- Distraction osteogenesis
-
Distraction osteogenesis Intervention ICD-9-CM 78.3, 84.53 MeSH D019857 Distraction osteogenesis, also called callus distraction,[1] callotasis[1] and osteodistraction[2] is a surgical process used to reconstruct skeletal deformities and lengthen the long bones of the body. A corticotomy is used to fracture the bone into two segments, and the two bone ends of the bone are gradually moved apart during the distraction phase, allowing new bone to form in the gap.[1][3][4] When the desired or possible length is reached, a consolidation phase follows in which the bone is allowed to keep healing. Distraction osteogenesis has the benefit of simultaneously increasing bone length and the volume of surrounding soft tissues.
Although distraction technology has been used mainly in the field of orthopedics, early results in rats[5] and humans[6] indicated that the process can be applied to correct deformities of the jaw. These techniques are now utilised extensively by maxillofacial surgeons for the correction of micrognathia, midface, and fronto-orbital hypoplasia in patients with craniofacial deformities.
Contents
History
In 1905, Alessandro Codivilla introduced surgical practices for lengthening of the lower limbs.[7] Early techniques had a high number of complications, particularly during healing, and often resulted in a failure to achieve the goal of the surgery.[8][9]
In 1934 the New York Hospital For Joint Disease worked on an early method developed by Ilizarov. The major item that the US team of surgeons developed was the metal frame the leg was placed in to hold it perfectly in place till the cut made in the bone was healed over. [10]
The breakthrough came with a technique introduced by Russian orthopedic surgeon Gavril Ilizarov.[9] Ilizarov developed a procedure based on the biology of the bone and on the ability of the surrounding soft-tissues to regenerate under tension; the technique involved an external fixator, the Ilizarov apparatus, structured as a modular ring.[9] Although the types of complications remained the same (infection, the most common complication occurring particularly along the pin tracks, pain, nerve and soft tissue irritation[9]) the Ilizarov technique reduced the frequency and severity of the complications.[11] The Ilizarov technique made the surgery safer,[12] and allowed the goal of lengthening the limb to be achieved.
Difficulties arising during distraction osteogenesis
Difficulties that may arise during distraction osteogenesis are commonly classified in medical scientific literature according to the standard introduced by professor Dror Paley in a 1990 article.[11] Paley distinguished among problems (defined as "a difficulty that arises during the distraction or fixation period that is fully resolved by the end of the treatment period by non operative means"), obstacles, and complications.
Techniques
Using exclusively an external fixator
The most common is the Ilizarov surgery with the Ilizarov external fixator. Other external fixators are Wagner[13], Orthofix and Judet. Dr. Helong Bai (8th Hospital in Chongqing, China) developed the technique "Micro-wound" with a different apparatus.[14]
Ilizarov surgery
Main article: Ilizarov apparatus
Ilizarov surgery, developed by Gavriel Ilizarov, a Russian orthopedic surgeon, in 1951, is the oldest and most common method of distraction osteogenesis. It often brings complications[11], while some new methods have a much lower rate of complications.
The process involves the following:
- Shattered bones and devascularised ones are removed from the patient, leaving a gap;
- The healthy part of the upper bone is broken into two segments with an external saw;
- The leg is then fitted with the Ilizarov frame that pierces through the skin, muscles, and bone;
- Screws attached to the middle bone are turned 1 millimetre (mm) per day, so that new bone tissues that are formed in the growth zone are gradually pulled apart to increase the gap (One millimetre has been found to be the optimal bone distraction rate. Lengthening too fast overstretches the soft tissues, resulting not only in pain, but also in the inability of the bone to fill up the gap; too slow, and the bone hardens before the full lengthening process is complete.);
- After the gap is closed, the patient continues to wear the frame until the new bone solidifies; the waiting period is usually 120 days before the leg can be used.
Ilizarov surgery is extremely painful, uncomfortable, infection-prone, and often causes unsightly scars [citation needed]. Frames used to be made of stainless steel rings weighing up to 7 kilogram (kg), but newer models are made of Carbon fiber reinforced plastic, which though lighter, are equally cumbersome.
Derivative devices provide physicians better control over the bone axis and angle during elongation, such as the Taylor Spacial Frame (TSF) which is computer assisted. The downside of these developments are their relative complexity and resulting longer learning curve.
For decades, the Ilizarov procedure was the best chance for shattered bones to be restored, and crooked ones straightened. Breakthroughs in distraction osteogenesis in the 1990s, however, have resulted in less painful (albeit more expensive) alternatives, such as unilateral rails.
Using exclusively an intramedullary nail
The techniques that use an intramedullary nail without an external fixator are: Albizzia, Bliskunov, Guichet, Fitbone and ISKD.[15]
The Guichet Method
Invented in 1987 by Dr. Jean-Marc Guichet MD, the Albizzia nail was created during his residency at the University Center (CHU) of Dijon, France. The Albizzia nail is inserted into the bone canal after it is calibrated with a reamer. The nail is then fixed to the ends of the bone fragments with screws. The nail consists of two sliding tubes that rotate in relation to the other, allowing for the nail to extend through a series of “clicks.” After insertion, the patient “clicks” the nail by turning the knee and leg (femoral nail) or foot (tibial nail) alternating inward and outward rotations to gradually lengthen. 15 clicks per day results in 1mm of gain. Expansions of up to 10cm have been reported. The Albizzia nail is used in almost 30 countries and over 3,000 nails have been implanted.
In 2009, Dr. Guichet patented the Guichet Nail. The Guichet Nail is an improved version of the Albizzia nail because it uses stronger steel that allows for full weight bearing activity almost immediately after surgery. Furthermore, the Guichet Nail is customizable for size to ensure maximum comfort and efficiency for patients with smaller bones. Although there is initial pain after the surgery and during the clicks, the Guichet Nail is believed to be less painful than other methods as it is less invasive. Furthermore, as the patient controls the method of “clicking,” the patient is able to reduce pain by determining the most suitable method for themselves.
The Guichet Nail is currently used exclusively at the Leg Lengthening Clinic in Marseilles, France. Founded in 2011 by Guichet and Keeper, the clinic specializes in cosmetic leg lengthening surgeries. With worldwide recognition for being the foremost knowledgeable limb reconstruction surgeon with respect to internal fixators in the world, Dr. Guichet has successfully completed over 350 limb lengthening procedures.
Intramedullary skeletal kinetic distractor
In 2001, the "Intramedullary skeletal kinetic distractor" (ISKD) was introduced, allowing lengthening to take place internally, thereby drastically reducing the risk of infections and scarring. The ISKD device was designed by Dr. J. Dean Cole, MD of Orlando, Florida.
With ISKD, a telescopic rod that can be gradually extended by knee or ankle rotations is implanted into the bone. Lengthening is monitored by a hand-held external magnetic sensor that tracks the rotation of an internal magnet on a daily basis.
ISKD requires a physical leg movement to "click" the device into lengthening. In this method, there is no risk of accidentally over-stretching the bone due to the lengthener being preset to the desired fully extended length. However, there is a risk of growing the bone too quickly. Bone growth is monitored by measuring changes in the magnetic field of an embedded magnet in the system. The poles of the magnet change as the device grows. However, if the motion of the leg makes the device grow too quickly, and the magnet switches poles twice between measurements, then that growth is not recorded. This leads to overly rapid growth which can cause a number of issues such as nerve damage or causing breaks in the bone.
While there is some pain associated with the immediate post-op lengthening, the initial lengthening procedure is not to begin until one week after surgery. Furthermore, there is no noticeable "click" to the patient as there is less than nine degrees of rotation of the two bone segments in relation to one another.
Regularly used at a handful of medical centers mostly in the United States, only several dozens of ISKD devices are implanted each year. An improved version is currently being developed by its manufacturer (Orthofix).
Fitbone surgery
A form of surgery involving an intramedullar, fully implantable, electronically-motorised limb-lengthening implant[9], called "Fitbone", is a technologically advanced, though relatively complex, device.
Developed in Germany by Augustin Betz and Rainer Baumgart, the first successful operations were performed in 1996 and the technique was patented in 1997. Thus far, most of the surgeries using this method have been performed in Munich, Germany by Baumgart and Peter Thaller. The first successful surgeries in Asia have been performed since 2001 by Dr Sarbjit Singh in Tan Tock Seng Hospital, Singapore, and Dr Sittiporn, Bumrungrad Hospital, Bangkok. In December 2005 Fitbone surgery was done in Malaysia at the Mahkota Orthopaedic Reconstruction and Limb Lengthening Center, Melaka by Thirukumaran Subramaniam and Jeyaratnam T Satkunasingam. Dr. Bruce Foster of Adelaide, Australia, chairman of the "Bone Growth Foundation" — a charity established with the aim of helping children with crippling bone growth problems — is currently the only surgeon that uses the "Fitbone" device in the southern hemisphere.
Fitbone comprises a telescopic nail implant that can extend, powered by an electric motor and controlled by a receiver with an antenna that is buried under the skin; the receiver in turn is controlled by a hand-held radio-frequency transmitter. The procedure for lengthening the lower leg is as follows:
- A two-centimetre incision is made at the patient's knee, and a reamer is used to create enough space in the bone for a stainless steel nail.
- The bone is cut about 14 cm below the knee from the inside with an internal saw.
- The stainless steel nail is held in place by two screws. The top of the nail is attached to a tiny, plastic-encased receiver that is placed under the skin.
- The patient controls the lengthening process. By pushing a button on the transmitter when it is placed against the antenna, the built-in motor extends the nail one millimetre per day. When the leg has grown to the desired length, lengthening stops, and the bone is allowed to solidify.
- The device can be removed about two years after the initial surgery.
This procedure, however, comes at a price. While the Ilizarov external fixator costs approximately USD$4,000, and the ISKD implant about USD$8,000, the Fitbone device carries a price tag of roughly USD$15,000 (all prices exclusive of surgery costs).
The Bliskunov device is currently not available.
Future technology
Due to shortcomings of current external and internal devices and the evident market potential of cosmetic limb elongation, a growing number of companies are researching potential intramedullary technologies. These include:
- Concepts based on electromagnetic actuation
- Concepts based on smart material integration
- Concepts based on manual actuation
- Concepts based on electronic actuation
Biotechnological advances, such as in stem cell research, may become the next generation standard of care for limb elongation once it matures, possibly within a decade or two.[citation needed]
Post-surgical care
Following the initial surgery, patients must undergo a demanding physiotherapy regime comprising stretching exercises and at times, they may be required to be hooked up to a "continuous passive motion" device. The purpose is to avoid stiffness and to stimulate the muscles, nerves and blood vessels to grow alongside the bone. Patients are often prescribed painkillers and are unable to work while undergoing rehabilitation.[citation needed]
Aspects in limb lengthening
Maxillofacial Distraction Osteogenesis
Correcting the majority of congenital craniofacial defects, as well as some facial injuries resulting from trauma, requires making bones longer. Distraction osteogenesis is an effective way to grow new bone, but it is much more difficult to accomplish in the face than in other areas of the body. Bones must often be moved in three dimensions, as opposed to just one, as in a limb, and scarring must be kept to a minimum. Researchers[16] are attempting to improve the distraction devices used in the face. Until recently, the mechanisms were external and only operated along straight lines. Now, maxillofacial surgeons can use curvilinear devices capable of moving bone in three dimensions.
These new devices still need to be improved. They depend on patient caretakers reliably turning a screw. The next goal is to create devices that will move bone continuously, not in daily increments of 1 mm. These continuously moving devices would cause less pain, wouldn’t require daily patient compliance, and might promote faster bone growth. At the moment, researchers are testing a continuously moving device in animal models, and they have found that the device’s components are durable, that its user interface works, and that it is tolerated by the body. When the position sensor in the device is perfected, the device will be ready to use in people.
In distraction osteogenesis procedures involving the face, it is critical that bone movements be carefully planned before a device is implanted. No existing device is capable of changing its trajectory mid-course, and small skeletal changes lead to large changes in the structure of the face. Recently researchers have developed state-of-the-art software capable of simulating the entire process of distraction osteogenesis[17]. The 3-D planning tool uses data from CT scans to create a segmented model of the patient’s skull, and it then calculates the vector of movement required to achieve desirable bone positioning. Outcome CT scans can be overlaid on the original model to assess the effectiveness of the procedure. In the future, researchers hope that the distraction devices used in maxillofacial procedures will continue to improve, along with the corresponding software[18].
General solid bone regeneration
Distraction osteogenesis 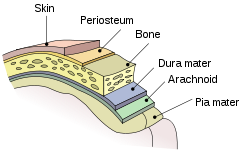
The periosteum appears just below the skin. 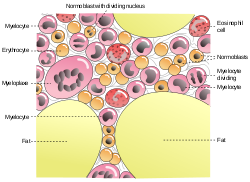
bone marrow The most important aspects for the success of bone distraction are an intact medullary blood supply, preservation of soft-tissue envelope, primarily the periosteum (which helps preserve the blood supply) and secondarly bone marrow and the stability of the fixator.[19][20][21][22][23]
Distraction rate
The distraction rate must be gradual, as a rapid rate of distraction will result in a fibrous union in which the bone pieces are joined by fibrous, rather than osseous tissue.[24][25]
Too slow of a distraction rate would result in early bone consolidation. A common distraction rate for lower limbs is 1 millimeter per day.[citation needed]
Complications
In a 2004 study[26] lengthening with an exclusively intramedullary nail (Albizzia) had a "significant lower rate" of complications respect to exclusively external methods (Judet, Orthofix, Ilizarov and Wagner fixators).
Possible uses of distraction osteogenesis
Although distraction osteogenesis is most often used in the treatment of post-traumatic injuries, it is increasingly used to correct limb discrepancies caused by congenital conditions and old injuries. A list of the possible uses of distraction osteogenesis are as follows:
- Congenital deformities (birth defects):
- Developmental deformities
- Neurofibromatosis (a rare condition which causes overgrowth in one leg); and
- Bow legs, resulting from rickets or secondary arthritis.
- Post-traumatic injuries
- Growth plates fractures;
- Malunion or non-union (when bones do not completely join, or join in a faulty position after a fracture);
- Shortening and deformity; and
- Bone defects.
- Infections and diseases
- Osteomyelitis (a bone infection, usually caused by bacteria);
- Septic arthritis (infections or bacterial arthritis); and
- Poliomyelitis (a viral disease which may result in the atrophy of muscles, causing permanent deformity).
- After tumors
- Short stature
- Achondroplasia (a form of dwarfism where arms and legs are very short, but torso is more normal in size); and
- Constitutional short stature.
Cosmetic lengthening of limbs
Generally, doctors tend to discourage[citation needed] cosmetic lengthening for people who want to add a couple of inches to their frames because such people are:
- breaking perfectly functional limbs;
- confining themselves unnecessarily to crutches or a wheelchair for over a year;
- voluntarily subjecting themselves to pain and discomfort;
- exposing themselves to unnecessary risk of infections, of damaged nerves and blood vessels, and fat embolism that can result in death; and
- incurring unnecessary expenses as the procedure is relatively expensive.[citation needed]
People insistent on doing the procedure, however, are required by some doctors[citation needed] to undergo a thorough body image assessment by a psychologist to help determine how far the person's quality of life has been affected by his perceived lack of height, and if doing the surgery will make a marked difference. The entire evaluation, which includes in-depth doctor-patient discussions, usually takes months during which time, the doctors hope that their patients will change their minds.[citation needed]
In popular culture
The protagonist of the movie Gattaca undergoes a limb lengthening procedure, along with other extreme methods, in order to impersonate another person and thus avoid genetic discrimination.
In Ian Fleming's James Bond novel Dr. No, Dr. No alludes to using leg-lengthing to increase his height to roughly 7 feet tall as part of a larger scheme to mask his identity.
See also
- Bone grafting
- Bone healing
- Fibrocartilage callus
- Nonunion
- Orthopedic surgery
- Tissue expansion
- Valgus deformity
Notes
- ^ a b c De Bastiani 1987
- ^ Tavakoli 1998
- ^ Paley 1997
- ^ Aquerreta 1994
- ^ Mehrara 1999
- ^ Chin, M.; Toth, B.A. (1996). "Distraction osteogenesis in maxillofacial surgery using internal devices: review of five cases.". J Oral Maxillofac Surg 54 (1): 45–53. doi:10.1016/S0278-2391(96)90303-1. PMID 8530999.
- ^ Codivilla, Alessandro (1905). "On the means of lengthening in the lower limbs, the muscles, and tissues which are shortened through deformity.". American Journal of Orthopedics Surgery" 2: 353.
- ^ Mosca, V.; Moseley, C.F. (1986). "Complications of Wagner leg lengthening and their avoidance". Orthop. Trans. 10: 462.
- ^ a b c d e Baumgart, Rainer; Augustin Betz, Leonhard Schweiberer (October 1997). "A Fully Implantable Motorized Intramedullary Nail for Limb Lengthening and Bone Transport". Clinical Orthopaedics & Related Research 343: 135–143. http://www.corronline.com/pt/re/corr/abstract.00003086-199710000-00023.htm;jsessionid=FSHQ4RjMvGXdZQK2fGxznvjsnR1hrypMmdXYZNZHT2Fqh2zxg2NR!-2083468996!-949856145!8091!-1. Retrieved 2006-12-27.
- ^ "Surgeon Stretches Crippled Legs", September 1934, Popular Science
- ^ a b c Paley, Dror (January 1990). "Problems, Obstacles, and Complications of Limb Lengthening by the Ilizarov Technique". Clinical Orthopaedics & Related Research 250: 81–104. http://www.corronline.com/pt/re/corr/abstract.00003086-199001000-00011.htm.
- ^ Paley, Dror (1988). "Current techniques of limb lengthening". Journal of Pediatric Orthopaedics 8 (1): 73–92. doi:10.1097/01241398-198801000-00018. PMID 3275690.
- ^ Zarzycki D, Tesiorowski M, Zarzycka M, Kacki W, Jasiewicz B (2002). "Long-term results of lower limb lengthening by the Wagner method". J Pediatr Orthop 22 (3): 371–4. doi:10.1097/00004694-200205000-00021. PMID 11961458. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0271-6798&volume=22&issue=3&spage=371.
- ^ "Short Persons Support: Health : Cosmetic Leg Lengthening : New Procedures". http://www.shortsupport.org/Health/Leg-Lengthening/new_devel.html.
- ^ "Orthoped — J. M. GUICHET". http://www.allongement-os-grandir.com/index-eng.php?page=nails#.
- ^ Led by Dr. Leonard B. Kaban of Massachusetts General Hospital
- ^ With financial support from CIMIT, Dr. Kaban’s team has spreaheaded this effort
- ^ Leonard B. Kaban, “Bone Lengthening by Distraction Osteogenesis,” CIMIT Forum, October 2, 2007
- ^ Guichet, Jean-Marc; Barbara Deromedis, Leo T. Donnan, Giovanni Peretti, Pierre Lascombes and Flavio Bado (1 May 2003). "Gradual Femoral Lengthening with the Albizzia Intramedullary Nail" (abstract). The Journal of Bone and Joint Surgery (American) 85-A (5): 838–848. PMID 12728034. http://www.ejbjs.org/cgi/content/abstract/85/5/838.
- ^ Delloye, C; Delefortrie G, Coutelier L, Vincent A. (January 1990). "Bone regenerate formation in cortical bone during distraction lengthening. An experimental study" (abstract). Clinical Orthopaedics & Related Research 250: 34–42. http://www.corronline.com/pt/re/corr/abstract.00003086-199001000-00005.htm.
- ^ Aldegheri, R (1993). "Callotasis". Journal of Pediatric Orthopaedics.
- ^ Guichet, Jean-Marc; Braillon P, Bodenreider O, Lascombes P (October 1998). "Periosteum and bone marrow in bone lengthening: a DEXA quantitative evaluation in rabbits". Acta Orthopaedica Scandinavica 69 (5): 527–31. doi:10.3109/17453679808997792. PMID 9855238.
- ^ Guichet, Jean-Marc (September 1999). Bone formation during limb lengthening. Animal experimentation with and without preservation of the bone marrow and/or periosteum. New York: New York University.
- ^ Warren SM, Mehrara BJ, Steinbrech DS, et al. (February 2001). "Rat mandibular distraction osteogenesis: part III. Gradual distraction versus acute lengthening". Plast. Reconstr. Surg. 107 (2): 441–53. doi:10.1097/00006534-200102000-00021. PMID 11214060. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0032-1052&volume=107&issue=2&spage=441.
- ^ fibrous union on biologyonline
- ^ de Billy B, Langlais J, Pouliquen JC, Guichet JM, Damsin JP. "Complications in lengthening of the femur using different methods". Http://proceedings.jbjs.org.uk/cgi/content/abstract/87-B/SUPP_I/70-c 87-B (Supp I): 70. http://proceedings.jbjs.org.uk/cgi/content/abstract/87-B/SUPP_I/70-c.
References
- Aquerreta, J. D. (1994). "Complications of bone lengthening". International orthopedics 18: 299–303. http://www.springerlink.com/index/K47P867K21600581.pdf.
- Chin, Martin; Bryant A Toth (January 1996). "Distraction osteogenesis in maxillofacial surgery using internal devices: Review of five cases". Journal of Oral and Maxillofacial Surgery 54 (1): 45–53. doi:10.1016/S0278-2391(96)90303-1. PMID 8530999. http://www.joms.org/article/PIIS0278239196903031/abstract.
- De Bastiani, G.; Aldegheri R, Renzi-Brivio L, Trivella G. (Mar-Apr 1987). "Limb lengthening by callus distraction (callotasis)". Journal of Pediatric Orthopaedics 7 (2): 129–34. doi:10.1097/01241398-198703000-00002. PMID 3558791.
- Mehrara, Babak J.; Rowe, Norman M.; Steinbrech, Douglas S.; Dudziak, Matthew E.; Saadeh, Pierre B.; McCarthy, Joseph G.; Gittes, George K.; Longaker, Michael T. (February 1999). "Rat Mandibular Distraction Osteogenesis: II. Molecular Analysis of Transforming Growth Factor Beta-1 and Osteocalcin Gene Expression". Plastic & Reconstructive Surgery 103 (2): 536–547. doi:10.1097/00006534-199902000-00026. http://www.plasreconsurg.com/pt/re/prs/abstract.00006534-199902000-00026.htm;jsessionid=FTyMbbxLfbsnPyYF89F81rtmj2p7KmRhP5KvDh2nfNqz25pvtmzB!-2083468996!-949856145!8091!-1.
- Paley, Dror; John E. Herzenberg, Guy Paremain, Anil Bhave (1997). "Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening". Journal of Bone & Joint Surgery (American Edition) 79 (10): 1464–80. PMID 9378732. http://www.ejbjs.org/cgi/content/abstract/79/10/1464.
- Tavakoli, K; Walsh WR, Bonar F, Smart R, Wulf S, Poole MD (August 1998). "The role of latency in mandibular osteodistraction". J Craniomaxillofac Surg 26 (4): 209–19. PMID 9777499.
Conference References
- Leonard B. Kaban, “Bone Lengthening by Distraction Osteogenesis,” CIMIT Forum, October 2, 2007
Further reading
- Simpson AH, Cole AS, Kenwright J (1999). "Leg lengthening over an intramedullary nail" (pdf). J Bone Joint Surg Br 81 (6): 1041–5. doi:10.1302/0301-620X.81B6.9359. PMID 10615983. http://www.jbjs.org.uk/cgi/reprint/81-B/6/1041.pdf.
External links
- Distraction Osteogenesis information from Seattle Children's Hospital Craniofacial Center
- Dr. Dror Paley LIMB LENGTHENING INTRODUCTION
- Limb Lengthening - ISKD Documents by Dr. Cole - includes additional information leg lengthening and case studies
- Dr. Guichet Leg Lengthening Clinic
- The Leg Lengthening Clinic's official forum and support group for those who have done or are considering Limb Lengthening
- Introduction to Distraction Osteogenesis by Dr. Martin Chin, D.D.S.
- Previous history of Prof. Betz’s Fitbone-Surgery
- Information on Fitbone procedure
- Cosmetic Leg Lengthening
- LL Community Support group for those who have done or are considering Limb Lengthening.
Categories:
Wikimedia Foundation. 2010.
