- Phrenic nerve
-
Nerve: Phrenic nerve 
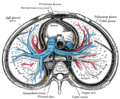
The phrenic nerve and its relations with the vagus nerve. (Phrenic labeled at upper left.) 
Plan of the cervical plexus. (Phrenic labeled at bottom right.) Latin nervus phrenicus Gray's subject #210 928 Innervates Diaphragm From C3-C5 of cervical plexus The phrenic nerve (Ancient Greek: φρήν phrēn "mind") originates mainly from the 4th cervical nerve, but also receives contributions from the 5th and 3rd cervical nerves (C3-C5) in humans.[1]
The phrenic nerves contain motor, sensory, and sympathetic nerve fibers. These nerves provide the only motor supply to the diaphragm as well as sensation to the central tendon. In the thorax, each phrenic nerve supplies the mediastinal pleura and pericardium.
The contribution of the C5 nerve to the phrenic nerve may be derived from an accessory phrenic nerve. Frequently, it is a branch of the nerve to the subclavius. If present, the accessory phrenic nerve lies lateral to the main nerve and descends posterior and sometimes anterior to the subclavian vein. The accessory phrenic nerve joins the phrenic nerve either in the root of the neck or in the thorax.
Contents
Path
The phrenic nerve descends obliquely with the IJV across the anterior scalene, deep to the prevertebral layer of deep cervical fascia and the transverse cervical and suprascapular arteries. On the left; the phrenic nerve crosses anterior to the first part of the subclavian artery. On the right; it lies on the anterior scalene muscle and crosses anterior to the 2nd part of the subclavian artery. On both sides, the phrenic nerve runs posterior to the subclavian vein and anterior to the internal thoracic artery as it enters the thorax.
Found in the middle mediastinum, both phrenic nerves run from C3, C4 and C5 along the anterior scalene muscle deep to the carotid sheath.
- The right phrenic nerve passes over the brachiocephalic artery, posterior to the subclavian vein, and then crosses the root of the right lung anteriorly and then leaves the thorax by passing through the vena cava hiatus opening in the diaphragm at the level of T8. The right phrenic nerve passes over the right atrium.
- The left phrenic nerve passes over the pericardium of the left ventricle and pierces the diaphragm separately.
On both sides the phrenic nerve runs posterior to the subclavian vein and posterior to the internal thoracic artery as it enters the thorax where it runs anterior to the root of the lung and into the pericardium between the fibrous and parietal layers.[1]
Both of these nerves supply motor fibres to the diaphragm and sensory fibres to the fibrous pericardium, mediastinal pleura, and diaphragmatic peritoneum.
The pericardiacophrenic arteries and veins travel with their respective phrenic nerves.
The contribution of the 5th cervical nerve may stem from an accessory phrenic nerve. Most often it is a branch of the nerve to the subclavius and may contain numerous phrenic nerve fibers. If the accessory phrenic nerve is present it lies lateral to the main nerve and descends posterior and occasionally inferior to the subclavian vein. The accessory phrenic nerve connects to the phrenic nerve in the thorax or the root of the neck.[1]
Clinical relevance
Pain arising from structures served by the phrenic nerve is often "referred" to other somatic regions served by spinal nerves C3-C5. For example, a subphrenic abscess beneath the right diaphragm might cause a patient to feel pain in the right shoulder (Kehr's sign). Irritation of the phrenic nerve (or the tissues supplied by it) leads to the hiccough reflex. A hiccough is a spasmodic contraction of the diaphragm, which pulls air against the closed folds of the larynx.
The phrenic nerve must be identified during thoracic surgery and preserved. It passes anterior to the hilum of the corresponding lung, and therefore can be identified easily. The right phrenic nerve may be crushed by the vena cava clamp during liver transplantation.[2] Severing the phrenic nerve, or a phrenectomy,[3] will paralyse that half of the diaphragm. Diaphragm paralysis is best demonstrated by sonography.[4] Breathing will be made more difficult but will continue provided the other nerve is intact.
Fortunately, the phrenic nerve arises from the neck (C3-C5) and innervates the diaphragm, which is much lower. Hence, patients who suffer spinal cord injuries below the neck are still able to breathe effectively, despite any paralysis of the lower limbs.
Additional images
References
- ^ a b c Moore, Keith L. (1999). Clinically oriented anatomy. Philadelphia: Lippincott Williams & Wilkins. ISBN 0-683-06141-0.
- ^ Vivian C. McAlister, David R. Grant, Andre Roy, William F. Brown, Linda C. Hutton, David J. Leasa, Cameron N. Ghent, James E. Veitch, and William J. Wall. "Right Phrenic Nerve Injury in Orthotopic Liver Transplantation" Transplantation 55.4 (1993): 826-830.
- ^ Hine, Maynard Kiplinger (1975). Review of dentistry: questions and answers (6 ed.). Mosby. pp. 421. ISBN 0801621968. http://books.google.com/books?id=OPJpAAAAMAAJ&q=Phrenectomy+-wikipedia&dq=Phrenectomy+-wikipedia&client=firefox-a&pgis=1. Retrieved May 13, 2008.
- ^ Vivian C. McAlister, David R. Grant, Andre Roy, William F. Brown, Linda C. Hutton, David J. Leasa, Cameron N. Ghent, James E. Veitch, and William J. Wall. "Right Phrenic Nerve Injury in Orthotopic Liver Transplantation" Transplantation 55.4 (1993): 826-830.
External links
- -1402273763 at GPnotebook
- Phrenic+nerve at eMedicine Dictionary
- SUNY Figs 19:04-05 - "Left side of the mediastinum."
- SUNY Figs 25:03-15 - "Diagram of the cervical plexus."
Nerves of head and neck: the cervical plexus (C1–C4) (TA A14.2.02, GA 9.926) superficial deep Categories:- Nerves of the head and neck
Wikimedia Foundation. 2010.