- Signs and symptoms of Parkinson's disease
-
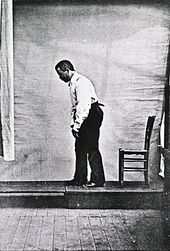
 Illustration of the Parkinson disease by Sir William Richard Gowers from A Manual of Diseases of the Nervous System in 1886 showing the characteristic posture of PD patients
Illustration of the Parkinson disease by Sir William Richard Gowers from A Manual of Diseases of the Nervous System in 1886 showing the characteristic posture of PD patients
Signs and symptoms of Parkinson's disease are varied. Parkinson's disease affects movement, producing motor symptoms.[1] Non-motor symptoms, which include autonomic dysfunction, cognitive and neurobehavioral problems, and sensory and sleep difficulties, are also common.[1]
Contents
Motor symptoms
Further information: Parkinsonian GaitFour motor symptoms are considered cardinal in PD: tremor, rigidity, slowness of movement, and postural instability.[1] Other motor symptoms include gait and posture disturbances such as decreased arm swing, a forward-flexed posture and the use of small steps when walking; speech and swallowing disturbances; and other symptoms such as a mask-like face expression or small handwriting are examples of the range of common motor problems that can appear.[1]
Cardinal symptoms
Four symptoms are considered cardinal in PD: tremor, rigidity, bradykinesia and postural instability.[1]
- Tremor is the most apparent and well-known symptom.[1] It is also the most common; though around 30% of individuals with PD do not have tremor at disease onset, most develop it as the disease progresses.[1] It is usually a rest tremor: maximal when the limb is at rest and disappearing with voluntary movement and sleep.[1] It affects to a greater extent the most distal part of the limb, and at onset typically appears in only a single arm or leg, becoming bilateral later.[1] Frequency of PD tremor is between 4 and 6 hertzs (cycles per second). It is a pronation-supination tremor that is described as "pill-rolling"; a term used to describe the tendency of the index finger of the hand to get into contact with the thumb and perform together a circular movement.[1][2] Such term was given due to the similarity of the movement in PD patients with the former pharmaceutical technique of manually making pills.[2] PD tremor is not improved with alcohol intake, as opposed to essential tremor.[1]
- Rigidity is a characterized by an increased muscle tone (an excessive and continuous contraction of the muscles) which produces stiffness and resistance to movement in joints.[1] Rigidity may be associated with joint pain; such pain being a frequent initial manifestation of the disease.[1] When limbs of the person with PD are passively moved by others a "cogwheel rigidity" is commonly seen.[1] Cogwheel-like refers to the ratchety jerks by which the articulation is moved as opposed to the normal fluid movement: when a muscle is externally tried to move it resists at first but with enough force it is partially moved until it resists again and only with further force it will be moved.[1][3][4] The combination of tremor and increased tone is considered to be at the origin of cogwheel rigidity.[5]
- Bradykinesia and akinesia: the former refers to slowness of movement while the latter to the absence of it.[1] It is the most characteristic clinical feature of PD, and is associated with difficulties along the whole course of the movement process, from planning to initiation and finally execution of a movement.[1] The performance of sequential and simultaneous movements is also hindered.[1] Bradykinesia is the most disabling symptom in the early stages of the disease.[3] Initial manifestations of bradykinesia are problems when performing daily life tasks requiring fine motor control such as writing, sewing or getting dressed.[1] Clinical evaluation is based in similar tasks consisting such as alternating movements between both hands or feet.[3] Bradykinesia is not equal for all movements or times. It is modified by the activity or emotional state of the subject to the point of some patients barely able to walk being capable of riding a bicycle.[1] Generally patients have less difficulties when some short of external cue is provided.[1][6]
... immobile patients who become excited may be able to make quick movements such as catching a ball (or may be able to suddenly run if someone screams "fire"). This phenomenon (kinesia paradoxica) suggests that patients with PD have intact motor programmes but have difficulties accessing them without an external trigger, such as a loud noise, marching music or a visual cue requiring them to step over an obstacle.[1]
- Postural instability: In the late stages postural instability is typical, which leads to impaired balance and frequent falls, and secondarily to bone fractures.[1] Instability is often absent in the initial stages, especially in younger people.[3] Up to 40% of the patients may experience falls and around 10% may have falls weekly, with number of falls being related to the severity of PD. It is produced by a failure of postural reflexes, along other disease related factors such as orthostatic hypotension or cognitive and sensory changes[1]
Other motor symptoms
 Drawing of a Parkinson's disease patient face showing hypomimia. Depiction appeared in Nouvelle iconographie de la Salpétrière, vol 1 (1888)
Drawing of a Parkinson's disease patient face showing hypomimia. Depiction appeared in Nouvelle iconographie de la Salpétrière, vol 1 (1888)
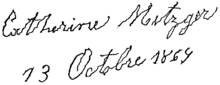 Example of writing by a patient with Parkinson's disease; possibly showing micrographia in addition to other abnormal characteristics. Published by Jean-Martin Charcot in 1879. Text accompanying image stated "The strokes forming the letters are very irregular and sinuous, whilst the irregularities and sinuosities are of a very limited width. On a careful examination of this specimen of writing it will be perceived that the down-strokes are all, with the exception of the first letter, made with comparative firmness and are, in fact, nearly normal — the finer up-strokes, on the contrary, are all tremulous in appearance, and it is to the unsteadiness of these lines that the peculiar character of the writing here is principally due."
Example of writing by a patient with Parkinson's disease; possibly showing micrographia in addition to other abnormal characteristics. Published by Jean-Martin Charcot in 1879. Text accompanying image stated "The strokes forming the letters are very irregular and sinuous, whilst the irregularities and sinuosities are of a very limited width. On a careful examination of this specimen of writing it will be perceived that the down-strokes are all, with the exception of the first letter, made with comparative firmness and are, in fact, nearly normal — the finer up-strokes, on the contrary, are all tremulous in appearance, and it is to the unsteadiness of these lines that the peculiar character of the writing here is principally due."
Other motor symptoms include:
- Gait and posture disturbances:
- Shuffling gait:[1] gait is characterized by short steps, with feet barely leaving the ground. Small obstacles tend to cause the patient to trip.
- Decreased arm-swing.[1]
- Turning "en bloc": rather than the usual twisting of the neck and trunk and pivoting on the toes, PD patients keep their neck and trunk rigid, requiring multiple small steps to accomplish a turn.
- Camptocormia:[1] stooped, forward-flexed posture. In severe forms, the head and upper shoulders may be bent at a right angle relative to the trunk.[7]
- Festination:[1] a combination of stooped posture, imbalance, and short steps. It leads to a gait that gets progressively faster and faster, often ending in a fall.
- Gait freezing: also called motor blocks, is a manifestation of akinesia.[1] Gait freezing is characterized by a sudden inability to move the lower extremities which usually lasts less than 10 seconds.[1] It may worsen in tight, cluttered spaces, when attempting to initiate gait or turning around, or when approaching a destination.[1] Freezing improves with treatment and also with behavioral techniques such as marching to command or following a given rhythm.[1]
- Dystonia:[1] abnormal, sustained, painful twisting muscle contractions, often affecting the foot and ankle (mainly toe flexion and foot inversion) which often interferes with gait.
- Scoliosis[1]
- Speech and swallowing disturbances.
- Hypophonia:[1] soft speech.
- Monotonic speech: Speech quality tends to be soft, hoarse, and monotonous.[1]
- Festinating speech: excessively rapid, soft, poorly-intelligible speech.
- Drooling: most likely caused by a weak, infrequent swallow.[1]
- Dysphagia: impaired ability to swallow; which in the case of PD is probably related to an inability to initiate the swallowing reflex or by a too long laryngeal or oesophageal movement.[1] Can lead to aspiration pneumonia.
- Dysarthria[1]
- Other motor symptoms and signs:
- Fatigue
- Hypomimia:[1] a mask-like face
- Difficulty rolling in bed or rising from a seated position.[1]
- Micrographia:[1] small, cramped handwriting.
- Impaired fine motor dexterity and motor coordination.[1]
- Impaired gross motor coordination.
- Akathisia: an unpleasant desire to move.
- Reemergence of primitive reflexes.[1]
- Glabellar reflex
Neuropsychiatric
Example of reported prevalences of mood problems in PD patients with dementia[1][8] Mood problem Prevalence Depression 58% Apathy 54% Anxiety 49%  Pathologic gambling can appear in PD patients as a manifestation of a dopamine dysregulation syndrome
Pathologic gambling can appear in PD patients as a manifestation of a dopamine dysregulation syndrome
Parkinson's disease causes neuropsychiatric disturbances, which include mainly cognition, mood and behavior problems and can be as disabling as motor symptoms.[1]
Cognitive disturbances occur even in the initial stages of the disease in some cases.[9] A very high proportion of sufferers will have mild cognitive impairment as the disease advances.[1] Most common deficits in non-demented patients are:
- Executive dysfunction, which translates into impaired set shifting, poor problem solving, and fluctuations in attention among other difficulties.[9]
- Slowed cognitive speed (Bradyphrenia).[9]
- Memory problems; specifically in recalling learned information, with an important improvement with cues. Recognition is less impaired than free recall pointing towards a retrieving more than to an encoding problem.[9]
- Regarding language, patients are found to have problems in verbal fluency tests.[9]
- Visuospatial skills difficulties, which are seen when the person with PD is for example asked to perform tests of facial recognition and perception of line orientation.[9]
Deficits tend to aggravate with time, developing in many cases into dementia. A person with PD has a sixfold increased risk of suffering it,[1] and the overall rate in people with the disease is around 30%.[9] Moreover, prevalence of dementia increases in relation to disease duration, going up to 80%.[9] Dementia has been associated with a reduced quality of life in disease sufferers and caregivers, increased mortality and a higher probability of attending a nursing home.[9]
Cognitive problems and dementia are usually accompanied by behavior and mood alterations, although these kind of changes are also more common in those patients without cognitive impairment than in the general population. Most frequent mood difficulties include:[1]
- Depression:[1] Depression is well recognized in PD, having been identified as "melancholia" by James Parkinson in his original report of the disease in 1817. Estimated prevalence rates of depression vary widely according to the population sampled and methodology used although prevalence at a given time is most probably around 31%; which doubles the numbers in the general population.[10] There is an increased risk for any individual with depression to go on to develop Parkinson's disease at a later date.[10][11] It is increasingly thought to be a consequence of the disease rather than an emotional reaction to disability.[12] Since Parkinson's affects many areas of the brain that control mood (specifically the frontal lobe as well as those areas that produce serotonin, norepinephrine and dopamine), depression may result.[13] Depression is one of the most common neuropsychiatric conditions found in patients who have Parkinson's disease, and it is associated with more rapid progression of physical symptoms and a greater decline in cognitive skills. Depression in patients with PD was found to be more predictive of overall disability than was the motor disability from the PD. An interesting finding is that although there is a high rate of depression in patients with PD, the incidence of suicide is lower in this group of patients.[14] Many of the symptoms of PD may overlap with those of depression, making diagnosis a difficult issue.[15]
- Apathy[1]
- Anxiety:[1] Seventy percent of individuals with Parkinson's disease diagnosed with pre-existing depression go on to develop anxiety. Ninety percent of Parkinson's disease patients with pre-existing anxiety subsequently develop depression; apathy or abulia.
Obsessive–compulsive behaviors such as craving, binge eating, hypersexuality, pathological gambling, or other, can also appear in PD, and have been related to a dopamine dysregulation syndrome associated with the medications for the disease.[1]
Psychotic symptoms are common in PD, generally associated with dopamine therapy. Symptoms of psychosis, or impaired reality testing, are either hallucinations, typically visual, less commonly auditory, and rarely in other domains including tactile, gustatory or olafactory, or delusions, that is, irrational beliefs. Hallucinations are generally stereotyped and without emotional content. Initially patients usually have insight so that the hallucinations are benign in terms of their immediate impact but have poor prognostic implications, with increased risk of dementia, worsened psychotic symptoms and mortality. Delusions occur in about 5-10% of treated patients, and are considerably more disruptive, being paranoid in nature, of spousal infidelity or family abandonment. Psychosis is an independent risk factor for nursing home placement.[16]
Hallucinations can occur in Parkinsonian syndromes for a variety of reasons. There is an overlap between Parkinson's disease and Lewy body dementia, so that where Lewy bodies are present in the visual cortex, hallucinations may result. Hallucinations can also be brought about by excessive dopaminergic stimulation. Most hallucinations are visual in nature, often formed as familiar people or animals, and are generally non-threatening in nature. Some patients find them comforting; however their carers often find this part of the disease most disturbing and the occurrence of hallucinations is a major risk factor for hospitalisation. Treatment options consist of modifying the dosage of dopaminergic drugs taken each day, adding an antipsychotic drug like quetiapine, or offering carers a psychosocial intervention to help them cope with the hallucinations.
Sleep
 Rapid eye movement sleep (REM) is altered in PD as opposed to the shown EEG polysomnographic record representing normal REM
Rapid eye movement sleep (REM) is altered in PD as opposed to the shown EEG polysomnographic record representing normal REM
Sleep problems can be worsened by medications for PD, but they are a core feature of the disease.[1] Some common symptoms are:
- Excessive daytime somnolence.[1]
- Insomnia, characterized mostly by sleep fragmentation.[1]
- Disturbances in REM sleep: disturbingly vivid dreams, and rapid eye movement behavior disorder, characterized by acting out of dream content.[1] It appears in a third of the patients and it is a risk factor for Parkinson's disease in the overall population.[1]
Perception
- Impaired proprioception (the awareness of bodily position in three-dimensional space).
- Reduction or loss of sense of smell (hyposmia or anosmia).[1] It may be an early marker of the disease.[1]
- Pain:[1] neuropathic, muscle, joints, and tendons, attributable to tension, dystonia, rigidity, joint stiffness, and injuries associated with attempts at accommodation.
- Paresthesias.[1]
Autonomic
- Orthostatic hypotension,[1] leading to dizziness and fainting
- Oily skin[17]
- Urinary incontinence[1] (typically in later disease progression) and nocturia (getting up in the night to pass urine)
- Altered sexual function:[1] characterized by profound impairment of sexual arousal, behavior, orgasm, and drive is found in mid and late Parkinson disease.
- Excessive sweating[1]
Gastrointestinal
Parkinson' disease causes constipation and gastric dysmotility that is severe enough to endanger comfort and even health.[18] A factor in this is the appearance of Lewy bodies and Lewy neurites even before these affect the functioning of the substantia nigra in the neurons in the enteric nervous system that control gut functions.[19]
Neuro-ophthalmological
PD is related to different ophthalmological abnormalities produced by the neurological changes.[1][20] Among them are:
- Decreased blink rate[1]
- Irritation of the eye surface[1]
- Alteration in the tear film[1]
- Visual hallucinations[1]
- Decreased eye convergence[1]
- Blepharospasm[1]
- Abnormalities in ocular pursuit and saccadic movements[1]
- Difficulties to open the eye-lids[1] This can have particular relevance when driving. People with Parkinson's have been shown to be less accurate in spotting landmarks and roadsigns whilst driving.[21]
- Limitations in the upward gaze[1]
- Blurred vision[20]
- Diplopia (double vision), produced by a reduced eye convergence.[20]
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt bu bv bw bx Jankovic J (April 2008). "Parkinson's disease: clinical features and diagnosis". J. Neurol. Neurosurg. Psychiatr. 79 (4): 368–76. doi:10.1136/jnnp.2007.131045. PMID 18344392. http://jnnp.bmj.com/content/79/4/368.full.
- ^ a b Cooper G, Eichhorn G, Rodnitzky RL (2008). "Parkinson's disease". In Conn PM. Neuroscience in medicine. Totowa: Humana Press. pp. 508–512. ISBN 978-1-60327-455-8.
- ^ a b c d Samii A, Nutt JG, Ransom BR (May 2004). "Parkinson's disease". Lancet 363 (9423): 1783–93. doi:10.1016/S0140-6736(04)16305-8. PMID 15172778.
- ^ Banich MT, Compton RJ (2011). "Motor control". Cognitive neuroscience. Belmont, CA: Wadsworth, Cengage learning. pp. 108–44. ISBN 0-8400-3298-6.
- ^ Fung VSC, Thompson PD (2007). "Rigidity and spasticity". In Tolosa E, Jankovic JJ. Parkinson's disease and movement disorders. Hagerstown, MD: Lippincott Williams & Wilkins. pp. 504–13. ISBN 0-7817-7881-6.
- ^ Rodriguez-Oroz MC, Jahanshahi M, Krack P, et al. (December 2009). "Initial clinical manifestations of Parkinson's disease: features and pathophysiological mechanisms". Lancet Neurol 8 (12): 1128–39. doi:10.1016/S1474-4422(09)70293-5. PMID 19909911.
- ^ Lepoutre A, Devos D, Blanchard-Dauphin A, et al (2006). "A specific clinical pattern of camptocormia in Parkinson's disease". J. Neurol. Neurosurg. Psychiatr. 77 (11): 1229–34. doi:10.1136/jnnp.2005.083998. PMC 2077366. PMID 16735399. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2077366.
- ^ Aarsland D, Brønnick K, Ehrt U, et al. (January 2007). "Neuropsychiatric symptoms in patients with Parkinson's disease and dementia: frequency, profile and associated care giver stress". Journal of Neurology, Neurosurgery, and Psychiatry 78 (1): 36–42. doi:10.1136/jnnp.2005.083113. PMC 2117797. PMID 16820421. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2117797.
- ^ a b c d e f g h i Caballol N, Martí MJ, Tolosa E (September 2007). "Cognitive dysfunction and dementia in Parkinson disease". Mov. Disord. 22 Suppl 17: S358–66. doi:10.1002/mds.21677. PMID 18175397.
- ^ a b Lieberman A (January 2006). "Depression in Parkinson's disease -- a review". Acta Neurologica Scandinavica 113 (1): 1–8. doi:10.1111/j.1600-0404.2006.00536.x. PMID 16367891.
- ^ Ishihara L, Brayne C (April 2006). "A systematic review of depression and mental illness preceding Parkinson's disease". Acta Neurologica Scandinavica 113 (4): 211–20. doi:10.1111/j.1600-0404.2006.00579.x. PMID 16542159.
- ^ McDonald W; Richard, IH; Delong, MR (2003). "Prevalence, Etiology, and Treatment of Depression in Parkinson’s Disease". Biol Psychiatry 54 (3): 363–375. doi:10.1016/S0006-3223(03)00530-4. PMID 12893111.
- ^ Menza, Matthew Combating Depression in Parkinson's Disease. Parkinson's Disease Foundation News & Review. Spring 2009.
- ^ Menza MA. Psychiatric symptoms associated with Parkinson disease. Drug Benefit Trends. 2010;22:58-60.
- ^ The National Collaborating Centre for Chronic Conditions, ed (2006). "Non-motor features of Parkinson’s disease". Parkinson's Disease. London: Royal College of Physicians. pp. 113–33. ISBN 1-86016-283-5. http://guidance.nice.org.uk/CG35/Guidance/pdf/English.
- ^ Friedman JH (June 2010). "Parkinson's disease psychosis 2010: A review article". Parkinsonism Relat Disord 16 (9): 553–60. doi:10.1016/j.parkreldis.2010.05.004. PMID 20538500.
- ^ Gupta AK, Bluhm R (January 2004). "Seborrheic dermatitis". Journal of the European Academy of Dermatology and Venereology 18 (1): 13–26; quiz 19–20. doi:10.1111/j.1468-3083.2004.00693.x. PMID 14678527.
- ^ Pfeiffer RF (February 2003). "Gastrointestinal dysfunction in Parkinson's disease". Lancet Neurology 2 (2): 107–16. doi:10.1016/S1474-4422(03)00307-7. PMID 12849267.
- ^ Lebouvier T, Chaumette T, Paillusson S, et al. (September 2009). "The second brain and Parkinson's disease". The European Journal of Neuroscience 30 (5): 735–41. doi:10.1111/j.1460-9568.2009.06873.x. PMID 19712093.
- ^ a b c Armstrong RA (March 2008). "Visual signs and symptoms of Parkinson's disease". Clin Exp Optom 91 (2): 129–38. doi:10.1111/j.1444-0938.2007.00211.x. PMID 18271776.
- ^ Uc EY; Rizzo, M; Anderson, SW; Sparks, J; Rodnitzky, RL; Dawson, JD (2006). "Impaired visual search in drivers with Parkinson's disease". Annals of Neurology 6 (4): EPub ahead of print. doi:10.1002/ana.20958. PMID 16969860.
Categories:
Wikimedia Foundation. 2010.