resources 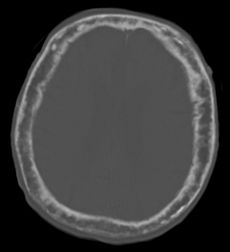
"This 92 year-old male patient presented for assessment of acute hemiparesis. An incidental finding was marked thickening of the calvarium. The diploic space is widened and there are ill-defined sclerotic and lucent areas throughout. The cortex is thickened and irregular. The findings probably correspond to the “cotton wool spots” seen on plain films in the later stages of Paget’s disease." (dr Dawes)ICD-10 M88 ICD-9 731.0 OMIM 602080 DiseasesDB 9479 MedlinePlus 000414 eMedicine med/2998 radio/514 pmr/98 MeSH D010001 Paget's disease is a chronic disorder that can result in enlarged and misshapen bones. The excessive breakdown and formation of bone tissue causes affected bone to weaken, resulting in pain, misshapen bones, fractures, and arthritis in the joints near the affected bones. Paget's disease typically is localized, affecting just one or a few bones, as opposed to osteoporosis, for example, which affects all the bones in the body. Decisions about treating Paget's disease can be complicated because: 1) no two people are affected in exactly the same way by the disease, and 2) it is sometimes difficult to predict whether a person with Paget's disease who shows no signs of the disorder will develop symptoms or complications, such as a bone fracture, at a later date. Although there is no cure for Paget's disease, medications (bisphosphonates and calcitonin) can help control the disorder and lessen pain and other symptoms. Paget's disease experts recommend that these medications be taken by people with Paget's disease who: have bone pain, headache, back pain, or a nerve-related symptom (such as "shooting" pains in the leg) that is directly associated with the disease; have elevated levels of serum alkaline phosphatase (SAP) in their blood; display evidence that a bone fracture will occur; require pretreatment therapy for affected bones that require surgery; have active symptoms in the skull, long bones, or vertebrae (spine); have the disease in bones located next to major joints, placing them at risk of developing osteoarthritis; develop a rare condition called hypercalcemia that occurs when a person with several bones affected by Paget's disease and a high SAP level is immobilized.
Today's medications, especially when started before complications begin, are often successful in controlling the disorder. Paget's disease is rarely diagnosed in people less than 40 years of age. Women are more commonly affected than men.[1] Prevalence of Paget's disease ranges from 1.5 to 8.0 percent, depending on age and country of residence. Prevalence of familial Paget's disease (where more than one family member has the disease) ranges from 10 to 40 percent in different parts of the world.[citation needed] Because early diagnosis and treatment is important, after age 40, siblings and children of someone with Paget's disease may wish to have an alkaline phosphatase blood test every two or three years. If the alkaline phosphatase level is above normal, other tests such as a bone-specific alkaline phosphatase test, bone scan, or X-ray can be performed.
Contents
Etymology
The term osteitis deformans is now considered technically incorrect, and the preferred term is osteodystrophia deformans.
Causes
Viral
Paget's disease may be caused by a slow virus infection (i.e., paramyxoviruses) present for many years before symptoms appear.
- Respiratory syncytial virus[7]
Contamination has been suggested to have played a role in producing past positive results.[8]
Genetic
There is also a hereditary factor.[9][10] Associations include:
Name OMIM Locus Gene PDB1 167250 6p ? PDB2 18q22.1 RANK PDB3 5q35 SQSTM1 PDB4 606263 5q31[11] ? Pathogenesis
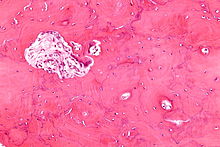 Micrograph showing Paget's disease of the bone with the characteristic jigsaw puzzle-like/mosaic pattern, H&E stain
Micrograph showing Paget's disease of the bone with the characteristic jigsaw puzzle-like/mosaic pattern, H&E stain
The pathogenesis of Paget's disease is described in 3 stages, which are:
i. Osteoclastic activity
ii. Mixed osteoclastic-osteoblastic activity
iii. Exhaustive (burnt out) stageInitially, there is a marked increase in the rate of bone resorption at localized areas caused by large and numerous osteoclasts. These localized areas of osteolysis are seen radiologically as an advancing lytic wedge in long bones or osteoporosis circumscripta in the skull. The osteolysis is followed by a compensatory increase in bone formation induced by osteoblasts recruited to the area. This is associated with accelerated deposition of lamellar bone in a disorganized fashion. This intense cellular activity produces a chaotic picture of trabecular bone ("mosaic" pattern), rather than the normal linear lamellar pattern. The resorbed bone is replaced and the marrow spaces are filled by an excess of fibrous connective tissue with a marked increase in blood vessels, causing the bone to become hypervascular. The bone hypercellularity may then diminish, leaving a dense "pagetic bone," also known as burned-out Paget's disease.
Sir James Paget first suggested the disease was due to an inflammatory process. New evidence suggests he may have been correct and that a paramyxovirus infection is the underlying cause of Paget's disease. No infectious virus has yet been isolated as a causative agent, however, and other evidence suggests an intrinsic hyperresponsive reaction to vitamin D and RANK ligand is the cause. Further research is therefore necessary.[12]
Symptoms
Many patients do not know they have Paget's disease because they have a mild case with no symptoms. Sometimes, symptoms may be confused with those of arthritis or other disorders. In other cases, the diagnosis is made only after complications have developed. Symptoms can include:
Diagnosis
Paget's disease may be diagnosed using one or more of the following tests:
- Pagetic bone has a characteristic appearance on X-rays. A skeletal survey is therefore indicated.
- An elevated level of alkaline phosphatase in the blood in combination with normal calcium, phosphate, and aminotransferase levels in an elderly patient are suggestive of Paget's disease.
- Bone scans are useful in determining the extent and activity of the condition. If a bone scan suggests Paget's disease, the affected bone(s) should be X-rayed to confirm the diagnosis.
Comparison of bone pathology Phosphate Alkaline phosphatase Parathyroid hormone Comments Osteoporosis unaffected unaffected variable unaffected decreased bone mass Osteopetrosis unaffected unaffected elevated unaffected thick dense bones also known as marble bone Osteomalacia and rickets decreased decreased variable elevated soft bones Osteitis fibrosa cystica elevated decreased elevated elevated brown tumors Paget's disease of bone unaffected unaffected variable (depending on stage of disease) unaffected abnormal bone architecture Prognosis
The outlook is generally good, particularly if treatment is given before major changes in the affected bones have occurred. Any bone or bones can be affected, but Paget's disease occurs most frequently in the spine, skull, pelvis, femur, and lower legs. In general, symptoms progress slowly, and the disease does not spread to normal bones. Treatment can control Paget's disease and lessen symptoms, but is not a cure. Osteogenic sarcoma, a form of bone cancer, is an extremely rare complication that occurs in less than one percent of all patients.
Associated medical conditions
Paget's disease may lead to other medical conditions, including:
- Arthritis may be caused by bowing of long bones in the leg, distorting alignment and increasing pressure on nearby joints. In addition, pagetic bone may enlarge, causing joint surfaces to undergo excessive wear. In these cases, pain may be due to a combination of Paget's disease and osteoarthritis.
- Loss of hearing in one or both ears may occur when Paget's disease affects the skull and the bone that surrounds the inner ear. Treating the Paget's disease may slow or stop hearing loss. Hearing aids may also help.
- Cardiovascular disease can result from severe Paget's disease (i.e. with more than 15% skeletal involvement). Arteriovenous connections can often form in the bone, and so the heart has to work harder (pump more blood) to ensure adequate oxygen supply to the tissues. This increase in cardiac output can lead to calcification of the aortic valve, and the resulting aortic stenosis causes left ventricular hypertrophy and eventually high-output congestive failure.
- Kidney stones are somewhat more common in patients with Paget's disease.
- Pagetic bone can cause nervous system problems, such as pressure on the brain, spinal cord, or nerves, and reduced blood flow to the brain and spinal cord.
- Rarely, Paget's disease is associated with the development of osteosarcoma (malignant tumor of bone). When there is a sudden onset or worsening of pain, sarcoma should be considered.
- When Paget's disease affects the facial bones, the teeth may become loose. Disturbance in chewing may occur.
- Rarely, when the skull is involved, the nerves to the eye may be affected, causing some loss of vision.
- Angioid streaks may develop, possibly as a result of calcification of collagen or other pathological deposition.
Paget's disease is not associated with osteoporosis. Although Paget's disease and osteoporosis can occur in the same patient, they are different disorders. Despite their marked differences, several treatments for Paget's disease are also used to treat osteoporosis.
Treatment
Endocrinologists (internists who specialize in hormonal and metabolic disorders), rheumatologists (internists who specialize in joint and muscle disorders), orthopedic surgeons, neurologists, and otolaryngologists are generally knowledgeable about treating Paget's disease, and may be called upon to evaluate specialized symptoms.
Drug therapy
The goal of treatment is to relieve bone pain and prevent the progression of the disease. The U.S. Food and Drug Administration has approved the following treatments for Paget's disease:
Bisphosphonates
Five bisphosphonates are currently available. In general, the most commonly prescribed are: risedronic acid (Actonel), alendronic acid (Fosamax) and pamidronic acid (Aredia). Etidronic acid (Didronel) and other bisphosphonates may be appropriate therapies for selected patients, but are less commonly used. As a rule, bisphosphonate tablets should be taken with 200-250 mL (6–8 oz) of tap water (not from a source with high mineral content) on an empty stomach. None of these drugs should be used by people with severe kidney disease.
- Etidronate disodium (Didronel) in tablet form is available in 200–400 mg doses. The approved regimen is once daily for six months; the higher dose (400 mg) is more commonly used. No food, beverage, or medications should be consumed for two hours before and after taking. The course should not exceed six months, but repeat courses can be given after rest periods, preferably of three to six months duration.
- Pamidronate disodium (Aredia) in intravenous form: the approved regimen uses a 30 mg infusion over four hours on each of three consecutive days, but a more commonly used regimen is 60 mg over two to four hours for two or more consecutive or nonconsecutive days.
- Alendronate sodium (Fosamax) is given as tablets of 40 mg once daily for six months; patients should wait at least 30 minutes after taking before eating any food, drinking anything other than tap water, taking any medication, or lying down (patient may sit).
- Tiludronate disodium (Skelid) in two tablets of 200 mg are taken once daily for three months; they may be taken any time of day, as long as there is a period of two hours before and after resuming food, beverages, and medications.
- Risedronate sodium (Actonel) as a 30 mg tablet taken once daily for 2 months is the prescribed regimen; patients should wait at least 30 minutes after taking before eating any food, drinking anything other than tap water, taking any medication, or lying down (patient may sit).
- Zoledronic acid (Reclast, Aclasta) is given as an intravenous infusion; a single dose (5 mg over 15 minutes) is effective for two years.
Calcitonin
- Miacalcin is administered by injection; 50 to 100 units daily or three times per week for 6–18 months. Repeat courses can be given after brief rest periods. Miacalcin may be appropriate for certain patients, but is seldom used. The nasal spray form of this drug is not approved for the treatment of Paget's disease.
Surgery
Medical therapy prior to surgery helps to decrease bleeding and other complications. Patients who are having surgery should discuss treatment with their physician. There are generally three major complications of Paget's disease for which surgery may be recommended.
- Fractures — Surgery may allow fractures to heal in a better position.
- Severe degenerative arthritis — If disability is severe and medication and physical therapy are no longer helpful, joint replacement of the hips and knees may be considered.
- Bone deformity — Cutting and realignment of pagetic bone (osteotomy) may help painful weight bearing joints, especially the knees.
Complications resulting from enlargement of the skull or spine may injure the nervous system. However, most neurologic symptoms, even those that are moderately severe, can be treated with medication and do not require neurosurgery.
Diet and exercise
In general, patients with Paget's disease should receive 1000–1500 mg of calcium, adequate sunshine, and at least 400 units of vitamin D daily. This is especially important in patients being treated with bisphosphonates; however, taking oral bisphosphonates should be separated from taking calcium by at least two hours, because the calcium can inhibit the absorption of the bisphosphonate. Patients with a history of kidney stones should discuss calcium and vitamin D intake with their physicians.
Exercise is very important in maintaining skeletal health, avoiding weight gain, and maintaining joint mobility. Since undue stress on affected bones should be avoided, patients should discuss any exercise program with their physicians before beginning.
References in pop culture
- C.S.I. New York: A murder victim in Season 2 episode "Youngblood" was afflicted with Paget's disease.
- Retired Boston Red Sox center fielder Dom DiMaggio suffered from Paget's disease and served as a member of the board of directors of the Paget Foundation.[13]
- Robot Chicken:Season 5:Kramer vs. Showgirls:The 90s Revisited: We learn that "Brain" of Pinky and the Brain was not a genius but his enlarged cranium is the result of Paget's disease, which has also left him blind.[14]
- Egil, the main character in Egils Saga is speculated to have suffered from this disease: he is described as being abnormally large and strong, and after death his skull was said to have been covered in ridges.
References
- ^ Kumar and Clark, Parveen and Micheal (2009). [Link to this page: http://www.studentconsult.com/content/default.cfm?ISBN=9780702029936&ID=HC010583 Welcome to Kumar and Clark's Clinical Medicine 7E]. Elsiver. pp. 565. ISBN 978-0-7020-2993-6. Link to this page: http://www.studentconsult.com/content/default.cfm?ISBN=9780702029936&ID=HC010583.
- ^ Friedrichs WE, Reddy SV, Bruder JM et al. (January 2002). "Sequence analysis of measles virus nucleocapsid transcripts in patients with Paget's disease". J. Bone Miner. Res. 17 (1): 145–51. doi:10.1359/jbmr.2002.17.1.145. PMID 11771661.
- ^ Baslé MF, Fournier JG, Rozenblatt S, Rebel A, Bouteille M (May 1986). "Measles virus RNA detected in Paget disease bone tissue by in situ hybridization". J. Gen. Virol. 67 ( Pt 5) (5): 907–13. doi:10.1099/0022-1317-67-5-907. PMID 3701300. http://vir.sgmjournals.org/cgi/pmidlookup?view=long&pmid=3701300.
- ^ Matthews BG, Afzal MA, Minor PD et al. (April 2008). "Failure to detect measles virus ribonucleic acid in bone cells from patients with Paget's disease". J. Clin. Endocrinol. Metab. 93 (4): 1398–401. doi:10.1210/jc.2007-1978. PMID 18230662. http://jcem.endojournals.org/cgi/pmidlookup?view=long&pmid=18230662.
- ^ Hoyland JA, Dixon JA, Berry JL, Davies M, Selby PL, Mee AP (May 2003). "A comparison of in situ hybridisation, reverse transcriptase-polymerase chain reaction (RT-PCR) and in situ-RT-PCR for the detection of canine distemper virus RNA in Paget disease". J. Virol. Methods 109 (2): 253–9. doi:10.1016/S0166-0934(03)00079-X. PMID 12711070. http://linkinghub.elsevier.com/retrieve/pii/S016609340300079X.
- ^ Gordon MT, Anderson DC, Sharpe PT (1991). "Canine distemper virus localised in bone cells of patients with Paget disease". Bone 12 (3): 195–201. doi:10.1016/8756-3282(91)90042-H. PMID 1910961.
- ^ Mills BG, Singer FR, Weiner LP, Holst PA (February 1981). "Immunohistological demonstration of respiratory syncytial virus antigens in Paget disease of bone". Proc. Natl. Acad. Sci. U.S.A. 78 (2): 1209–13. doi:10.1073/pnas.78.2.1209. PMC 319977. PMID 6940136. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=319977.
- ^ Ralston SH, Afzal MA, Helfrich MH et al. (April 2007). "Multicenter blinded analysis of RT-PCR detection methods for paramyxoviruses in relation to Paget disease of bone". J. Bone Miner. Res. 22 (4): 569–77. doi:10.1359/jbmr.070103. PMID 17227218. http://www.jbmronline.com/doi/abs/10.1359/jbmr.070103?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov.[dead link]
- ^ Ralston SH, Langston AL, Reid IR (July 2008). "Pathogenesis and management of Paget disease of bone". Lancet 372 (9633): 155–63. doi:10.1016/S0140-6736(08)61035-1. PMID 18620951. http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(08)61035-1.
- ^ Whyte MP (April 2006). "Paget disease of bone and genetic disorders of RANKL/OPG/RANK/NF-kappaB signaling". Ann. N. Y. Acad. Sci. 1068: 143–64. doi:10.1196/annals.1346.016. PMID 16831914. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0077-8923&date=2006&volume=1068&spage=143.
- ^ Laurin N, Brown JP, Lemainque A et al. (September 2001). "Paget Disease of Bone: Mapping of Two Loci at 5q35-qter and 5q31". Am. J. Hum. Genet. 69 (3): 528–43. doi:10.1086/322975. PMC 1235483. PMID 11473345. http://linkinghub.elsevier.com/retrieve/pii/S0002-9297(07)61164-1.
- ^ Basic Pathology, Kumar Abbas Fausto Mitchell, Saunders Elsevier
- ^ http://www.paget.org/Paget25thBook-ForWeb.pdf
- ^ http://robotchicken.wikia.com/wiki/The_90's_Revisited
Osteochondropathy (M80–M94, 730–733) Osteopathies endocrine bone disease: Osteitis fibrosa cystica (Brown tumor)infectious bone disease: Osteomyelitis (Sequestrum, Involucrum) · Sesamoiditis · Brodie abscess · PeriostitisBone density
and structureDensity / metabolic bone diseaseContinuity of boneOtherFibrous dysplasia (Monostotic, Polyostotic) · Skeletal fluorosis · bone cyst (Aneurysmal bone cyst) · Hyperostosis (Infantile cortical hyperostosis) · Osteosclerosis (Melorheostosis)OtherPaget's disease of bone · Algoneurodystrophy · Hypertrophic pulmonary osteoarthropathy · Nonossifying fibromaChondropathies OtherBoth lower limb: hip (Legg–Calvé–Perthes syndrome) · tibia (Osgood-Schlatter disease, Blount's disease) · foot (Köhler disease, Sever's disease)Categories:- Osteopathies
Wikimedia Foundation. 2010.
