- Percutaneous coronary intervention
-
Percutaneous coronary intervention Intervention 
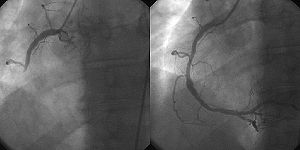
A coronary angiogram (an X-ray with radio-opaque contrast in the coronary arteries) that shows the left coronary circulation. The distal left main coronary artery (LMCA) is in the left upper quadrant of the image. Its main branches (also visible) are the left circumflex artery (LCX), which courses top-to-bottom initially and then toward the centre/bottom, and the left anterior descending (LAD) artery, which courses from left-to-right on the image and then courses down the middle of the image to project underneath of the distal LCX. The LAD, as is usual, has two large diagonal branches, which arise at the centre-top of the image and course toward the centre/right of the image.ICD-9-CM 36.09, 00.66 Percutaneous coronary intervention (PCI), commonly known as coronary angioplasty or simply angioplasty, is one therapeutic procedure used to treat the stenotic (narrowed) coronary arteries of the heart found in coronary heart disease. These stenotic segments are due to the build up of cholesterol-laden plaques that form due to atherosclerosis. PCI is usually performed by an interventional cardiologist.
Coronary artery bypass grafting (CABG), which bypasses stenotic arteries by grafting vessels from elsewhere in the body, is an alternative treatment. Most studies have found that CABG is better than PCI for reducing death and myocardial infarction. However, PCI does improve quality of life. PCI has proven to be as effective and less costly than CABG in patients with medically refractory myocardial ischemia.[1]
Contents
History
Main article: History of invasive and interventional cardiologyCoronary angioplasty, also known as percutaneous transluminal coronary angioplasty (PTCA), because it's done through the skin and through the lumen of the artery, was first developed in 1977 by Andreas Gruentzig. The first procedure took place Friday Sept 16, 1977 at Zurich, Switzerland[2]. Adoption of the procedure accelerated subsequent to Gruentzig's move to Emory University in the United States. Gruentzig's first fellow at Emory was Merril Knudtson, who, by 1981, had already introduced it to Calgary, Alberta, Canada[3]. By the mid-1980s, many leading medical centers throughout the world were adopting the procedure as a treatment for coronary artery disease (CAD).
Angioplasty is sometimes erroneously referred to as Dottering, after Interventional Radiologist, Dr Charles Theodore Dotter, who, together with Dr Melvin P. Judkins, first described angioplasty in 1964.[4] As the range of procedures performed upon coronary artery lumens has widened, the name of the procedure has changed to percutaneous coronary intervention (PCI).
Indications
Percutaneous coronary intervention can be performed to reduce or eliminate the symptoms of coronary artery disease, including angina (chest pain), dyspnea (shortness of breath) on exertion, and congestive heart failure. PCI is also used to abort an acute myocardial infarction, and in some specific cases it may reduce death.[citation needed]
Angioplasty is less invasive than coronary artery bypass surgery (CABG). However, CABG has better results in terms of death, myocardial infarction, and the need to repeat the procedure. This was demonstrated in repeated studies.
A 2002 randomized controlled trial found that bare metal stents had no benefit over CABG.[5]
A 2008 randomized controlled trial found that drug-coated stents did not reduce death in non-acute cases. The COURAGE trial concluded that treating with PCI for stable coronary artery disease did not reduce the risk of death, myocardial infarction, or other major cardiovascular events when added to standard medical treatment.[6]
A 2008 retrospective study found a lower death rate for CABG.[7]
PCI did have a small effect on improving quality of life.[8]
Controversy
The value of angioplasty in rescuing someone having a heart attack (by immediately alleviating an obstruction) is clearly defined in multiple studies, but studies have failed to find reduction in hard endpoints for angioplasty vs. medical therapy in stable angina patients. The artery-opening procedure can temporarily alleviate chest pain, but does not contribute to longevity. The "vast majority of heart attacks do not originate with obstructions that narrow arteries".[9]
Procedures
The term balloon angioplasty is commonly used to describe percutaneous coronary intervention, which describes the inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery. While balloon angioplasty is still done as a part of nearly all percutaneous coronary interventions, it is rarely the only procedure performed.
Other procedures that are done during a percutaneous coronary intervention include:
- Implantation of stents
- Rotational or laser atherectomy
- Brachytherapy (Use of radioactive source to inhibit restenosis.)
Sometimes a small mesh tube, or "stent", is introduced into the blood vessel or artery to prop it open using percutaneous methods. Angioplasty with stenting is a viable alternative to heart surgery for some forms of non-severe coronary artery disease.[10] It has consistently been shown to reduce symptoms due to coronary artery disease and to reduce cardiac ischemia, but has not been shown in large trials to reduce mortality due to coronary artery disease, except in patients being treated for a heart attack acutely (also called primary angioplasty). In acute cases, there is a small but definite reduction of mortality with this form of treatment compared with medical therapy, which usually consists of the administration of thrombolytic ("clot busting") medication.[11][12]
Technique
The angioplasty procedure usually consists of most of the following steps and is performed by physicians, physician assistants, nurse practitioners, nurses, radiological technologists and cardiac invasive specialist; all of whom have extensive and specialized training in these types of procedures.
- Access into the femoral artery in the leg (or, less commonly, into the radial artery or brachial artery in the arm) is created by a device called an "introducer needle". This procedure is often termed percutaneous access.
- Once access into the artery is gained, a "sheath introducer" is placed in the opening to keep the artery open and control bleeding.
- Through this sheath, a long, flexible, soft plastic tube called a "guiding catheter" is pushed. The tip of the guiding catheter is placed at the mouth of the coronary artery. The guiding catheter also allows for radiopaque dyes (usually iodine based) to be injected into the coronary artery, so that the disease state and location can be readily assessed using real time x-ray visualization.
- During the x-ray visualization, the cardiologist estimates the size of the coronary artery and selects the type of balloon catheter and coronary guidewire that will be used during the case. Heparin (a "blood thinner" or medicine used to prevent the formation of clots) is given to maintain blood flow.
- The coronary guidewire, which is an extremely thin wire with a radio-opaque flexible tip, is inserted through the guiding catheter and into the coronary artery. While visualizing again by real-time x-ray imaging, the cardiologist guides the wire through the coronary artery to the site of the stenosis or blockage. The tip of the wire is then passed across the blockage. The cardiologist controls the movement and direction of the guide wire by gently manipulating the end that sits outside the patient through twisting of the guidewire.
- While the guidewire is in place, it now acts as the pathway to the stenosis. The tip of the angioplasty or balloon catheter is hollow and is then inserted at the back of the guidewire—thus the guidewire is now inside of the angioplasty catheter. The angioplasty catheter is gently pushed forward, until the deflated balloon is inside of the blockage.
- The balloon is then inflated, and it compresses the atheromatous plaque and stretches the artery wall to expand.
- If an expandable wire mesh tube (stent) was on the balloon, then the stent will be implanted (left behind) to support the new stretched open position of the artery from the inside.[13]
Coronary stenting
Traditional ("bare metal") coronary stents provide a mechanical framework that holds the artery wall open, preventing stenosis, or narrowing, of coronary arteries. PTCA with stenting has been shown to be superior to angioplasty alone in patient outcome by keeping arteries patent for a longer period of time.[14]
Newer drug-eluting stents (DES) are traditional stents that are coated with drugs, which, when placed in the artery, release certain drugs over time. It has been shown that these types of stents help prevent restenosis of the artery through several different physiological mechanisms, which rely upon the suppression of tissue growth at the stent site and local modulation of the body's inflammatory and immune responses. Five drugs, Biolimus A9[15], Zotarolimus, sirolimus, everolimus and paclitaxel, have demonstrated safety and efficacy in this application in controlled clinical trials by stent device manufacturers.[citation needed] However, in 2006 three broad European trials seem to indicate that drug-eluting stents may be susceptible to an event known as "late stent thrombosis", where the blood-clotting inside the stent can occur one or more years post-stent. Late stent thrombosis occurs in 0.9% of patients, and is extremely dangerous and is fatal in about one-third of cases when the thrombosis occurs.[16][17] New generation DES products, such as the BioMatrix stent marketed by Biosensors International since January 2008 in Europe, seek to eliminate this risk by using a biodegradable coating.
Risks
Coronary angioplasty is widely practised and has a number of risks;[18] however, major procedural complications are uncommon. Coronary angioplasty is usually performed by an interventional cardiologist, a medical doctor with special training in the treatment of the heart using invasive catheter-based procedures.[citation needed]
The patient is usually awake during angioplasty, and chest discomfort may be experienced during the procedure; the reporting of symptoms indicates the procedure is causing ischemia and the cardiologist may alter or abort part of the procedure. Bleeding from the insertion point in the groin is common, in part due to the use of anti-platelet clotting drugs. Some bruising is therefore to be expected, but occasionally a hematoma may form. This may delay hospital discharge as flow from the artery into the hematoma may continue (pseudoaneurysm) which requires surgical repair. Infection at the skin puncture site is rare and dissection (tearing) of the access blood vessel is uncommon. Allergic reaction to the contrast dye used is possible, but has been reduced with the newer agents. Deterioration of kidney function can occur in patients with pre-existing kidney disease, but kidney failure requiring dialysis is rare. Vascular access complications are less common and less serious when the procedure is performed via the radial artery.[citation needed]
The most serious risks are death, stroke, VF (non-sustained VT is common), myocardial infarction (heart attack) and aortic dissection. A heart attack during or shortly after the procedure occurs in 0.3% of cases; this may require emergency coronary artery bypass surgery.[19] Heart muscle injury characterized by elevated levels of CK-MB, troponin I, and troponin T may occur in up to 30% of all PCI procedures. Elevated enzymes have been associated with later clinical outcomes such as higher risk of death, subsequent MI and need for repeat revascularization procedures[20][21]. Angioplasty carried out shortly after a myocardial infarction has a risk of causing a stroke of 1 in 1000, which is less than the 1 in 100 risk encountered by those receiving thrombolytic drug therapy.[citation needed]
As with any procedure involving the heart, complications can sometimes, though rarely, cause death. Less than 2 percent of people die during angioplasty. Sometimes chest pain can occur during angioplasty because the balloon briefly blocks off the blood supply to the heart. The risk of complications is higher in:[22]
- People aged 75 and older
- People who have kidney disease or diabetes
- Women
- People who have poor pumping function in their hearts
- People who have extensive heart disease and blockages
See also
- Angioplasty
- Cardiac catheterization
- Coronary artery bypass surgery
- Cutting balloon
- Fractional flow reserve
References
- ^ Stroupe KT, Morrison DA, Hlatky MA, Barnett PG, Cao L, Lyttle C, Hynes DM, Henderson WG (September 2006). "Cost-effectiveness of coronary artery bypass grafts versus percutaneous coronary intervention for revascularization of high-risk patients". Circulation 114 (12): 1251–1257. PMID 16966588.
- ^ Meier B, Bachmann D, Lüscher T (February 2003). "25 years of coronary angioplasty: almost a fairy tale". Lancet 361 (9356): 527. doi:10.1016/S0140-6736(03)12470-1. PMID 12583964.
- ^ "Foothills Interventional Cardiology Service". http://www.libin.ucalgary.ca/services/foothills.php. Retrieved 2008-12-31.
- ^ Dotter CT, Judkins MP (November 1964). "Transluminal treatment of arteriosclerotic obstruction". Circulation 30 (5): 654–70. PMID 14226164. http://circ.ahajournals.org/cgi/reprint/30/5/654. Retrieved 2009-07-13.
- ^ SoS Investigators (2002). "Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): a randomised controlled trial". Lancet 360 (9338): 965–70. doi:10.1016/S0140-6736(02)11078-6. PMID 12383664.
- ^ Boden, W. E., R. A. O'Rourke, et al. (2007). ["Optimal medical therapy with or without PCI for stable coronary disease." http://content.nejm.org/cgi/content/abstract/356/15/1503] N Engl J Med 356(15): 1503-16.
- ^ Hannan EL, Wu C, Walford G, et al. (2008). "Drug-eluting stents vs. coronary-artery bypass grafting in multivessel coronary disease". N. Engl. J. Med. 358 (4): 331–41. doi:10.1056/NEJMoa071804. PMID 18216353.
- ^ Weintraub WS, Spertus JA, Kolm P, et al. (August 2008). "Effect of PCI on quality of life in patients with stable coronary disease". The New England Journal of Medicine 359 (7): 677–87. doi:10.1056/NEJMoa072771. PMID 18703470. Lay summary – NPR (2008-09-04).
- ^ Kolata, Gina. "New Heart Studies Question the Value Of Opening Arteries" The New York Times, March 21, 2004. Retrieved January 29, 2011.
- ^ Michaels AD, Chatterjee K (December 2002). "Cardiology patient pages. Angioplasty versus bypass surgery for coronary artery disease". Circulation 106 (23): e187–90. doi:10.1161/01.CIR.0000044747.37349.64. PMID 12460885. http://circ.ahajournals.org/cgi/content/full/106/23/e187. Retrieved 2009-07-13.
- ^ Mercado, N, Flather, MD, Boersna, E, et al., on Behalf of the Trial Investigators CABG vs Stenting for Multivessel Disease: a Meta-analysis of ARTS-1, SoS, ERACI-2, and MASS-2, Presentation at European Society of Cardiology Congress 2003
- ^ Weaver WD, Simes RJ, Betriu A, et al. (December 1997). "Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review". JAMA 278 (23): 2093–8. doi:10.1001/jama.278.23.2093. PMID 9403425.
- ^ PTCA or Balloon Angioplasty
- ^ Gandhi MM, Dawkins KD (March 1999). "Fortnightly review: Intracoronary stents". BMJ (Clinical Research Ed.) 318 (7184): 650–3. PMC 1115094. PMID 10066211. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1115094. Retrieved 2009-07-13.
- ^ Windecker, Stephan; Serruys, Patrick W; Wandel, Simon; Buszman, Pawel; Trznadel, Stanislaw; Linke, Axel; Lenk, Karsten; Ischinger, Thomas et al. (2008). "Biolimus-eluting stent with biodegradable polymer versus sirolimus-eluting stent with durable polymer for coronary revascularisation (LEADERS): a randomised non-inferiority trial". The Lancet 372 (9644): 1163–1173. doi:10.1016/S0140-6736(08)61244-1. http://www.lancet.com/journals/lancet/article/PIIS0140-6736%2808%2961244-1/fulltext.
- ^ Mauri L, Hsieh WH, Massaro JM, Ho KK, D'Agostino R, Cutlip DE (March 2007). "Stent thrombosis in randomized clinical trials of drug-eluting stents". The New England Journal of Medicine 356 (10): 1020–9. doi:10.1056/NEJMoa067731. PMID 17296821.
- ^ European Society of Cardiology Science News, 2007 Thrombosis is the price for the success of drug-eluting stents
- ^ UK's NHS endorsed 'Best Treatments' advice on 'clinical evidence for patients from the BMJ' on Coronary angioplasty and its risks
- ^ Yang EH, Gumina RJ, Lennon RJ, Holmes DR, Rihal CS, Singh (2005). "to 2003". Journal of the American College of Cardiology 46 (11): 2004–2009. doi:10.1016/j.jacc.2005.06.083. PMID 16325032.
- ^ Califf R. M., Abdelmeguid A. E. et al. (1998). "Myonecrosis after revascularization procedures". J Am Coll Cardiol 31 (2): 241–51. doi:10.1016/S0735-1097(97)00506-8. PMID 9462562.
- ^ Tardiff B. E., Califf R. M. et al. (1999). "Clinical outcomes after detection of elevated cardiac enzymes in patients undergoing percutaneous intervention. IMPACT-II Investigators. Integrilin (eptifibatide) to Minimize Platelet Aggregation and Coronary Thrombosis-II.". J Am Coll Cardiol 33 (1): 88–96. doi:10.1016/S0735-1097(98)00551-8. PMID 9935014.
- ^ http://www.nhlbi.nih.gov/health/dci/Diseases/Angioplasty/Angioplasty_Risks.html
External links
- Angioplasty.Org news and education
- European Association of Percutaneous Cardiovascular Interventions (EAPCI)
- Q&A: Primary angioplasty, 18 Oct 2008
Categories:- Cardiac procedures
Wikimedia Foundation. 2010.