- De Vivo disease
-
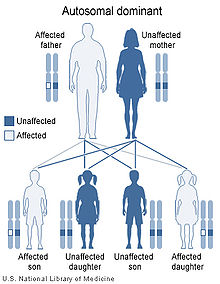
De Vivo disease Classification and external resources OMIM 606777 De Vivo disease is an autosomal dominant developmental disorder associated with a deficiency of GLUT1 also known as Glucose transporter type 1 deficiency syndrome (Glut1-DS)
Contents
Presentation
De Vivo disease is characterized by deceleration of head growth also known as microcephaly, mental and motor developmental delays, infantile seizures refractory to anticonvulsants, ataxia, dystonia, dysarthria, opsoclonus, spasticity, and other paroxysmal neurologic phenomena. Mothers of infants with this disorder usually have uneventful pregnancies and deliveries, with the child appearing normal and with in typical birth weight and length ranges. Infants with GLUT1 deficiency syndrome have a normal head size at birth, but the growth of the brain and skull is slow, in severe cases resulting in an abnormally small head size.[1] Typically, seizures start between one and four months in 90% of cases with abnormal eye movements and apneic episodes preceding the onset of seizures in some cases.[2] Seizures usually are complex to begin with and later become more generalized. Seizure frequency is variable and a history of decreasing frequency during times of ketosis may prompt a diagnosis. Developmental delays are often global and include receptive and expressive language dysfunction.
Genetics
The gene that is involved in this disorder, SLC2A1, provides the code that produces the protein known as the glucose transporter protein type 1. This protein is used in transporting glucose across the blood-brain barrier.
Effects
The disease causes infantile seizures refractory to anticonvulsive drugs, developmental delay, acquired microcephaly and neurologic manifestations including spasticity, hypotonia, and ataxia. [3]
Diagnosis and treatment
De Vivo is diagnosed with CSF glucose value, (<2.2 mmol/L), or lowered CSF/plasma glucose ratio (<0.4), erythrocyte 3-O-methyl-d-glucose uptake assay.[2] Once diagnosed, a Ketogenic diet is usually recommended as it helps to control seizures by providing ketones as an alternative fuel source for the brain other than glucose.[4]
Seeing that the ketogenic diet was discovered as a way to reduce seizures long before 1991 when De Vivo was first diagnosed, it is speculated that some of the ketogentic diet's success was because the children who experienced success on the diet actually had De Vivo at a time when the disease was not yet understood. Less thatn 100 cases have been identified since it's discovery.[1]
References
- ^ a b "GLUT1 deficiency syndrome". Genetics Home Reference. http://ghr.nlm.nih.gov/condition/glut1-deficiency-syndrome. Retrieved 10 October 2011.
- ^ a b Wang, Pascual, Vivo. "Glucose Transporter Type 1 Deficiency Syndrome". Gene Reviews.
- ^ "[GLUT-1 deficiency syndrome or De Vivo disease: a case report"]. PubMed. http://www.ncbi.nlm.nih.gov/pubmed/18556184. Retrieved 12 October 2011.
- ^ De Vivo DC, Trifiletti RR, Jacobson RI, Ronen GM, Behmand RA, Harik SI (1991). "Defective glucose transport across the blood-brain barrier as a cause of persistent hypoglycorrhachia, seizures, and developmental delay". N. Engl. J. Med. 325 (10): 703–709. doi:10.1056/NEJM199109053251006. PMID 1714544.
External links
- GeneReview/NIH/UW entry on Glucose Transporter Type 1 Deficiency Syndrome
- The Colleen Giblin Research Laboratories for Pediatric Neurology
Genetic disorder, membrane: Solute carrier disorders 1-10 SLC1A3 (Episodic ataxia 6) · SLC2A1 (De Vivo disease) · SLC2A5 (Fructose malabsorption) · SLC2A10 (Arterial tortuosity syndrome) · SLC3A1 (Cystinuria) · SLC4A1 (Hereditary spherocytosis 4/Hereditary elliptocytosis 4) · SLC4A11 (Congenital endothelial dystrophy type 2, Fuchs' dystrophy 4) · SLC5A1 (Glucose-galactose malabsorption) · SLC5A2 (Renal glycosuria) · SLC5A5 (Thyroid dyshormonogenesis type 1) · SLC6A19 (Hartnup disease) · SLC7A7 (Lysinuric protein intolerance) · SLC7A9 (Cystinuria)11-20 SLC11A1 (Crohn's disease) · SLC12A3 (Gitelman syndrome) · SLC16A1 (HHF7) · SLC16A2 (Allan–Herndon–Dudley syndrome) · SLC17A5 (Salla disease) · SLC17A8 (DFNA25)21-40 see also solute carrier family
B structural (perx, skel, cili, mito, nucl, sclr) · DNA/RNA/protein synthesis (drep, trfc, tscr, tltn) · membrane (icha, slcr, atpa, abct, othr) · transduction (iter, csrc, itra), trfkCategories:- Autosomal dominant disorders
- Neurological disorders
- Membrane transport protein disorders
- Genetic disorder stubs
Wikimedia Foundation. 2010.