- Colorectal polyp
-
Colon polyps Classification and external resources 
Polyp of sigmoid colon as revealed by colonoscopy. Approximately 1 cm in diameter. The polyp was removed by snare cauteryICD-10 K63.5 & various MedlinePlus 000266 eMedicine med/414 MeSH C23.300.825  Gross appearance of a colectomy specimen containing two colorectal polyps and one invasive colorectal carcinoma
Gross appearance of a colectomy specimen containing two colorectal polyps and one invasive colorectal carcinoma
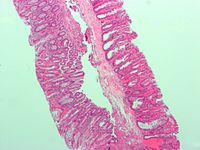
 Micrograph of a tubular adenoma, the most common type of dysplastic polyp in the colon.
Micrograph of a tubular adenoma, the most common type of dysplastic polyp in the colon.
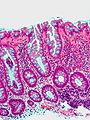
 Micrograph of a tubular adenoma – dysplastic epithelium (dark purple) on left of image; normal epithelium (blue) on right. H&E stain.
Micrograph of a tubular adenoma – dysplastic epithelium (dark purple) on left of image; normal epithelium (blue) on right. H&E stain.
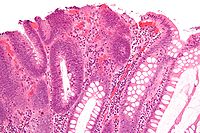
 Micrograph of a villous adenoma. These polyps are considered to have a high risk of malignant transformation. H&E stain.
Micrograph of a villous adenoma. These polyps are considered to have a high risk of malignant transformation. H&E stain.
A colorectal polyp is a polyp (fleshy growth) occurring on the lining of the colon or rectum.[1] Untreated colorectal polyps can develop into colorectal cancer.[2]
Colorectal polyps are often classified by their behaviour (i.e. benign vs. malignant) and/or etiology (e.g. as a consequence of inflammatory bowel disease). They may be benign (e.g. hyperplastic polyp), pre-malignant (e.g. tubular adenoma) or malignant (e.g. colorectal adenocarcinoma).
Contents
Types
The most common general classification is:
- hyperplastic,
- neoplastic (adenomatous & malignant),
- hamartomatous and,
- inflammatory.
Hyperplastic polyp
Most hyperplastic polyps are found in the distal colon and rectum.[3] They have no malignant potential [3], which means that they are no more likely than normal tissue to eventually become a cancer.
Hyperplastic polyps are serrated polyps. Hyperplastic polyps have three histologic patterns of growth: microvesicular, goblet cell and mucin poor.
Hyperplastic polyposis syndrome is a rare condition that has been defined by the World Health Organization as either:
-
- Five or more hyperplastic polyps proximal to the sigmoid colon, with two polyps greater than 10mm in diameter; or
- Any number of hyperplastic polyps proximal to the sigmoid colon in a person with a first degree relative who has hyperplastic polyposis syndrome; or
- More than 30 hyperplastic polyps of any size throughout the colon and rectum.[4]
Neoplastic polyp
A neoplasm is a tissue whose cells have lost its normal differentiation. They can be either benign growths or malignant growths. The malignant growths can either have primary or secondary causes.
Adenomas
Neoplastic polyps of the bowel are often benign hence called adenomas. An adenoma is tumor glandular tissue, that has not (yet) gained the properties of a cancer.
The common adenomas of the colon are the tubular, tubulovillous, villous, and sessile serrated (SSA).[3]
As is evident from their name, sessile serrated and traditional serrated adenomas (TSAs) have a serrated appearance and can be difficult to distinguish microscopically from hyperplastic polyps.[3] Making this distinction is important, however, since SSAs and TSAs have the potential to become cancers,[4] while hyperplastic polyps do not.[3]
The villous subdivision are associated with the highest malignant potential because they generally have the largest surface area. (This is because the villi are projections into the lumen and hence have a bigger surface area.) However, villous adenomas are no more likely than tubular or tubulovillous adenomas to become canerous if their sizes are all the same.[3]
Hamartomatous polyp
They are growths, like tumours found in organs as a result of faulty development. They are normally made up of a mixture of tissues. They grow at the normal rate of the host tissue and rarely cause problems such as compression. A common example of a hamartomatous lesion is a strawberry naevus. Hamartomatous polyps are often found by chance; occurring in syndromes such as Peutz-Jegher Syndrome or Juvenile Polyposis Syndrome.
Peutz-Jeghers syndrome is associated with polyps of the GI tract and also increased pigmentation around the lips, genitalia, buccal mucosa feet and hands. People are often diagnosed with Peutz-Jegher after presenting at around the age of 9 with an intussusception. The polyps themselves carry little malignant potential but because of potential coexisting adenomas there is a 15% chance of colonic malignancy.
Juvenile polyps are hamartomatous polyps which often become evident before twenty years of age, but can also be seen in adults. They are usually solitary polyps found in the rectum which most commonly present with rectal bleeding. Juvenile polyposis syndrome is characterised by the presence of more than five polyps in the colon or rectum, or numerous juvenile polyps throughout the gastrointestinal tract, or any number of juvenile polyps in any person with a family history of juvenile polyposis. People with juvenile polyposis have an increased risk of colon cancer.[4]
Inflammatory polyp
These are polyps which are associated with inflammatory conditions such as Ulcerative Colitis and Crohns disease.
Symptoms
Colorectal polyps are not usually associated with symptoms.[2] When they occur, symptoms include rectal bleeding, bloody stools, abdominal pain and fatigue.[2] A change in bowel habits may occur including constipation and diarrhoea.[5] Occasionally, if a polyp is big enough to cause a bowel obstruction, there may be nausea, vomiting and severe constipation.[5]
Screening and diagnosis
Colorectal polyps can be detected using a faecal occult blood test, flexible sigmoidoscopy, colonoscopy, virtual colonoscopy, digital rectal examination, barium enema or a pill camera.[5]
When does a polyp become a problem?
Malignant potential is associated with
- degree of dysplasia
- Type of polyp (e.g. villous adenoma):
- Tubular Adenoma: 5% risk of cancer
- Tubulovillous adenoma: 20% risk of cancer
- Villous adenoma: 40% risk of cancer
- Size of polyp:
- <1 cm =<1% risk of cancer[citation needed]
- 1 cm=10%risk of cancer[citation needed]
- 2 cm=15%risk of cancer[citation needed]
Normally an adenoma which is greater than 0.5 cm is treated
Treatment
Polyps can be removed during a colonoscopy or sigmoidoscopy using a wire loop that cuts the stalk of the polyp and cauterises it to prevent bleeding.[5] Many "defiant" polyps — large, flat, and otherwise laterally spreading adenomas — may be removed endoscopically by a technique called endoscopic mucosal resection (EMR), which involves injection of fluid underneath the lesion to lift it and thus enable facilitate surgical excision. These techniques may be employed as an alternative to a much-more-invasive colectomy.[6]
Structure
Polyps are either pedunculated (attached to the intestinal wall by a stalk) or sessile (grow directly from the wall).[7]
See also
Polyp table
Additional images
-
Microvesicular hyperplastic polyp. H&E stain.
References
- ^ Santero, Michael; Dennis Lee (2005-03-25). "Colon polyp symptoms, diagnosis and treatment". MedicineNet.com. http://www.medicinenet.com/colon_polyps/article.htm. Retrieved 2007-10-25.
- ^ a b c Lehrer, Jenifer K. (2006-07-25). "Colorectal polyps". MedlinePlus. http://www.nlm.nih.gov/medlineplus/ency/article/000266.htm. Retrieved 2007-10-25.
- ^ a b c d e f Kumar, Vinay (2010). "17 - Polyps". Robbins and Cotran pathologic basis of disease. (8th ed. ed.). Philadelphia, PA: Saunders/Elsevier. ISBN 978-1416031215. http://www.mdconsult.com/books/page.do?eid=4-u1.0-B978-1-4377-0792-2..50022-5--cesec238&isbn=978-1-4377-0792-2&uniqId=278090687-4#4-u1.0-B978-1-4377-0792-2..50022-5--f46.
- ^ a b c Stoler, Mark A.; Mills, Stacey E.; Carter, Darryl; Joel K Greenson; Reuter, Victor E. (2009). Sternberg's Diagnostic Surgical Pathology. Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7942-1.
- ^ a b c d "Colon polyps". Mayo Clinic. 2007-07-16. http://www.mayoclinic.com/health/colon-polyps/DS00511/DSECTION=1. Retrieved 2007-10-25.
- ^ "How I Do It" — Removing large or sessile colonic polyps. Dr. Brian Saunders MD FRCP; St. Mark’s Academic Institute; Harrow, Middlesex, UK. Retrieved April 9, 2008.
- ^ Classen, Meinhard; G. N. J. Tytgat, Charles J. Lightdale (2002). Gastroenterological Endoscopy. Thieme. pp. 303. ISBN 1588900134. http://www.google.co.uk/books?id=sp0istaUg1AC&pg=PA314&d.
External links
- "How I Do It" — Removing large or sessile colonic polyps. Dr. Brian Saunders MD FRCP; St. Mark’s Academic Institute; Harrow, Middlesex, UK. Retrieved April 9, 2008.
- http://www.netdoctor.co.uk/diseases/facts/colonpolyps.htm
- http://www.clevelandclinic.org/registries/inherited/jp.htm
Tumors: digestive system neoplasia (C15–C26/D12–D13, 150–159/211) GI tract Upper GI tractGastric carcinoma · Signet ring cell carcinoma · Gastric lymphoma (MALT lymphoma) · Linitis plasticaUpper and/or lowerAccessory exocrine pancreas: Adenocarcinoma · Pancreatic ductal carcinoma
cystic neoplasms: Serous microcystic adenoma · Intraductal papillary mucinous neoplasm · Mucinous cystic neoplasm · Solid pseudopapillary neoplasm
PancreatoblastomaPeritoneum Categories:- Digestive system neoplasia
- Gross pathology
- Colon (anatomy)
Wikimedia Foundation. 2010.