- Chondrocalcinosis
-
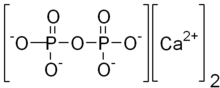
Chondrocalcinosis Classification and external resources 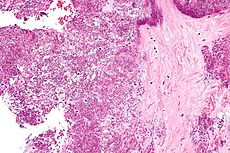
Micrograph showing crystal deposition in an intervertebral disc. H&E stain.ICD-10 M11.1-M11.2 ICD-9 712.3 OMIM 600668 118600 DiseasesDB 10832 DDB 30784 MedlinePlus 000421 eMedicine med/1938 radio/125 orthoped/382 emerg/221 MeSH D002805 Calcium pyrophosphate dihydrate disease (CPPD) is a rheumatologic disorder with varied symptoms arising due to the accumulation of crystals of calcium pyrophosphate dihydrate in the connective tissues. It is more commonly known by alternative names that specify certain clinical or radiographic findings, although neither is synonymous with CPPD. Pseudogout refers to the acute symptoms of joint inflammation or synovitis: red, tender, and swollen joints that may resemble gouty arthritis (a similar condition in which monosodium urate crystals are deposited within the joints). Chondrocalcinosis,[1][2] on the other hand, refers to the radiographic evidence of calcification in hyaline and/or fibrocartilage. Pyrophosphate arthropathy is a term that may refer to either of the above.[3] Statistically, the knee joint is the most commonly affected.[1]
Contents
General
CPPD crystal deposition disease is a polyarticular arthritis (i.e., it leads to an inflammation of several joints in the body), although it may begin as monoarticular (i.e., confined to just one joint).[4] CPPD crystals tend to form within articular tissues.[4] Although, in theory, any joint may be affected, statistics show that the knees, wrists, and hips are the most commonly attributed areas.[2] In rare cases, pseudogout may affect the spinal canal and cause damage to the spinal cord.[5] The exact cause of CPPD is unknown, although increased breakdown of adenosine triphosphate (the molecule used as energy currency in all animals), which results in increased pyrophosphate levels in joints, is thought to be one reason why crystals may develop.[2] There is some recent evidence suggesting that the gene ANKH is involved in crystal-related inflammatory reactions and inorganic phosphate transport.[2] Excessive calcium (due to hypomagnesemia) has a potential relationship with chondrocalcinosis, and magnesium supplementation may reduce or alleviate symptoms.[6]
One genetic study found an association between chondrocalcinosis and a region of chromosome 8q.[7]
Signs and symptoms
People with this disorder usually first go to the doctor because inflammation is causing pain in one or more joints.[2] Hyperparathyroidism, hypothyroidism, hemochromatosis, hypophosphatemia, hypomagnesemia and renal osteodystrophy are often also associated with chondrocalcinosis.[2] Other diseases associated with chondrocalcinosis are Wilson's disease and osteoarthritis. In some cases, traumatic arthritis can cause chondrocalcinosis.[2][4] In general, the white blood cell count is raised.[2] In rare instances, patients may also have signs of carpal tunnel syndrome.[2] This condition can also be associated with Milwaukee Shoulder. On microscopic investigation with crossed polarizing filters of joint fluid obtained by aspiration, rhombus-shaped, positively birefringent crystals on Congo red stain may be seen.
Diagnosis
Radiography has a large role to play in the diagnosis of chondrocalcinosis, with radiographs, CT scans, MRIs, ultrasound, and nuclear medicine all having a part.[1] CT scans and MRIs show calcific masses (usually within the ligamentum flavum or joint capsule), however radiography is more successful.[1] As with most conditions, chondrocalcinosis can present with similarity to other diseases such as ankylosing spondylitis and gout.[1][2] Arthrocentesis, or removing synovial fluid from the affected joint, is performed to test the synovial fluid for the calcium pyrophosphate crystals that are present in CPPD.
Treatment
Because any medication that could reduce the inflammation of chondrocalcinosis bears a risk of causing organ damage, treatment is not advised if the condition is not causing pain.[2] For acute pseudogout, intra-articular corticosteroid injection, systemic corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), or, on occasion, high-dose colchicine.[2] In general, NSAIDs are administered in low doses to help prevent chondrocalcinosis. However, if an acute attack is already occurring, higher doses are administered.[2] If nothing else works, hydroxychloroquine or methotrexate may provide relief.[8] Research into surgical removal of calcifications is underway, however this still remains an experimental procedure.[2]
Epidemiology
CPPD affects people of all cultures and ethnic origins, and, in the United States, around 50% of the population over 85 years of age are affected.[2] It may cause considerable pain, but it is never fatal[2] Women are at a slightly higher risk than men, with an estimated ratio of occurrence of 1.4:1 respectively.[2]
References
- ^ a b c d e Rothschild, Bruce M Calcium Pyrophosphate Deposition Disease (radiology)
- ^ a b c d e f g h i j k l m n o p q Rothschild, Bruce M Calcium Pyrophosphate Deposition Disease (rheumatology) at eMedicine
- ^ Longmore, Murray; Ian Wilkinson, Tom Turmezei, Chee Kay Cheung (2007). Oxford Handbook of Clinicial Medicine. Oxford. p. 841. ISBN 0-19-856837-1.
- ^ a b c Wright GD, Doherty M (1997). "Calcium pyrophosphate crystal deposition is not always 'wear and tear' or aging". Ann. Rheum. Dis. 56 (10): 586–8. doi:10.1136/ard.56.10.586. PMC 1752269. PMID 9389218. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1752269.
- ^ Walid M S, Yelverton JC, Ajjan M, Grigorian AA. (2008). "Pseudogout of the thoracic spine mimicking a tumor. Crazy". Russian Neurosurgery Online. 1 (20).
- ^ de Filippi JP, Diderich PP, Wouters JM. (1992). "Hypomagnesemia and chondrocalcinosis". Ned Tijdschr Geneeskd 1 (20): 139–41. PMID 1732847.
- ^ Baldwin CT, Farrer LA, Adair R, Dharmavaram R, Jimenez S, Anderson L (March 1995). "Linkage of early-onset osteoarthritis and chondrocalcinosis to human chromosome 8q". Am. J. Hum. Genet. 56 (3): 692–7. PMC 1801178. PMID 7887424. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1801178.
- ^ Emkey GR and Reginato AM (2009). "All about gout and pseudogout". Journal of Musculoskeletal Medicine 26 (10). http://www.musculoskeletalnetwork.com/display/article/1145622/1476306.
External links
Musculoskeletal disorders: Arthropathies (M00–M19, 711–719) Arthritis
(monoarthritis/
polyarthritis)NoninfectiousRheumatoid arthritis: Juvenile idiopathic arthritis · Adult-onset Still's disease · Felty's syndromeNoninflammatoryOther hemorrhage (Hemarthrosis) · pain (Arthralgia) · Osteophyte · villonodular synovitis (Pigmented villonodular synovitis) · Joint stiffnessM: JNT
anat(h/c, u, t, l)/phys
noco(arth/defr/back/soft)/cong, sysi/epon, injr
proc, drug(M01C, M4)
Categories:- Arthritis
- Inflammatory polyarthropathies
- Musculoskeletal disorders
Wikimedia Foundation. 2010.