- Erlotinib
-
Erlotinib 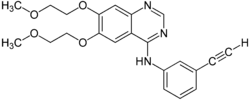
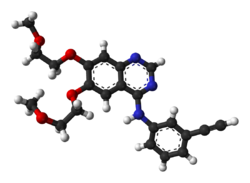
Systematic (IUPAC) name N-(3-ethynylphenyl)-6,7-bis(2-methoxyethoxy)
quinazolin-4-amineClinical data Trade names Tarceva AHFS/Drugs.com monograph MedlinePlus a605008 Licence data EMA:Link, US FDA:link Pregnancy cat. D(US) Legal status POM (UK) ℞-only (US) Routes Oral Identifiers CAS number 183321-74-6 
ATC code L01XE03 PubChem CID 176870 DrugBank APRD00951 ChemSpider 154044 
UNII J4T82NDH7E 
KEGG D07907 
ChEBI CHEBI:114785 
ChEMBL CHEMBL553 
Chemical data Formula C22H23N3O4 Mol. mass 393.436 g/mol SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Erlotinib hydrochloride (trade name Tarceva) is a drug used to treat non-small cell lung cancer, pancreatic cancer and several other types of cancer. It is a reversible tyrosine kinase inhibitor, which acts on the epidermal growth factor receptor (EGFR). It is marketed in the United States by Genentech and OSI Pharmaceuticals and elsewhere by Roche. In lung cancer, it extends life by an average of 3.3 months at a cost of CDN$95,000.
Contents
Mechanism
Erlotinib is an EGFR inhibitor. The drug follows Iressa gefitinib, which was the first drug of this type. Erlotinib specifically targets the epidermal growth factor receptor (EGFR) tyrosine kinase, which is highly expressed and occasionally mutated in various forms of cancer. It binds in a reversible fashion to the adenosine triphosphate (ATP) binding site of the receptor.[1] For the signal to be transmitted, two members of the EGFR family need to come together to form a homodimer. These then use the molecule of ATP to autophosphorylate each other, which causes a conformational change in their intracellular structure, exposing a further binding site for binding proteins that cause a signal cascade to the nucleus. By inhibiting the ATP, autophosphorylation is not possible and the signal is stopped.
Clinical applications
Erlotinib has shown a survival benefit in the treatment of lung cancer in phase III trials. The SATURN (Sequential Tarceva in Unresectable NSCLC) study found that erlotinib added to chemotherapy improved overall survival by 19%, and improved progression-free survival (PFS) by 29%, when compared to chemotherapy alone.[2][3] The manufacturer estimated that erlotinib can extend life by approximately 3.3 months.[4] This is at a cost of CDN$95,000, which some researchers call "marginally" cost effective, and led NICE to refuse to recommend it.[5]
The U.S. Food and Drug Administration (FDA) has approved for the treatment of locally advanced or metastatic non-small cell lung cancer that has failed at least one prior chemotherapy regimen.
In November 2005, the FDA approved erlotinib in combination with gemcitabine for treatment of locally advanced, unresectable, or metastatic pancreatic cancer.[6]
In lung cancer, erlotinib has been shown to be effective in patients with or without EGFR mutations, but appears to be more effective in the group of patients with EGFR mutations. A test for the EGFR mutation in cancer patients has been developed by Genzyme. The response rate among EGFR mutation positive patients is approximately 60%. Patients who are non-smokers, and light former smokers, with adenocarcinoma or subtypes like BAC are more likely to have EGFR mutations, but mutations can occur in all types of patients.
EGFR positive patients are generally KRAS negative.[citation needed]
Erlotinib has recently been shown to be a potent inhibitor of JAK2V617F activity. JAK2V617F is a mutant of tyrosine kinase JAK2, is found in most patients with polycythemia vera (PV) and a substantial proportion of patients with idiopathic myelofibrosis or essential thrombocythemia. The study suggests that erlotinib may be used for treatment of JAK2V617F-positive PV and other myeloproliferative disorders.[7]
The drug's US patent will expire in 2020.[8] In India, generic pharmaceutical firm Cipla is battling with Roche against the Indian patent for this drug. In April 2009, the Delhi High Court granted a final approval to Cipla to manufacture and sell its generic version of Erlotinib in India.[9] Meanwhile, another generic pharmaceutical firm - Natco is also seeking to manufacture the generic version of Erlotinib in India but sell it to patients in Nepal using the TRIPS Agreements' Doha Declaration.[10][11]
Administration
Oral tablets
Side effects
Common side effects
- Rash occurs in the majority of patients. This resembles acne and primarily involves the face and neck. It is self-limited and resolves in the majority of cases, even with continued use. Interestingly, some clinical studies have indicated a correlation between the severity of the skin reactions and increased survival though this has not been quantitatively assessed.[12] The Journal of Clinical Oncology reported in 2004 that "cutaneous [skin] rash seems to be a surrogate marker of clinical benefit, but this finding should be confirmed in ongoing and future studies."[13] The newsletter Lung Cancer Frontiers reported in its October 2003 issue, "Patients with moderate to severe cutaneous reactions [rashes] have a far better survival, than those with only mild reactions and much better than those with no cutaneous manifestations of drug effects."[14]
- Diarrhea
- Loss of appetite
- Fatigue
- Rarely, interstitial pneumonitis, which is characterized by cough and increased dyspnea. This may be severe and must be considered among those patients whose breathing acutely worsens.
- Rarely, ingrown hairs, such as eyelashes
- It has also been suggested that erlotinib can cause hearing loss.
- Partial hair loss (by strands, not typically in clumps)
Rare side effects
In spring 2009, the US Food and Drug Administration issued a warning on erlotinib. The FDA reported serious gastrointestinal tract, skin, and ocular disorders in patients taking the drug. In addition, according to a letter released by Genentech and OSI Pharmaceuticals, some people prescribed erlotinib have developed serious or fatal gastrointestinal tract perforations; "bullous, blistering, and exfoliative skin conditions, some fatal; and serious eye problems such as corneal lesions. Some of the cases, including ones which resulted in death, were suggestive of Stevens-Johnson syndrome/toxic epidermal necrolysis.[15]
Resistance to treatment
A key issue with EGFR-directed treatments is that after a period of time, frequently 8–12 months, the cancer cells become resistant to the treatment. The primary source of resistance is a second mutation called T790M. A second source of resistance is the MET mutation.[16]
Chemically resistance appears to occur by recruiting a mutated IGF-1 receptor to act as one of the EGFR partners in the homodimer, so forming a heterodimer.[17] This allows the signal to be transmitted even in the presence of an EGFR inhibitor. Some IGR-1R inhibitors are in various stages of development (based either around tyrphostins such as AG1024 or AG538[18] or pyrrolo[2,3-d]-pyrimidine derivatives such as NVP-AEW541[19]).
Pan-inhibitors show some promise in combating resistance, at least in cell studies. Today (3/10) the most promising approach to combating resistance appears to be a dual approach, combining pan-inhibitors like HKI 272 with Erbitux. "Surprisingly, we found that only the combination of both agents together induced dramatic shrinkage of erlotinib-resistant tumors harboring the T790M mutation, because together they efficiently depleted both phosphorylated and total EGFR. We suggest that these studies have immediate therapeutic implications for lung cancer patients, as dual targeting with cetuximab (Erbitux) and a second-generation EGFR TKI may be an effective strategy to overcome T790M-mediated drug resistance." Dual targeting of EGFR can overcome a major drug resistance mutation in mouse models of EGFR mutant lung cancer.[20]
Notes
http://www.cancer.gov/clinicaltrials/results/lung-and-erlotinib0604l http://www.roche.com/med-cor-2007-10-22 http://www.roche.com/med-cor-2009-05-30b http://www.cipla.com/whatsnew/news.htm#27apr09 http://www.cipla.com/whatsnew/news.htm#20mar08
References
- ^ Raymond E, Faivre S, Armand J (2000). "Epidermal growth factor receptor tyrosine kinase as a target for anticancer therapy". Drugs 60 Suppl 1: 15–23; discussion 41–2. PMID 11129168.
- ^ 2009 - SATURN: A double-blind, randomized, phase III study of maintenance erlotinib versus placebo following nonprogression with first-line platinum-based chemotherapy in patients with advanced NSCLC.
- ^ April 2010 - Tarceva Indication Announcement Letter
- ^ http://www.nice.org.uk/newsroom/pressreleases/ErlotinibForNonSmallCellLungCancer.jsp NICE unable to recommend erlotinib for the maintenance treatment of non-small-cell lung cancer]
- ^ Erlotinib for Advanced NSCLC is "Marginally" Cost Effective, Fran Lowry, Medscape, 25 February 2010
- ^ Takimoto CH, Calvo E. "Principles of Oncologic Pharmacotherapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ^ Li Z, Xu M, Xing S, Ho W, Ishii T, Li Q, Fu X, Zhao Z (2007). "Erlotinib Effectively Inhibits JAK2V617F Activity and Polycythemia Vera Cell Growth". J Biol Chem 282 (6): 3428–32. doi:10.1074/jbc.C600277200. PMC 2096634. PMID 17178722. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2096634.
- ^ http://drugpatentwatch.com/ultimate/preview/ingredient/index.php?query=erlotinib
- ^ http://sify.com/finance/equity/fullstory.php?id=14626687
- ^ http://sify.com/finance/equity/fullstory.php?id=14612495
- ^ http://www.cipla.com/whatsnew/news.htm#27apr09
- ^ Dudek A, Kmak K, Koopmeiners J, Keshtgarpour M (2006). "Skin rash and bronchoalveolar histology correlates with clinical benefit in patients treated with gefitinib as a therapy for previously treated advanced or metastatic non-small cell lung cancer". Lung Cancer 51 (1): 89–96. doi:10.1016/j.lungcan.2005.09.002. PMID 16290256.
- ^ Román Pérez-Soler, M.D., et al. (2004). "Selected Highlights". Lung Cancer Frontiers 22 (16): 3238–3247.
- ^ Thomas L. Petty, M.D. (2003). "Determinants of Tumor Response and Survival With Erlotinib in Patients With Non—Small-Cell Lung Cancer". Journal of Clinical Oncology 1 (17): 3–4.
- ^ http://jama.ama-assn.org/cgi/content/extract/301/24/2542-b
- ^ Dr Dubey; Dr Howard L. (Jack) West (03 2009). "Learning from the Tumor: When Drugs Stop Working". GRACE::Lung Cancer. Seattle, WA: Global Resource for Advancing Cancer Education (GRACE). http://cancergrace.org/lung/2009/03/09/sd-egfr-mechs-of-resistance/. Retrieved 26 February 2011. "... the tumor develops a secondary mutation that was described as T790M mutation. This new mutation blocks the binding of tarceva in the tumor so that tarceva cannot work anymore. ... MET is a gene that helps tumor grow. ... European investigators studied lung tumors that were removed from people who had lung cancer surgery... survival was shorter when high amounts of MET was present in the tumor.... T790M and MET are the biggest reasons why drugs like tarceva eventually stop working."
- ^ Jones H, Goddard L, Gee J, Hiscox S, Rubini M, Barrow D, Knowlden J, Williams S, Wakeling A, Nicholson R (2004). "Insulin-like growth factor-I receptor signalling and acquired resistance to gefitinib (ZD1839; Iressa) in human breast and prostate cancer cells". Endocr Relat Cancer 11 (4): 793–814. doi:10.1677/erc.1.00799. PMID 15613453. http://erc.endocrinology-journals.org/cgi/content/full/11/4/793. Free full text
- ^ Blum G, Gazit A, Levitzki A (2000). "Substrate competitive inhibitors of IGF-1 receptor kinase". Biochemistry 39 (51): 15705–12. doi:10.1021/bi001516y. PMID 11123895.
- ^ Warshamana-Greene G, Litz J, Buchdunger E, García-Echeverría C, Hofmann F, Krystal G (2005). "The insulin-like growth factor-I receptor kinase inhibitor, NVP-ADW742, sensitizes small cell lung cancer cell lines to the effects of chemotherapy". Clin Cancer Res 11 (4): 1563–71. doi:10.1158/1078-0432.CCR-04-1544. PMID 15746061. Free full text
- ^ J Clin Invest. 2009 October 1; 119(10). Tang, Dual MET EGFR combinatorial inhibition against T790M-EGFR-mediated erlotinib-resistant lung cancer, Br J Cancer. 2008 September 16; 99(6)
External links
- Official Tarceva website
- Tarceva Discussion Group for Cancer Patients
- Sordella R, Bell DW, Haber DA, Settleman J (August 2004). "Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways". Science 305 (5687): 1163–7. doi:10.1126/science.1101637. PMID 15284455..
- Genzyme "Genzyme Launches Exclusive Lung Cancer Test" Press Release September 27, 2005
- "Determinants of Tumor Response and Survival With Erlotinib in Patients With Non-Small-Cell Lung Cancer, Journal of Clinical Oncology, August 15, 2004.
- October 2003 issue of Lung Cancer Frontiers on rash/effectiveness correlation
- FAQ: I started an EGFR inhibitor two weeks ago but haven’t developed a rash. Does this mean it’s not working?, Dr. Howard L. (Jack) West, M.D., GRACE, February 21, 2011 (directed toward the layperson).
Targeted therapy / extracellular chemotherapeutic agents/antineoplastic agents (L01) CI monoclonal antibodies ("-mab") Others for solid tumorsTyrosine-kinase inhibitors ("-nib") ErbB: HER1/EGFR (Erlotinib, Gefitinib, Vandetanib) • HER1/EGFR and HER2/neu (Afatinib, Lapatinib, Neratinib)
RTK class III: C-kit and PDGFR (Axitinib, Pazopanib, Sunitinib, Sorafenib, Toceranib) • FLT3 (Lestaurtinib)
VEGFR (Axitinib, Cediranib, Pazopanib, Regorafenib, Semaxanib, Sorafenib, Sunitinib, Toceranib, Vandetanib)Other fusion protein against VEGF (Aflibercept) • proapoptotic peptide against ANXA2 and prohibitin (Adipotide) • exotoxin against IL-2 (Denileukin diftitox)M: NEO
tsoc, mrkr
tumr, epon, para
drug (L1i/1e/V03)
Categories:- Receptor tyrosine kinase inhibitors
- Quinazolines
- Alkynes
- Amines
- Ethers
- Phenol ethers
Wikimedia Foundation. 2010.
