- Complications of diabetes mellitus
-
Diabetes complication Classification and external resources ICD-10 E10-E14 ICD-9 250.1-250.9 MeSH D048909 The complications of diabetes mellitus are far less common and less severe in people who have well-controlled blood sugar levels.[1][2]
Wider health problems accelerate the deleterious effects of diabetes. These include smoking, elevated cholesterol levels, obesity, high blood pressure, and lack of regular exercise.
Contents
Acute
Diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is an acute and dangerous complication that is always a medical emergency. Low insulin levels cause the liver to turn to ketone for fuel (ie, ketosis); ketone bodies are intermediate substrates in that metabolic sequence. This is normal when periodic, but can become a serious problem if sustained. Elevated levels of ketone bodies in the blood decrease the blood's pH, leading to DKA. On presentation at hospital, the patient in DKA is typically dehydrated, and breathing rapidly and deeply. Abdominal pain is common and may be severe. The level of consciousness is typically normal until late in the process, when lethargy may progress to coma. Ketoacidosis can easily become severe enough to cause hypotension, shock, and death. Urine analysis will reveal significant levels of ketone bodies (which have exceeded their renal threshold blood levels to appear in the urine, often before other overt symptoms). Prompt, proper treatment usually results in full recovery, though death can result from inadequate or delayed treatment, or from complications (e.g., brain edema). DKA is always a medical emergency and requires medical attention. Ketoacidosis is much more common in type 1 diabetes than type 2.
Hyperglycemia hyperosmolar state
Hyperosmolar nonketotic state (HNS) is an acute complication sharing many symptoms with DKA, but an entirely different origin and different treatment. A person with very high (usually considered to be above 300 mg/dl (16 mmol/L)) blood glucose levels, water is osmotically drawn out of cells into the blood and the kidneys eventually begin to dump glucose into the urine. This results in loss of water and an increase in blood osmolarity. If fluid is not replaced (by mouth or intravenously), the osmotic effect of high glucose levels, combined with the loss of water, will eventually lead to dehydration. The body's cells become progressively dehydrated as water is taken from them and excreted. Electrolyte imbalances are also common and are always dangerous. As with DKA, urgent medical treatment is necessary, commonly beginning with fluid volume replacement. Lethargy may ultimately progress to a coma, though this is more common in type 2 diabetes than type 1.[citation needed]
Hypoglycemia
Hypoglycemia, or abnormally low blood glucose, is an acute complication of several diabetes treatments. It is rare otherwise, either in diabetic or non-diabetic patients. The patient may become agitated, sweaty, weak, and have many symptoms of sympathetic activation of the autonomic nervous system resulting in feelings akin to dread and immobilized panic. Consciousness can be altered or even lost in extreme cases, leading to coma, seizures, or even brain damage and death. In patients with diabetes, this may be caused by several factors, such as too much or incorrectly timed insulin, too much or incorrectly timed exercise (exercise decreases insulin requirements) or not enough food (specifically glucose containing carbohydrates). The variety of interactions makes cause identification difficult in many instances.
It is more accurate to note that iatrogenic hypoglycemia is typically the result of the interplay of absolute (or relative) insulin excess and compromised glucose counterregulation in type 1 and advanced type 2 diabetes. Decrements in insulin, increments in glucagon, and, absent the latter, increments in epinephrine are the primary glucose counterregulatory factors that normally prevent or (more or less rapidly) correct hypoglycemia. In insulin-deficient diabetes (exogenous) insulin levels do not decrease as glucose levels fall, and the combination of deficient glucagon and epinephrine responses causes defective glucose counterregulation.
Furthermore, reduced sympathoadrenal responses can cause hypoglycemia unawareness. The concept of hypoglycemia-associated autonomic failure (HAAF) in diabetes posits that recent incidents of hypoglycemia causes both defective glucose counterregulation and hypoglycemia unawareness. By shifting glycemic thresholds for the sympathoadrenal (including epinephrine) and the resulting neurogenic responses to lower plasma glucose concentrations, antecedent hypoglycemia leads to a vicious cycle of recurrent hypoglycemia and further impairment of glucose counterregulation. In many cases (but not all), short-term avoidance of hypoglycemia reverses hypoglycemia unawareness in affected patients, although this is easier in theory than in clinical experience.
In most cases, hypoglycemia is treated with sugary drinks or food. In severe cases, an injection of glucagon (a hormone with effects largely opposite to those of insulin) or an intravenous infusion of dextrose is used for treatment, but usually only if the person is unconscious. In any given incident, glucagon will only work once as it uses stored liver glycogen as a glucose source; in the absence of such stores, glucagon is largely ineffective. In hospitals, intravenous dextrose is often used.
Diabetic coma
Diabetic coma is a medical emergency in which a person with diabetes mellitus is comatose (unconscious) because of one of the acute complications of diabetes:
- Severe diabetic hypoglycemia
- Diabetic ketoacidosis advanced enough to result in unconsciousness from a combination of severe hyperglycemia, dehydration and shock, and exhaustion
- Hyperosmolar nonketotic coma in which extreme hyperglycemia and dehydration alone are sufficient to cause unconsciousness.
In most medical contexts, the term diabetic coma refers to the diagnostical dilemma posed when a physician is confronted with an unconscious patient about whom nothing is known except that he has diabetes. An example might be a physician working in an emergency department who receives an unconscious patient wearing a medical identification tag saying DIABETIC. Paramedics may be called to rescue an unconscious person by friends who identify him as diabetic. Brief descriptions of the three major conditions are followed by a discussion of the diagnostic process used to distinguish among them, as well as a few other conditions which must be considered.
An estimated 2 to 15 percent of diabetics will suffer from at least one episode of diabetic coma in their lifetimes as a result of severe hypoglycemia.
Respiratory infections
The immune response is impaired in individuals with diabetes mellitus. Cellular studies have shown that hyperglycemia both reduces the function of immune cells and increases inflammation. The vascular effects of diabetes also tend to alter lung function, all of which leads to an increase in susceptibility to respiratory infections such as pneumonia and influenza among individuals with diabetes. Several studies also show diabetes associated with a worse disease course and slower recovery from respiratory infections.[3]
Chronic
Chronic elevation of blood glucose level leads to damage of blood vessels (angiopathy). The endothelial cells lining the blood vessels take in more glucose than normal, since they do not depend on insulin. They then form more surface glycoproteins than normal, and cause the basement membrane to grow thicker and weaker. In diabetes, the resulting problems are grouped under "microvascular disease" (due to damage to small blood vessels) and "macrovascular disease" (due to damage to the arteries).
However, some research challenges the theory of hyperglycemia as the cause of diabetic complications. The fact that 40% of diabetics who carefully control their blood sugar nevertheless develop neuropathy,[4] and that some of those with good blood sugar control still develop nephropathy,[5] requires explanation. It has been discovered that the serum of diabetics with neuropathy is toxic to nerves even if its blood sugar content is normal.[6] Recent research suggests that in type 1 diabetics, the continuing autoimmune disease which initially destroyed the beta cells of the pancreas may also cause retinopathy,[7] neuropathy,[8] and nephropathy.[9] One researcher has even suggested that retinopathy may be better treated by drugs to suppress the abnormal immune system of diabetics than by blood sugar control.[10] The familial clustering of the degree and type of diabetic complications[11] indicates that genetics may also play a role in causing complications such as diabetic retinopathy.[12] and nephropathy[13] Non-diabetic offspring of type 2 diabetics have been found to have increased arterial stiffness and neuropathy despite normal blood glucose levels,[14] and elevated enzyme levels associated with diabetic renal disease have been found in non-diabetic first-degree relatives of diabetics.[15][16] Even rapid tightening of blood glucose levels has been shown to worsen rather than improve diabetic complications, though it has usually been held that complications would improve over time with more normal blood sugar, provided this could be maintained.[17] However, one study continued for 41 months found that the initial worsening of complications from improved glucose control was not followed by the expected improvement in the complications.[18]
The damage to small blood vessels leads to a microangiopathy, which can cause one or more of the following:
- Diabetic cardiomyopathy, damage to the heart, leading to diastolic dysfunction and eventually heart failure.
- Diabetic nephropathy, damage to the kidney which can lead to chronic renal failure, eventually requiring dialysis. Diabetes mellitus is the most common cause of adult kidney failure worldwide in the developed world.
- Diabetic neuropathy, abnormal and decreased sensation, usually in a 'glove and stocking' distribution starting with the feet but potentially in other nerves, later often fingers and hands. When combined with damaged blood vessels this can lead to diabetic foot (see below). Other forms of diabetic neuropathy may present as mononeuritis or autonomic neuropathy. Diabetic amyotrophy is muscle weakness due to neuropathy.
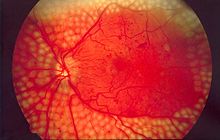
- Diabetic retinopathy, growth of friable and poor-quality new blood vessels in the retina as well as macular edema (swelling of the macula), which can lead to severe vision loss or blindness. Retinal damage (from microangiopathy) makes it the most common cause of blindness among non-elderly adults in the US.
Macrovascular disease leads to cardiovascular disease, to which accelerated atherosclerosis is a contributor:
- Coronary artery disease, leading to angina or myocardial infarction ("heart attack")
- Diabetic myonecrosis ('muscle wasting')
- Peripheral vascular disease, which contributes to intermittent claudication (exertion-related leg and foot pain) as well as diabetic foot.
- Stroke (mainly the ischemic type)
Diabetic foot, often due to a combination of sensory neuropathy (numbness or insensitivity) and vascular damage, increases rates of skin ulcers (diabetic foot ulcers) and infection and, in serious cases, necrosis and gangrene. It is why diabetics are prone to leg and foot infections and why it takes longer for them to heal from leg and foot wounds. It is the most common cause of non-traumatic adult amputation, usually of toes and or feet, in the developed world.
Carotid artery stenosis does not occur more often in diabetes, and there appears to be a lower prevalence of abdominal aortic aneurysm. However, diabetes does cause higher morbidity, mortality and operative risks with these conditions.[19]
Diabetic encephalopathy[20] is the increased cognitive decline and risk of dementia- including (but not limited to) the Alzheimer's type- observed in diabetes. Various mechanisms are proposed, including alterations to the vascular supply of the brain and the interaction of insulin with the brain itself.[21][22]
In the developed world, diabetes is the most significant cause of adult blindness in the non-elderly and the leading cause of non-traumatic amputation in adults, and diabetic nephropathy is the main illness requiring renal dialysis in the United States.[23]
References
- ^ Nathan DM, Cleary PA, Backlund JY, et al. (December 2005). "Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes". The New England Journal of Medicine 353 (25): 2643–53. doi:10.1056/NEJMoa052187. PMC 2637991. PMID 16371630. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2637991.
- ^ "The effect of intensive diabetes therapy on the development and progression of neuropathy. The Diabetes Control and Complications Trial Research Group". Annals of Internal Medicine 122 (8): 561–8. April 1995. doi:10.1059/0003-4819-122-8-199504150-00001 (inactive 2009-10-31). PMID 7887548. http://www.annals.org/cgi/pmidlookup?view=long&pmid=7887548.
- ^ Ahmed MS, Reid E and Khardori N (June 24, 2008). "Respiratory infections in diabetes: Reviewing the risks and challenges". Journal of Respiratory Diseases. http://www.consultantlive.com/diabetes/article/1145425/1403686.
- ^ M. Centofani, "Diabetes Complications: More than Sugar?" Science News, vol. 149, no. 26/27, Dec. 23–30, p. 421 (1995)
- ^ Rich SS (February 2006). "Genetics of diabetes and its complications". J. Am. Soc. Nephrol. 17 (2): 353–60. doi:10.1681/ASN.2005070770. PMID 16394110.
- ^ Pittenger GL, Liu D, Vinik AI (December 1993). "The toxic effects of serum from patients with type 1 diabetes mellitus on mouse neuroblastoma cells: a new mechanism for development of diabetic autonomic neuropathy". Diabet. Med. 10 (10): 925–32. doi:10.1111/j.1464-5491.1993.tb00008.x. PMID 8306588.
- ^ Kastelan S, Zjacić-Rotkvić V, Kastelan Z (2007). "Could diabetic retinopathy be an autoimmune disease?". Med. Hypotheses 68 (5): 1016–8. doi:10.1016/j.mehy.2006.05.073. PMID 17125935.
- ^ Granberg V, Ejskjaer N, Peakman M, Sundkvist G (August 2005). "Autoantibodies to autonomic nerves associated with cardiac and peripheral autonomic neuropathy". Diabetes Care 28 (8): 1959–64. doi:10.2337/diacare.28.8.1959. PMID 16043739.
- ^ Ichinose K, Kawasaki E, Eguchi K (2007). "Recent advancement of understanding pathogenesis of type 1 diabetes and potential relevance to diabetic nephropathy". Am. J. Nephrol. 27 (6): 554–64. doi:10.1159/000107758. PMID 17823503.
- ^ Adams DD (June 2008). "Autoimmune destruction of pericytes as the cause of diabetic retinopathy". Clin Ophthalmol 2 (2): 295–8. PMC 2693966. PMID 19668719. http://www.dovepress.com/articles.php?article_id=1783.
- ^ Monti MC, Lonsdale JT, Montomoli C, Montross R, Schlag E, Greenberg DA (December 2007). "Familial risk factors for microvascular complications and differential male-female risk in a large cohort of American families with type 1 diabetes". J. Clin. Endocrinol. Metab. 92 (12): 4650–5. doi:10.1210/jc.2007-1185. PMID 17878250.
- ^ Liew G, Klein R, Wong TY (2009). "The role of genetics in susceptibility to diabetic retinopathy". Int Ophthalmol Clin 49 (2): 35–52. doi:10.1097/IIO.0b013e31819fd5d7. PMC 2746819. PMID 19349785. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2746819.
- ^ Tarnow L, Groop PH, Hadjadj S, et al. (January 2008). "European rational approach for the genetics of diabetic complications—EURAGEDIC: patient populations and strategy". Nephrol. Dial. Transplant. 23 (1): 161–8. doi:10.1093/ndt/gfm501. PMID 17704113.
- ^ Foss CH, Vestbo E, Frøland A, Gjessing HJ, Mogensen CE, Damsgaard EM (March 2001). "Autonomic neuropathy in nondiabetic offspring of type 2 diabetic subjects is associated with urinary albumin excretion rate and 24-h ambulatory blood pressure: the Fredericia Study". Diabetes 50 (3): 630–6. doi:10.2337/diabetes.50.3.630. PMID 11246884.
- ^ Ban CR, Twigg SM (2008). "Fibrosis in diabetes complications: pathogenic mechanisms and circulating and urinary markers". Vasc Health Risk Manag 4 (3): 575–96. PMC 2515418. PMID 18827908. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2515418.
- ^ P. Zaoui, et al, "Role of Metalloproteases and Inhibitors in the Occurrence and Prognosis of Diabetic Renal Lesions," Diabetes and Metabolism, vol. 26 (Supplement 4), p. 25 (2000)
- ^ Taubes G (October 2008). "Diabetes. Paradoxical effects of tightly controlled blood sugar". Science 322 (5900): 365–7. doi:10.1126/science.322.5900.365. PMID 18927369.
- ^ Brinchmann-Hansen O, Dahl-Jørgensen K, Hanssen KF, Sandvik L (September 1988). "The response of diabetic retinopathy to 41 months of multiple insulin injections, insulin pumps, and conventional insulin therapy". Arch. Ophthalmol. 106 (9): 1242–6. PMID 3046587.
- ^ Weiss JS, Sumpio BE (February 2006). "Review of prevalence and outcome of vascular disease in patients with diabetes mellitus". European Journal of Vascular and Endovascular Surgery 31 (2): 143–50. doi:10.1016/j.ejvs.2005.08.015. PMID 16203161.
- ^ Aristides Veves, Rayaz A. Malik (2007). Diabetic Neuropathy: Clinical Management (Clinical Diabetes), Second Edition. New York: Humana Press. pp. 188–198. ISBN 1-58-829626-1.
- ^ Gispen WH, Biessels GJ (November 2000). "Cognition and synaptic plasticity in diabetes mellitus". Trends in Neurosciences 23 (11): 542–9. doi:10.1016/S0166-2236(00)01656-8. PMID 11074263.
- ^ http://www.cnn.com/2011/09/19/health/diabetes-doubles-alzheimers/index.html?hpt=he_c1
- ^ Mailloux, Lionel (2007-02-13). "UpToDate Dialysis in diabetic nephropathy". UpToDate. http://patients.uptodate.com/topic.asp?file=dialysis/15147. Retrieved 2007-12-07.
Diabetes (E10–E14, 250) Types of diabetes Blood tests Diabetes management Complications/prognosis Diabetic comas (Diabetic hypoglycemia, Diabetic ketoacidosis, Nonketotic hyperosmolar) · Diabetic angiopathy · Diabetic foot (ulcer, neuropathic arthropathy) · Diabetic myonecrosis · Diabetic nephropathy · Diabetic neuropathy · Diabetic retinopathy · Diabetic cardiomyopathy · Diabetic dermadrome (Diabetic dermopathy, Diabetic bulla, Diabetic cheiroarthropathy, Neuropathic ulcer)Lines of research Categories:- Diabetes
Wikimedia Foundation. 2010.