- Cutaneous leishmaniasis
-
Cutaneous leishmaniasis Classification and external resources ICD-10 B55.1 ICD-9 085.1-085.4 DiseasesDB 3266 29171 MeSH D016773 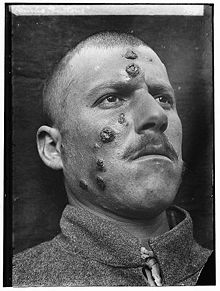 A 1917 case of Cutaneous Leishmaniasis in the Middle East, known then locally as "Jericho Buttons" for the frequency of cases near the ancient city of Jericho.
A 1917 case of Cutaneous Leishmaniasis in the Middle East, known then locally as "Jericho Buttons" for the frequency of cases near the ancient city of Jericho.
Cutaneous leishmaniasis (also known as "Aleppo boil," "Baghdad boil," "Bay sore," "Biskra button," "Chiclero ulcer," "Delhi boil," "Kandahar sore," "Lahore sore," "Leishmaniasis tropica," "Oriental sore," "Pian bois," and "Uta"[1]:423) is the most common form of leishmaniasis. It is a skin infection caused by a single-celled parasite that is transmitted by sandfly bites. There are about 20 species of Leishmania that may cause cutaneous leishmaniasis.
Contents
Signs and symptoms
Post kala-azar dermal leishmaniasis
Main article: Post-kala-azar dermal leishmaniasisPost kala-azar dermal leishmaniasis (PKDL) is a recurrence of Kala-azar that may appear on the skin of affected individuals up to 20 years after being partially treated, untreated or even in those considered adequately treated.[2][3] In Sudan they can be demonstrated in up to 60% of treated cases. They manifest as hypo-pigmented macules, papules, nodules, or facial erythema. Though any organism causing Kala-azar can lead to PKDL, it is commonly associated with L. donovani which gives different disease patterns in India and Sudan. In the Indian variant, nodules enlarge with time and form plaques but rarely ulcerate, but nodules from the African variety often ulcerate as they progress. Nerve involvement is common in African variety but rare in Indian subcontinent.[4] Histology demonstrates a mixture of chronic inflammatory cells; there can be macrophage or epitheloid granuloma.[5] Parasite concentration is not consistent among studies, perhaps reflecting low sensitivity of diagnostic methods used in earlier entries.
Current approach to diagnosis involves 1. demonstration of parasite by microscopy, in vitro culture or animal inoculation; 2. immuno-diagnosis of parasite antigen; 3. detection of parasite DNA in tissue. Newer PCR based tools have higher sensitivity and specificity. Emergence of PKLD has been reported in HIV affected individuals [6] and may become a problem in future.
Sodium stibogluconate (SSG) alone or in combination with rifampicin is used for the treatment of PKLD for a long course of up to 4 months. Compliance can be an issue for such a long course.
Mucocutaneous leishmaniasis
Mucocutaneous leishmaniasis is the most feared form of cutaneous leishmaniasis because it produces destructive and disfiguring lesions of the face. It is most often caused by Leishmania (Viannia) braziliensis, but cases caused by L. aethiopica have also been rarely described.
Mucocutaneous leishmaniasis is treated with long courses (e.g. 30 days) of pentavalent antimonials in a high dose (20 mg/kg). This may fail to cure up to 42% of patients.[7] Even in those patients who achieve an apparent cure, as many as 19% will relapse.[8] Several drug combinations with immunomodulators have been tested, for example, a combination of pentoxifylline (inhibitor of TNF-α) and a pentavalent antimonial at a high-dose for 30 days in a small-scale (23 patients) randomised placebo-controlled study from Brazil achieved cure rates of 90% and reduced time to cure,[9] a result that should be interpreted cautiously in light of inherent limitations of small-scale studies.[10] In an earlier small-scale (12 patients) study, addition of imiquimod showed promising results[11] which need yet to be confirmed in larger trials.
Pathophysiology
Promastigotes of leishmania are transmitted to human skin by the bite of a sandfly. Leishmania then invades human macrophages and replicates intracellularly.
A raised, red lesion develops at the site of the bite (often weeks or sometimes years afterwards). The lesion then ulcerates and may become secondarily infected with bacteria. In many species (for example, L. major) the lesion often spontaneously heals with atrophic scarring. In some species (for example, L. viannia braziliensis) the lesion may spontaneously heal with scarring, but then re-appear elsewhere (especially as destructive mucocutaneous lesions). Lesions of other leishmania species may spontaneously heal and then re-appear as satellite lesions around the site of the original lesion, or along the route of lymphatic drainage.
Some species tend to cause cutaneous leishmaniasis (e.g., L. major and L.tropica), whereas some species tend to cause visceral leishmaniasis (e.g., L. infantum and L donovani), though emerging research (due to high deployment rates of western countries to indigenous areas) is showing these species specific presentation lines are blurring[citation needed].
Diagnosis
Diagnosis is based on the characteristic appearance of non-healing raised, scaling lesions that may ulcerate and become secondarily infected with organisms such as Staphylococcus aureus, in someone who has returned from an endemic area. The gold standard for diagnosis is PCR.[12]
Treatment
The evidence for optimal treatment of cutaneous leishmaniasis is patchy. Treatments that work for one species of leishmania may not work for another; it is recommended that advice of a tropical medicine or geographical medicine specialist be sought. Ideally, every effort should be made to establish the species of leishmania by molecular techniques (PCR) prior to starting treatment. In the setting of a developing country, there is often only one species present in a particular locality, so it is usually unnecessary to speciate every infection. Unfortunately, leishmaniasis is an orphan disease, and almost all the current treatment options are toxic with significant side-effects.
- Leishmania major
- L. major infections are usually considered to heal spontaneously and do not require treatment, but there have been several reports of severe cases caused by L. major in Afghanistan. In Saudi Arabia, a six-week course of oral fluconazole 200 mg daily has been reported to speed up healing.[13]
- Leishmania (Viannia) braziliensis
- Treatment with pentavalent antimonials or amphotericin is mandatory, because of the risk of developing disfiguring mucocutaneous lesions.
- Leishmania infantum
- L. infantum causes cutaneous leishmaniasis in southern France.[14]
New treatment options are arising from the new oral drug Miltefosine (Impavido) which has shown in several clinical trials to be very efficient and safe in visceral and cutaneous leishmaniasis. Recent studies from Bolivia show a high cure rate for mucocutaneous leishmaniasis. Comparative studies against pentavalent antimonials in Iran and Pakistan are also beginning to show a high cure rate for L.major and L.tropica. It is registered in many countries of Latin America (e.g., Colombia), as well in Germany, the home country of its developer Zentaris GmbH. In October 2006 it received orphan drug status from the US Food and Drug administration. The drug is generally better tolerated than other drugs. Main side effects are gastrointestinal disturbances in the 1–2 days of treatment which does not affect the efficacy.
Secondary bacterial infection (especially with Staphylococcus aureus) is common and may require antibiotics. Clinicians who are unfamiliar with cutaneous leishmaniasis may mistake the lesion for a pure bacterial infection (especially after isolation of S. aureus from bacterial skin swabs) and fail to consider the possibility of leishmaniasis.
Epidemiology
Cutaneous leishmaniasis is endemic to many parts of the world. Around twenty different species of Leishmania parasite are capable of infecting humans. The distribution of cutaneous leishmaniasis is very tightly linked to geography and villages even 15 miles apart can have very different rates of cutaneous leishmaniasis.
Some Leishmania species are closely linked to humans and are therefore found in cities (e.g., L. tropica), whereas some are more traditionally associated with animal species and are therefore considered zoonoses (e.g., L. major). Some species that are traditionally considered zoonotic (e.g., L. panamensis) may be becoming primarily human diseases.[15]
Cutaneous leishmaniasis has been occurring in troops coming back from Afghanistan.[16]
See also
- List of cutaneous conditions
- Diffuse cutaneous leishmaniasis
- Leishmaniasis
- Phlebotominae
References
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ Banerjee N (1973). "Role of I.M.A. during natural calamities and national emergencies". Journal of the Indian Medical Association 61 (11): 477–81. PMID 4600129.
- ^ Rathi SK, Pandhi RK, Chopra P, Khanna N (2005). "Post-kala-azar dermal leishmaniasis: a histopathological study". Indian journal of dermatology, venereology and leprology 71 (4): 250–3. doi:10.4103/0378-6323.16616. PMID 16394433.
- ^ Salotra P, Singh R (2006). "Challenges in the diagnosis of post kala-azar dermal leishmaniasis". Indian J. Med. Res. 123 (3): 295–310. PMID 16778312.
- ^ Singh N, Ramesh V, Arora VK, Bhatia A, Kubba A, Ramam M (1998). "Nodular post-kala-azar dermal leishmaniasis: a distinct histopathological entity". J. Cutan. Pathol. 25 (2): 95–9. doi:10.1111/j.1600-0560.1998.tb01696.x. PMID 9521498.
- ^ Stark D, Pett S, Marriott D, Harkness J (2006). "Post-kala-azar dermal leishmaniasis due to Leishmania infantum in a human immunodeficiency virus type 1-infected patient". J. Clin. Microbiol. 44 (3): 1178–80. doi:10.1128/JCM.44.3.1178-1180.2006. PMC 1393159. PMID 16517925. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1393159.
- ^ Franke ED, Wignall FS, Cruz ME, et al. (1990). "Efficacy and toxicity of sodium stibogluconate for mucosal leishmaniasis". Ann Intern Med 113 (12): 934–40. PMID 2173461.
- ^ Netto EM, Marsden PD, Llanos-Cuentas EA, et al. (1990). "Long-term follow-up of patients with Leishmania (Viannia) braziliensis infection and treated with glucantime". Trans R Soc Trop Med Hyg 84 (3): 367–70. doi:10.1016/0035-9203(90)90321-5. PMID 2260171.
- ^ Machado PRL, Lessa H, Lessa M,et al. (2007). "Oral pentoxifylline combined with pentavalent antimony: A randomized trial for mucosal leishmaniasis". Clin Infect Dis 44 (6): 788–93. doi:10.1086/511643. PMID 17304449. http://cid.oxfordjournals.org/content/44/6/788.full.
- ^ Ojha R.P.et al.; Cervantes, D; Fischbach, LA (2007). "Oral pentoxifylline and pentavalent antimony for treatment of leishmaniasis: promising but inconclusive evidence of superiority, compared with antimony monotherapy". Clin. Infect. Dis. 45 (8): 1104. doi:10.1086/521938. PMID 17879933.
- ^ Arevalo I. et al. (2001). "Successful treatment of drug-resistant cutaneous leishmaniasis in humans by use of imiquimod, an immunomodulator". Clin. Infect. Dis. 33 (11): 1847–51. doi:10.1086/324161. PMID 11692295.
- ^ Reithinger R & Dujardin J-C (2007). "Molecular diagnosis of leishmaniasis: current status and future applications". J Clin Microbiol 45 (1): 21–25. doi:10.1128/JCM.02029-06. PMC 1828971. PMID 17093038. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1828971.
- ^ Alrajhi AA, Ibrahim EA, De Vol EB, et al. (2002). "Fluconazole for the treatment of cutaneous leishmaniasis caused by Leishmania major". N Engl J Med 346 (12): 891–95. doi:10.1056/NEJMoa011882. PMID 11907288. http://content.nejm.org/cgi/content/abstract/346/12/891.
- ^ Pratlong F. et al. (2004). "Isoenzymatic analysis of 712 strains of Leishmania infantum in the south of France and relationship of enzymatic polymorphism to clinical and epidemiological features". Journal of Clinical Microbiology 42 (9): 4077–82. doi:10.1128/jcm.42.9.4077-4082.2004. PMC 516332. PMID 15364993. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=516332.
- ^ Vergel C, Palacios R, Cadena H, et al. (2006). "Evidence for Leishmania (Viannia) parasites in the skin and blood of patients before and after treatment". J Infect Dis 194 (4): 503–511. doi:10.1086/505583. PMID 16845635.
- ^ "Canadian soldiers bring back Old World disease". http://www.medicalpost.com/therapeutics/dermatology/article.jsp?content=20090715_153109_1272.
Infectious diseases – Parasitic disease: protozoan infection: Excavata (A06–A07, B55–B57, 007, 085–086) Discicristata TrypanosomatidaLeishmania major/L. mexicana/L. aethiopica/L. tropica (Cutaneous leishmaniasis) · L. braziliensis (Mucocutaneous leishmaniasis) · L. donovani/infantum (Visceral leishmaniasis)SchizopyrenidaTrichozoa TrichomonadidaCategories:- Parasitic infestations, stings, and bites of the skin
Wikimedia Foundation. 2010.


