- Dubin–Johnson syndrome
-
Dubin-Johnson syndrome Classification and external resources 
BilirubinICD-10 E80.6 ICD-9 277.4 OMIM 237500 DiseasesDB 3982 eMedicine med/588 MeSH D007566 Dubin–Johnson syndrome is an autosomal recessive disorder that causes an increase of conjugated bilirubin in the serum without elevation of liver enzymes (ALT, AST). This condition is associated with a defect in the ability of hepatocytes to secrete conjugated bilirubin into the bile, and is similar to Rotor syndrome. It is usually asymptomatic but may be diagnosed in early infancy based on laboratory tests.
Contents
Pathophysiology
The conjugated hyperbilirubinemia is a result of defective endogenous and exogenous transfer of anionic conjugates from hepatocytes into the bile.[1] Pigment deposition in lysosomes causes the liver to turn black.
Diagnosis
A hallmark of DJS is the unusual ratio between the byproducts of heme biosynthesis.
- Unaffected subjects have a coproporphyrin III to coproporphyrin I ratio of approximately 3-4:1.
- In patients with DJS, this ratio is inverted with coproporphyrin I being 3-4x higher than coproporphyrin III. Analysis of urine porphyrins show a normal level of coproporphyrin but the I isomer accounts for 80% of the total (normally 25%).
In post-mortem autopsy, the liver will have a dark pink or black appearance due to pigment accumulation.
There is plenty of canalicular multi-drug resistant protein that causes bilirubin transfer to bile canaliculi. An isoform of this protein is localized to the apical hepatocyte membrane, allowing transport of glucuronide and glutathione conjugates back into the blood.
High levels of gamma-glutamyl transferase (GGT) help in diagnosing pathologies involving biliary obstruction.
Genetics
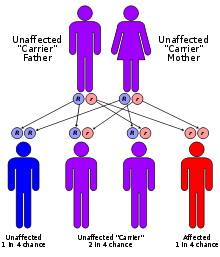
DJS is due to a defect in the multispecific anion transporter (cMOAT) gene (ABC transporter superfamily). It is an autosomal recessive disease and is likely due to a loss of function mutation, since the mutation affects the cytoplasmic / binding domain.
Prognosis
Prognosis is good, and treatment of this syndrome is usually unnecessary. Most patients are asymptomatic and have normal life spans.[1] Some neonates will present with cholestasis.[1] Hormonal contraceptives and pregnancy may lead to overt jaundice and icterus (yellowing of the eyes and skin).
References
- ^ a b c Suzanne M Carter, MS Dubin-Johnson Syndrome at eMedicine
See also
- Dubin-Johnson syndrome at NIH's Office of Rare Diseases
- Jaundice
- Gilbert syndrome
- Crigler-Najjar syndrome
- Rotor syndrome
Heme metabolism disorders (E80, 277.1, 277.4) Porphyria,
hepatic and erythropoietic
(porphyrin)Hereditary hyperbilirubinemia
(bilirubin)conjugated: Dubin–Johnson syndrome · Rotor syndromeGenetic disorder, membrane: ABC-transporter disorders ABCA ABCA1 (Tangier disease) · ABCA3 (Surfactant metabolism dysfunction 3) · ABCA4 (Stargardt disease 1, Retinitis pigmentosa 19) · ABCA12 (Harlequin-type ichthyosis, Lamellar ichthyosis 2)ABCB ABCC ABCC2 (Dubin–Johnson syndrome) · ABCC6 (Pseudoxanthoma elasticum) · ABCC7 (Cystic fibrosis) · ABCC8 (HHF1, TNDM2) · ABCC9 (Dilated cardiomyopathy 1O)ABCD ABCG Categories:- Accessory digestive gland disorders
- Hepatology
- Syndromes
- Membrane transport protein disorders
- Autosomal recessive disorders
- Heme metabolism disorders
Wikimedia Foundation. 2010.