- Myocardial infarction diagnosis
-
A diagnosis of myocardial infarction is made by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers (blood tests for heart muscle cell damage).[1][2] A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.
A chest radiograph and routine blood tests may indicate complications or precipitating causes and are often performed upon arrival to an emergency department. New regional wall motion abnormalities on an echocardiogram are also suggestive of a myocardial infarction. Echo may be performed in equivocal cases by the on-call cardiologist.[3] In stable patients whose symptoms have resolved by the time of evaluation, Technetium (99mTc) sestamibi (i.e. a "MIBI scan") or thallium-201 chloride can be used in nuclear medicine to visualize areas of reduced blood flow in conjunction with physiologic or pharmocologic stress.[3][4] Thallium may also be used to determine viability of tissue, distinguishing whether non-functional myocardium is actually dead or merely in a state of hibernation or of being stunned.[5]
Contents
Diagnostic criteria
WHO criteria[6] formulated in 1979 have classically been used to diagnose MI; a patient is diagnosed with myocardial infarction if two (probable) or three (definite) of the following criteria are satisfied:
- Clinical history of ischaemic type chest pain lasting for more than 20 minutes
- Changes in serial ECG tracings
- Rise and fall of serum cardiac biomarkers such as creatine kinase-MB fraction and troponin
The WHO criteria were refined in 2000 to give more prominence to cardiac biomarkers.[7] According to the new guidelines, a cardiac troponin rise accompanied by either typical symptoms, pathological Q waves, ST elevation or depression or coronary intervention are diagnostic of MI.
Physical examination
The general appearance of patients may vary according to the experienced symptoms; the patient may be comfortable, or restless and in severe distress with an increased respiratory rate. A cool and pale skin is common and points to vasoconstriction. Some patients have low-grade fever (38–39 °C). Blood pressure may be elevated or decreased, and the pulse can become irregular.[8][9]
If heart failure ensues, elevated jugular venous pressure and hepatojugular reflux, or swelling of the legs due to peripheral edema may be found on inspection. Rarely, a cardiac bulge with a pace different from the pulse rhythm can be felt on precordial examination. Various abnormalities can be found on auscultation, such as a third and fourth heart sound, systolic murmurs, paradoxical splitting of the second heart sound, a pericardial friction rub and rales over the lung.[8][10]
Electrocardiogram
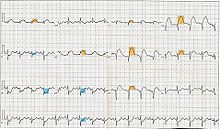 12-lead electrocardiogram showing ST-segment elevation (orange) in I, aVL and V1-V5 with reciprocal changes (blue) in the inferior leads, indicative of an anterior wall myocardial infarction.
12-lead electrocardiogram showing ST-segment elevation (orange) in I, aVL and V1-V5 with reciprocal changes (blue) in the inferior leads, indicative of an anterior wall myocardial infarction.
The primary purpose of the electrocardiogram is to detect ischemia or acute coronary injury in broad, symptomatic emergency department populations. A serial ECG may be used to follow rapid changes in time. The standard 12 lead ECG does not directly examine the right ventricle, and is relatively poor at examining the posterior basal and lateral walls of the left ventricle. In particular, acute myocardial infarction in the distribution of the circumflex artery is likely to produce a nondiagnostic ECG.[11] The use of additional ECG leads like right-sided leads V3R and V4R and posterior leads V7, V8, and V9 may improve sensitivity for right ventricular and posterior myocardial infarction.
The 12 lead ECG is used to classify patients into one of three groups:[12]
- those with ST segment elevation or new bundle branch block (suspicious for acute injury and a possible candidate for acute reperfusion therapy with thrombolytics or primary PCI),
- those with ST segment depression or T wave inversion (suspicious for ischemia), and
- those with a so-called non-diagnostic or normal ECG.
A normal ECG does not rule out acute myocardial infarction. Mistakes in interpretation are relatively common, and the failure to identify high risk features has a negative effect on the quality of patient care.[13]
Cardiac markers
Cardiac markers or cardiac enzymes are proteins that leak out of injured myocardial cells through their damaged cell membranes into the bloodstream. Until the 1980s, the enzymes SGOT and LDH were used to assess cardiac injury. Now, the markers most widely used in detection of MI are MB subtype of the enzyme creatine kinase and cardiac troponins T and I as they are more specific for myocardial injury. The cardiac troponins T and I which are released within 4–6 hours of an attack of MI and remain elevated for up to 2 weeks, have nearly complete tissue specificity and are now the preferred markers for asssessing myocardial damage.[14] Heart-type fatty acid binding protein is another marker, used in some home test kits. Elevated troponins in the setting of chest pain may accurately predict a high likelihood of a myocardial infarction in the near future.[15] New markers such as glycogen phosphorylase isoenzyme BB are under investigation.[16]
The diagnosis of myocardial infarction requires two out of three components (history, ECG, and enzymes). When damage to the heart occurs, levels of cardiac markers rise over time, which is why blood tests for them are taken over a 24-hour period. Because these enzyme levels are not elevated immediately following a heart attack, patients presenting with chest pain are generally treated with the assumption that a myocardial infarction has occurred and then evaluated for a more precise diagnosis.[17]
Angiography
In difficult cases or in situations where intervention to restore blood flow is appropriate, coronary angiography can be performed. A catheter is inserted into an artery (usually the femoral artery) and pushed to the vessels supplying the heart. A radio-opaque dye is administered through the catheter and a sequence of x-rays (fluoroscopy) is performed. Obstructed or narrowed arteries can be identified, and angioplasty applied as a therapeutic measure (see below). Angioplasty requires extensive skill, especially in emergency settings. It is performed by a physician trained in interventional cardiology.
Histopathology
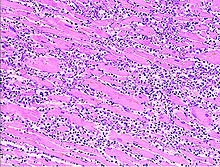 Microscopy image (magn. ca 100x, H&E stain) from autopsy specimen of myocardial infarct (7 days post-infarction).
Microscopy image (magn. ca 100x, H&E stain) from autopsy specimen of myocardial infarct (7 days post-infarction).
Histopathological examination of the heart may reveal infarction at autopsy. Under the microscope, myocardial infarction presents as a circumscribed area of ischemic, coagulative necrosis (cell death). On gross examination, the infarct is not identifiable within the first 12 hours.[18]
 Micrograph of a myocardial infarction (ca. 400x H&E stain ) with prominent contraction band necrosis.
Micrograph of a myocardial infarction (ca. 400x H&E stain ) with prominent contraction band necrosis.
Although earlier changes can be discerned using electron microscopy, one of the earliest changes under a normal microscope are so-called wavy fibers.[19] Subsequently, the myocyte cytoplasm becomes more eosinophilic (pink) and the cells lose their transversal striations, with typical changes and eventually loss of the cell nucleus.[20] The interstitium at the margin of the infarcted area is initially infiltrated with neutrophils, then with lymphocytes and macrophages, who phagocytose ("eat") the myocyte debris. The necrotic area is surrounded and progressively invaded by granulation tissue, which will replace the infarct with a fibrous (collagenous) scar (which are typical steps in wound healing). The interstitial space (the space between cells outside of blood vessels) may be infiltrated with red blood cells.[18]
These features can be recognized in cases where the perfusion was not restored; reperfused infarcts can have other hallmarks, such as contraction band necrosis.[21]
See also
References
- ^ Mallinson, T (2010). "Myocardial Infarction". Focus on First Aid (15): 15. http://www.focusonfirstaid.co.uk/Magazine/issue15/index.aspx. Retrieved 2010-06-08.
- ^ Myocardial infarction: diagnosis and investigations - GPnotebook, retrieved November 27, 2006.
- ^ a b DE Fenton et al. Myocardial infarction - eMedicine, retrieved November 27, 2006.
- ^ HEART SCAN - Patient information from University College London. Retrieved November 27, 2006.
- ^ Skoufis E, McGhie AI (1998). "Radionuclide techniques for the assessment of myocardial viability". Tex Heart Inst J 25 (4): 272–9. PMC 325572. PMID 9885104. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=325572.
- ^ Anonymous (March 1979). "Nomenclature and criteria for diagnosis of ischemic heart disease. Report of the Joint International Society and Federation of Cardiology/World Health Organization task force on standardization of clinical nomenclature". Circulation 59 (3): 607–9. PMID 761341.
- ^ Alpert JS, Thygesen K, Antman E, Bassand JP. (2000). "Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction". J Am Coll Cardiol 36 (3): 959–69. doi:10.1016/S0735-1097(00)00804-4. PMID 10987628.
- ^ a b S. Garas et al.. Myocardial Infarction. eMedicine. Retrieved November 22, 2006.
- ^ Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. Harrison's Principles of Internal Medicine. p. 1444. New York: McGraw-Hill, 2005. ISBN 0-07-139140-1.
- ^ Kasper DL, et al. Harrison's Principles of Internal Medicine. p. 1450.
- ^ Cannon CP at al. Management of Acute Coronary Syndromes. p. 175. New Jersey: Humana Press, 1999. ISBN 0-89603-552-2.
- ^ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care — Part 8: Stabilization of the Patient With Acute Coronary Syndromes". Circulation 112: IV–89–IV–110. 2005. doi:10.1161/CIRCULATIONAHA.105.166561. http://circ.ahajournals.org/cgi/content/full/112/24_suppl/IV-89.
- ^ Masoudi FA, Magid DJ, Vinson DR, et al. (October 2006). "Implications of the failure to identify high-risk electrocardiogram findings for the quality of care of patients with acute myocardial infarction: results of the Emergency Department Quality in Myocardial Infarction (EDQMI) study". Circulation 114 (15): 1565–71. doi:10.1161/CIRCULATIONAHA.106.623652. PMID 17015790. http://circ.ahajournals.org/cgi/content/full/114/15/1565.
- ^ Eisenman A (2006). "Troponin assays for the diagnosis of myocardial infarction and acute coronary syndrome: where do we stand?". Expert Rev Cardiovasc Ther 4 (4): 509–14. doi:10.1586/14779072.4.4.509. PMID 16918269.
- ^ Aviles RJ, Askari AT, Lindahl B, Wallentin L, Jia G, Ohman EM, Mahaffey KW, Newby LK, Califf RM, Simoons ML, Topol EJ, Berger P, Lauer MS (2002). "Troponin T levels in patients with acute coronary syndromes, with or without renal dysfunction". N Engl J Med 346 (26): 2047–52. doi:10.1056/NEJMoa013456. PMID 12087140.. Summary for laymen
- ^ Apple FS, Wu AH, Mair J, et al. (2005). "Future biomarkers for detection of ischemia and risk stratification in acute coronary syndrome". Clin. Chem. 51 (5): 810–24. doi:10.1373/clinchem.2004.046292. PMID 15774573. http://www.clinchem.org/cgi/content/full/51/5/810.
- ^ Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, Jones RH, Kereiakes D, Kupersmith J, Levin TN, Pepine CJ, Schaeffer JW, Smith EE III, Steward DE, Théroux P. (2002). "ACC/AHA 2002 guideline update for the management of patients with unstable angina and non–ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina)" (PDF). J Am Coll Cardiol 40 (7): 1366–74. PMID 12383588. http://www.acc.org/qualityandscience/clinical/guidelines/unstable/incorporated/UA_incorporated.pdf.
- ^ a b Rubin's Pathology — Clinicopathological Foundations of Medicine. Maryland: Lippincott Williams & Wilkins. 2001. pp. 546. ISBN 0-7817-4733-3.
- ^ Eichbaum FW. "'Wavy' myocardial fibers in spontaneous and experimental adrenergic cardiopathies" Cardiology 1975; 60(6): 358–65. PMID 782705
- ^ S Roy. Myocardial infarction. Retrieved November 28, 2006.
- ^ Fishbein, M. C. (1990). "Reperfusion injury". Clinical Cardiology 13 (3): 213–217. doi:10.1002/clc.4960130312. PMID 2182247.
Categories:- Aging-associated diseases
- Cardiovascular diseases
- Ischemic heart diseases
- Medical emergencies
- Cardiac procedures
Wikimedia Foundation. 2010.

